Translate this page into:
To Compare the Efficacy of Sub-Pecto-Interfascial Block with Erector Spinae Plane Block in Postoperative Pain Management in Patients Undergoing Cardiac Surgery
*Corresponding author: Rashmi Singh, Department of Cardiac Anaesthesia and Critical Care, All India Institute of Medical Sciences, Delhi, India. rashmisingh5509@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh R, Choudhury A, Chauhan S, Hote M. To Compare the Efficacy of Sub-Pecto-Interfascial Block with Erector Spinae Plane Block in Postoperative Pain Management in Patients Undergoing Cardiac Surgery. J Card Crit Care TSS. 2024;8:101-8. doi: 10.25259/JCCC_69_2023
Abstract
Objectives:
Pain following sternotomy has always been an issue of major concern for anesthesiologists. The incidence of pain is as high as 49% at rest following coronary artery bypass grafting. We planned to utilize the sub-pecto-interfascial plane (SIP) block and erector spinae plane (ESP) block to determine its efficacy and quality of analgesia as compared to conventional intravenous analgesia.
Material and Methods:
After the Institutional Ethics Committee’s approval, we recruited 105 patients and randomized them into three groups. Group 1 received conventional analgesia, group 2 SIP, and group 3 ESP block. Group 2 and Group 3 received allocated blocks after induction of balanced general anesthesia under ultrasound guidance. With high-frequency linear probe (13 MHz) planes identified, a mixture of injection ropivacaine (0.375%) and dexmedetomidine (1.1 mcg/mL) was deposited. In group 2, six injections of 6 mL each at the 2nd, 4th, and 6th intercostal spaces in the bilateral parasternal region. In group 3, two injections of 20 mL of the above-mentioned mixture on each side above the transverse process of the T5 vertebra under the erector spinae muscle plane were injected. All patients were monitored throughout the procedures, and their vitals were recorded. Heart rate, systolic blood pressure, and diastolic blood pressure were noted at baseline, at skin incision, at sternotomy, and 30 min post-extubation. Patients were followed for total fentanyl consumption, pain score (numerical rating scale [NRS] score), and peak inspiratory flow rate, which were noted at extubation and 2, 4, 6, 8, 12, and 24 hours post-extubation. Levels of C-reactive protein (CRP), cortisol, and prolactin were done at baseline and 24 h after surgery. Extubation time, time of first oral intake, and total length of intensive care unit (ICU) stay were also compared between the groups.
Results:
Total fentanyl consumption was significantly lower (P < 0.005) in group 2 and group 3 compared to group 1. Patient receiving blocks were significantly lower NRS score compared to the control group. Spirometry has shown improved results in block groups catering to early discharge from ICU. Rise in levels of CRP, cortisol, and prolactin were much higher in group 1 as compared to group 2 and group 3.
Conclusion:
The application of ESP and SIP blocks is far superior than conventional parenteral analgesics in terms of pain score, total opioid’s consumption, hemodynamic maintenance, spirometry efforts, and length of ICU stays.
Keywords
Sub-pecto-interfascial plane block
Erector spinae plane block
Off-pump coronary artery bypass grafting
Postoperative analgesia
INTRODUCTION
Pain following cardiac surgery is a major issue of concern for all cardiac anesthesiologists. An incidence as high as 27–62% has been reported after coronary artery bypass grafting (CABG) is done through midline sternotomy.[1] The left internal mammary artery (LIMA) harvesting worsens this scenario.[2] Opioids and non-steroidal anti-inflammatory drugs (NSAIDs) remained the two major pillars of postoperative analgesia. Excessive use of NSAIDs is associated with bleeding, various gastrointestinal complications, and acute kidney injury.[3,4] Likewise, tolerance, dependence, and respiratory depression are all well-known complications of opioid use.[5] At present, increased emphasis on fast-tracking and enhanced recovery after surgery (ERAS) necessitates opioid-free multimodal analgesia. Newer, less invasive regional nerve blocks targeting the local nerve supply under ultrasonography (USG) guidance look promising in providing opioid-free analgesia.[6]
De la Torre et al. first described the sub-pecto-interfascial plane (SIP) block for anesthesia for breast surgery.[7] Between the pectoralis major and intercostal muscle, local anesthetic (LA) is infiltrated to target the anterior cutaneous branch of the intercostal nerve. Few case reports have described the applicability of this block to patients with a rib fracture and difficult weaning from a mechanical ventilator[8] and post-sternotomy pain.[9] A recent trial by Zhang et al. has also shown that this block is effective in combating post-sternotomy pain.[10]
Erector spinae block was first practiced by Forero et al. in the successful management of chronic neuropathic pain.[11] It is simple to perform, yet it provides multi-dermatomal coverage targeting ventral and dorsal thoracic rami, resulting in anesthesia of the posterior, lateral, and anterior thoracic walls.
There is limited data presently available on the utility of regional anesthesia in combating post-sternotomy pain. SIP block has been utilized in patients with rib fractures, and one randomized control trial evaluated its role in post-sternotomy pain. So far, it looks promising, but there is a lack of literature. Our objective in this study is to find the efficacy and quality of postoperative analgesia of these novel fascial plane blocks against the conventional intravenous (I.V.) analgesic regimen.
MATERIAL AND METHODS
The Institute Ethics Committee Approval (IECPG-405) was taken. Furthermore, we registered our study with the Clinical Trial Registry of India (CTRI No. 2020/10/028184). Prerecruitment written informed consent was obtained from patients.
Sample size
A study done by Krishna et al. found that total fentanyl consumption in the ESP group and control group was 231.42 ± 50.6 (mean ± standard deviation [SD]) and 935.66 ± 160, respectively.[12] Anticipating a difference of 50 mcg in the total fentanyl consumption between ESP and SIP groups with a combined standard deviation of 50.6, the estimated sample size was calculated to be 29 in each group. Considering some dropouts in the study, 30 patients were chosen in each group (to be on the safer side); thus, the total sample size was 90. The assumed power and alpha levels are 90% and 1%, respectively. The alpha error of 1% was considered as there were three post hoc comparisons to be done (viz., control vs. ESP, control vs. SIP, and ESP vs. SIP).
Between October 2020 and October 2021, a total of 90 subjects were recruited after a stringent patient selection process. Patients were randomized into three groups using a computer-generated random number table. Group 1 is the control group, and no intervention was done in this group. Group 2 was the SIP block, and Group 3 was the erector spinae plane (ESP) block group.
Inclusion criteria
All coronary artery disease (CAD) patients of either sex in the age group of 20–70 years, NYHA I and II, cardiac anesthesia risk evaluation score categories 1 and 2[13] were included in the study. All patients having CAD (either single, double, or triple vessel) with normal left ventricular (LV) function for elective off-pump CABG were included in the study.
Exclusion criteria
Patients undergoing emergