Translate this page into:
Utility of Platelet Function Testing in Cardiac Surgery in 2021
Klaus Görlinger, MD Department of Anaesthesiology and Intensive Care Medicine University Hospital Essen, University Duisburg-Essen, Essen Germany kgoerlinger@ilww.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
In this issue of the Journal of Cardiac Critical Care, Sharan et al and Datta et al are reporting on perioperative and peri-interventional platelet function testing in an attempt to implement personalized antiplatelet therapy in India.1, 2
Sharan et al demonstrated that algorithm-based point-of-care thromboelastometry (ROTEM delta) combined with whole blood aggregometry (ROTEM platelet) helped to guide hemostatic interventions in the intra- and postoperative period of cardiac surgery.1On the one hand, this can avoid inappropriate blood transfusion, and on the other hand, excessive bleeding during and after cardiac surgery.3, 4 Both bleeding and transfusion are associated with worse patient outcomes.5 Here, whole blood impedance aggregometry (multiplate or ROTEM platelet) has been shown to be a valuable tool to assess platelet function before, during, and after cardiovascular surgery as well as during extracorporeal membrane oxygenation (ECMO).6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 This applies for pediatric cardiac surgery and ECMO too (Fig. 1 and Table 1).21, 22, 23 Furthermore, platelet function testing has been shown to predict patients’ outcome in trauma, bacterial sepsis, and COVID-19.24, 25, 26 In contrast to drug monitoring of aspirin and P2Y12-receptor inhibitors with arachidonic acid (ASPI test or ARATEM) and adenosine diphosphate (ADP; ADP test or ADP test) activated assays, platelet dysfunction due to diseases (e.g., trauma, cirrhosis, and sepsis) and devices (e.g., cardiopulmonary bypass, ECMO and dialysis) seem to affect predominantly the ADP- and thrombin-pathway (TRAP test or TRAPTEM activated by thrombin-receptor activating peptide 6; TRAP6). Here, a drop in platelet function has to be considered as a biomarker for worse outcome and not as trigger for platelet transfusion. Accordingly, Sharan et al demonstrated that a significant drop in platelet function from postprotamine to 48 hours after surgery in the ICU was associated with adverse fatal outcome, with an area under the aggregation curve (AUC) threshold value for TRAPTEM, ADPTEM and ARATEM of 53, 43 and 49.5 Ω·min, respectively.1 This is in line with the results reported by Yassen et al, in that a significant decrease in TRAPTEM AUC between postoperative day 14 and 21 after liver transplantation is associated with increased 3-month nonsurvival.27 On the other hand, increased aspirin resistance after cardiac surgery can be associated with ischemic events. This increase aspirin resistance seems to be mediated by an increased turnover of platelets after cardiac surgery rather than due to a pharmacologic aspirin resistance. Therefore, a switch to dual antiplatelet therapy should be considered in patients with postoperative aspirin resistance to avoid ischemic events.28, 29
|
Targeted increase in A5FIB (mm) |
Fibrinogen dose (mg/kg body weight) |
Fibrinogen concentrate (mL/kg body weight) |
Cryoprecipitate (mL/kg body weight) |
|---|---|---|---|
|
Fibrinogen dose (g) = targeted increase in A5FIB (mm) × body weight (kg) / 160. Correction factor (140–160 mm · kg · g-1) depends on the actual plasma volume. A5FIB levels of 12 to 16 mm may compensate for low platelet count or function. |
|||
|
2 mm |
12.5 mg/kg bw |
0.6 mL/kg bw |
1 mL/kg bw |
|
4 mm |
25.0 mg/kg bw |
1.2 mL/kg bw |
2 mL/kg bw |
|
6 mm |
37.5 mg/kg bw |
1.9 mL/kg bw |
3 mL/kg bw |
|
8 mm |
50.0 mg/kg bw |
2.5 mL/kg bw |
4 mL/kg bw |
|
10 mm |
62.5 mg/kg bw |
3.1 mL/kg bw |
5 mL/kg bw |
|
12 mm |
75.0 mg/kg bw |
3.8 mL/kg bw |
6 mL/kg bw |
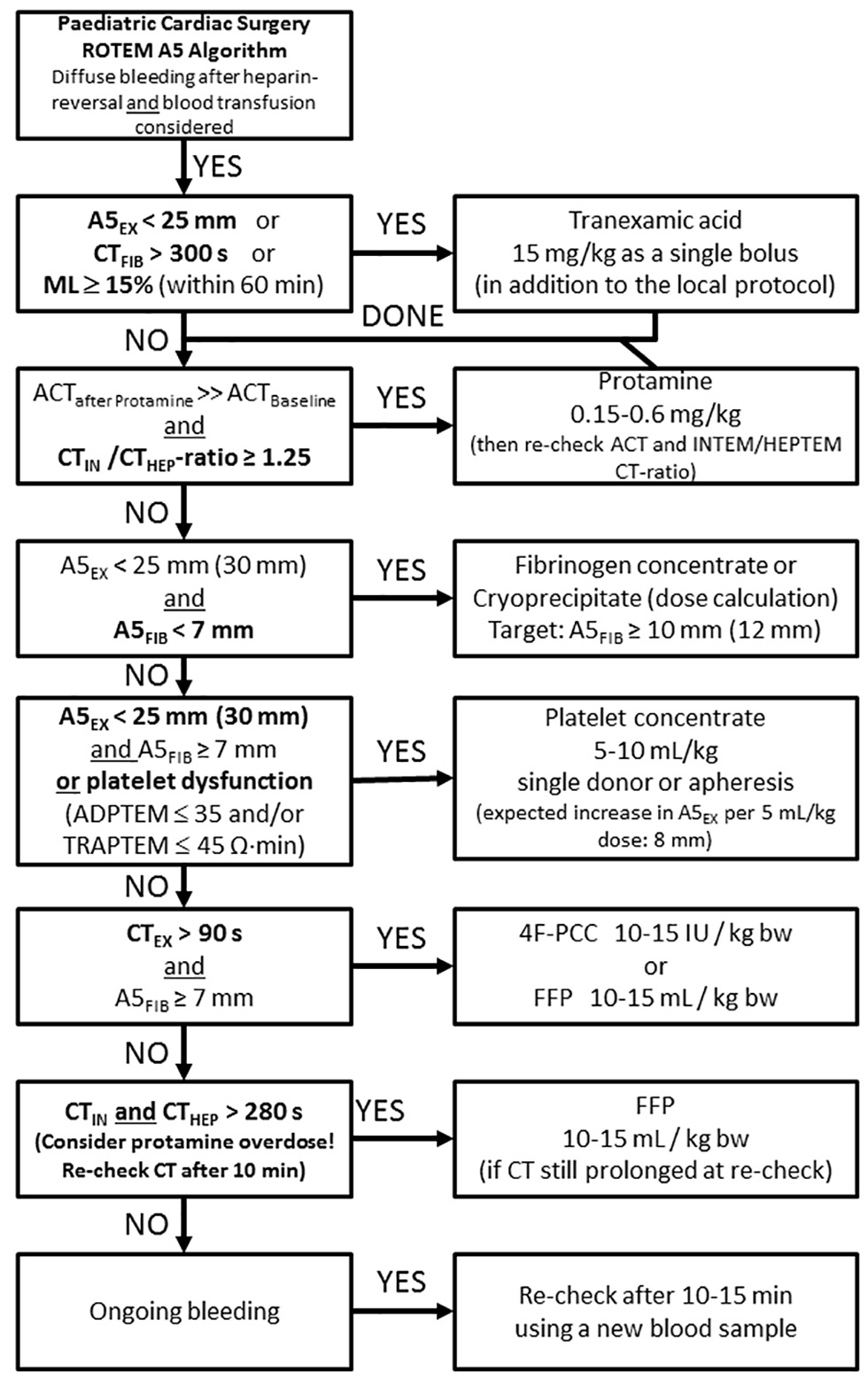
- Evidence-based pediatric cardiac surgery ROTEM A5 algorithm. Abbreviations: 4F-PCC, 4-factor prothrombin complex concentrate; A5EX, EXTEM clot firmness amplitude 5 minutes after CT in mm; A5FIB, FIBTEM clot firmness amplitude 5 minutes after CT in mm; ACT, activated clotting time in seconds; CTFIB, FIBTEM coagulation time in seconds; CTHEP, HEPTEM coagulation time in seconds; CTIN, INTEM coagulation time in seconds; EXTEM, extrinsic ROTEM assay activated by tissue factor and heparin neutralization by polybrene; FFP, fresh frozen plasma; FIBTEM, extrinsic ROTEM assay with platelet inhibition by cytochalasin D and heparin neutralization by polybrene; HEPTEM, intrinsic ROTEM assay with heparin neutralization by heparinase; INTEM, intrinsic ROTEM assay activated by ellagic acid; MCF, maximum clot firmness in mm; ML, EXTEM or FIBTEM maximum lysis in % of MCF; ROTEM, rotational thromboelastometry (Courtesy of Klaus Görlinger, Essen, Germany).
Datta et al reported on the use of thromboelastography platelet mapping for the assessment of individual platelet response secondary to oral antiplatelet therapy after percutaneous coronary interventions as an attempt to implement personalized antiplatelet therapy in India.2 Here, the authors demonstrated that aspirin along with ticagrelor was associated with a higher mean percentage of platelet inhibition and lower high on-treatment platelet reactivity (HPR) as compared with the usage of aspirin combined with clopidogrel or prasugrel. They concluded that platelet function testing may be used effectively to measure the individual response to antiplatelet therapy and personalize antiplatelet therapy for cardiac patients. This is in line with other studies dealing with personalized antiplatelet therapy in cardiology patients.30, 31, 32 In particular, the use of platelet function testing to deescalate antiplatelet therapy and avoid bleeding complications in hyperresponders seems to be a reasonable and promising approach.33, 34 Furthermore, platelet function test might be helpful to determine the optimum timing of elective and urgent coronary artery bypass graft (CABG) surgery after P2Y12 inhibitor cessation, in order to minimize bleeding complications.35, 36, 37, 38, 39, 40, 41, 42
In summary, both platelet function testing studies published in this issue of the Journal of Cardiac Critical Care support the use of peri-interventional and perioperative platelet function testing and highlight its potential to personalize and optimize the management of antiplatelet drugs in terms of precision medicine by implementing the therapeutic window concept.43, 44, 45, 46, 47 This approach is also recommended in European and American guidelines, and the time is ripe to implement personalized antiplatelet therapy and bleeding management as an essential part of patient blood management in India.48, 49, 50
AG is the Associate Director of Clinical Affairs of Werfen India, New Delhi, India.
Conflict of Interest
KG is the Medical Director of Tem Innovations GmbH, Munich, Germany.
References
- Role of platelet function test in predicting postoperative bleeding risk after coronary artery bypass grafting: a prospective observational study. J Card Crit Care TSS 2021
- [CrossRef] [Google Scholar]
- Use of thromboelastography platelet mapping for assessment of individual platelet response secondary to oral antiplatelet therapy after percutaneous coronary intervention: an attempt to start personalized antiplatelet therapy in India. J Card Crit Care TSS 2021
- [CrossRef] [Google Scholar]
- First-line therapy with coagulation factor concentrates combined with point-of-care coagulation testing is associated with decreased allogeneic blood transfusion in cardiovascular surgery: a retrospective, single-center cohort study. Anesthesiology. 2011;115(6):1179-1191.
- [Google Scholar]
- Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology. 2012;117(3):531-547.
- [Google Scholar]
- Major bleeding, transfusions, and anemia: the deadly triad of cardiac surgery. Ann Thorac Surg. 2013;96(2):478-485.
- [Google Scholar]
- Perioperative coagulation management and control of platelet transfusion by point-of-care platelet function analysis. Transfus Med Hemother. 2007;34(6):396-411.
- [Google Scholar]
- The role of point-of-care platelet function testing in predicting postoperative bleeding following cardiac surgery: a systematic review and meta-analysis. Anaesthesia. 2015;70(6):715-731.
- [Google Scholar]
- Bleeding risk assessment in patients undergoing elective cardiac surgery using ROTEM platelet and Multiplate impedance aggregometry. Anaesthesia. 2016;71(6):636-647.
- [Google Scholar]
- Preoperative platelet function predicts perioperative bleeding complications in ticagrelor-treated cardiac surgery patients: a prospective observational study. Br J Anaesth. 2016;117(3):309-315.
- [Google Scholar]
- Postoperative platelet function is associated with severe bleeding in ticagrelor-treated patients. Interact Cardiovasc Thorac Surg. 2019;28(5):709-715.
- [Google Scholar]
- Platelet function after cardiac surgery and its association with severe postoperative bleeding: the PLATFORM study. Platelets. 2019;30(7):908-914.
- [Google Scholar]
- Association among clopidogrel cessation, platelet function, and bleeding in coronary bypass surgery: an observational trial. Thorac Thorac Cardiovasc Surg 2019
- [CrossRef] [Google Scholar]
- Gryfelt G, van der Linden J, Wikman A. Platelet function analysed by ROTEM platelet in cardiac surgery after cardiopulmonary bypass and platelet transfusion. Transfus Med. 2020;30(5):369-376.
- [Google Scholar]
- The association between perioperative point-of-care platelet function analyses and transfusion requirements in cardiac surgery: methodological considerations. Thorac Cardiovasc Surg 2021
- [CrossRef] [Google Scholar]
- Bleeding risk stratification in coronary artery surgery: the should-not-bleed score. J Cardiothorac Surg. 2021;16(1):103.
- [Google Scholar]
- Prospective observational study of hemostatic alterations during adult extracorporeal membrane oxygenation (ECMO) using point-of-care thromboelastometry and platelet aggregometry. J Cardiothorac Vasc Anesth. 2015;29(2):288-296.
- [Google Scholar]
- Predicting transfusion requirements during extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2016;30(3):692-701.
- [Google Scholar]
- Decreased maximum clot firmness in rotational thromboelastometry (ROTEM) is associated with bleeding during extracorporeal mechanical circulatory support. Perfusion. 2016;31(8):625-633.
- [Google Scholar]
- platelet function during extracorporeal membrane oxygenation in adult patients. Front Cardiovasc Med. 2019;6:114.
- [Google Scholar]
- Platelet count and function in paediatric cardiac surgery: a prospective observational study. Br J Anaesth. 2014;113(5):847-854.
- [Google Scholar]
- Perioperative monitoring of platelet function in paediatric cardiac surgery by thromboelastometry, or platelet aggregometry? Br J Anaesth. 2016;116(6):822-828.
- [Google Scholar]
- Evaluation of coagulopathy on veno-arterial ECMO (VA) extracorporeal membrane oxygenation using platelet aggregometry and standard tests: A narrative review. Egyptian J Crit Care Med. 2018;6:73-78.
- [Google Scholar]
- Early TRAP path-way platelet inhibition predicts coagulopathic hemorrhage in trauma. Shock. 2015;43(6):33.
- [Google Scholar]
- Whole blood impedance aggregometry as a biomarker for the diagnosis and prognosis of severe sepsis. Crit Care. 2012;16(5):R204.
- [Google Scholar]
- Coagulation profile of COVID-19 patients admitted to the ICU: An exploratory study. PLoS One. 2020;15(12):243604.
- [Google Scholar]
- et al. A3162: Monitoring of platelet function during and three weeks after adult liver transplantation with ROTEM platelet and conventional coagulation tests. Anesthesiology 2018 Available at: http://www.asaabstracts.com/strands/asaabstracts/abstract.htm?year=2018&index=8&absnum=4522. Accessed July 27, 2021
- Assessment of platelet function by whole blood impedance aggregometry in coronary artery bypass grafting patients on acetylsalicylic acid treatment may prompt a switch to dual antiplatelet therapy. Heart Vessels. 2013;28(1):57-65.
- [Google Scholar]
- Impact of aspirin resistance on outcomes among patients following coronary artery bypass grafting: exploratory analysis from randomized controlled trial (NCT01159639. J Thromb Thrombolysis. 2015;39(4):522-531.
- [Google Scholar]
- The net clinical benefit of personalized antiplatelet therapy in patients undergoing percutaneous coronary intervention. Clin Sci (Lond. 2015;128(2):121-130.
- [Google Scholar]
- Benefits of laboratory personalized antiplatelet therapy in patients undergoing percutaneous coronary intervention: a meta-analysis of randomized controlled trials. Cardiol J. 2018;25(1):128-141.
- [Google Scholar]
- Platelet function test use for patients with coronary artery disease in the early 2020s. J Clin Med. 2020;9(1):194.
- [Google Scholar]
- ADAPT-DES Investigators. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013;382(98/92):614-623.
- [Google Scholar]
- TROPICAL-ACS Investigators. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): a randomised, open-label, multicentre trial. Lancet. 2017;390(10/104):1747-1757.
- [Google Scholar]
- Multiple electrode whole-blood aggregometry and bleeding in cardiac surgery patients receiving thienopyridines. Ann Thorac Surg. 2011;91(1):123-129.
- [Google Scholar]
- Effect of preoperative P2Y12 and thrombin platelet receptor inhibition on bleeding after cardiac surgery. Br J Anaesth. 2014;113(6):970-976.
- [Google Scholar]
- Platelet function recovery after ticagrelor withdrawal in patients awaiting urgent coronary surgery. Eur J Cardiothorac Surg. 2017;51(4):633-637.
- [Google Scholar]
- Platelet function measurement-based strategy to reduce bleeding and waiting time in clopidogrel-treated patients undergoing coronary artery bypass graft surgery: the timing based on platelet function strategy to reduce clopidogrel-associated bleeding related to CABG (TARGET-CABG) study. Circ Cardiovasc Interv. 2012;5(2):261-269.
- [Google Scholar]
- Does platelet reactivity predict bleeding in patients needing urgent coronary artery bypass grafting during dual antiplatelet therapy? Ann Thorac Surg. 2016;102(6):2010-2017.
- [Google Scholar]
- Is there a role for preoperative platelet function testing in patients undergoing cardiac surgery during antiplatelet therapy? Circulation. 2018;138(19):2145-2159.
- [Google Scholar]
- Timing of coronary bypass surgery in patients receiving clopidogrel: the role of VerifyNow. Can J Cardiol. 2016;32(6):724-725.
- [Google Scholar]
- Monitoring platelet reactivity during prasugrel or ticagrelor washout before urgent coronary artery bypass grafting. Coron Artery Dis. 2017;28(6):465-471.
- [Google Scholar]
- Platelet aggregation and its association with stent thrombosis and bleeding in clopidogrel-treated patients: initial evidence of a therapeutic window. J Am Coll Cardiol. 2010;56(4):317-318.
- [Google Scholar]
- Platelet function measurement in elective percutaneous coronary intervention patients: exploring the concept of a P2Y12 inhibitor therapeutic window. JACC Cardiovasc Interv. 2012;5(3):290-292.
- [Google Scholar]
- A pharmacodynamic comparison of a personalized strategy for anti-platelet therapy versus ticagrelor in achieving a therapeutic window. Int J Cardiol. 2015;197:318-325.
- [Google Scholar]
- Development of a concept for a personalized approach in the perioperative antiplatelet therapy administration/discontinuation management based on multiple electrode aggregometry in patients undergoing coronary artery surgery. J Thromb Thrombolysis. 2015;40(3):383-391.
- [Google Scholar]
- The role of evidence-based algorithms for rotational thromboelastometry-guided bleeding management. Korean J Anesthesiol. 2019;72(4):297-322.
- [Google Scholar]
- Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: First update 2016. Eur J Anaesthesiol. 2017;34(6):332-395.
- [Google Scholar]
- Society of Cardiovascular Anesthesiologists Clinical Practice Improvement Advisory for Management of Perioperative Bleeding and Hemostasis in Cardiac Surgery Patients. Anesth Analg. 2019;129(5):1209-1221.
- [Google Scholar]
- Patient blood management in India - Review of current practices and feasibility of applying appropriate standard of care guidelines. A position paper by an interdisciplinary expert group. J Anaesthesiol Clin Pharmacol. 2021;37(1):3-13.
- [Google Scholar]






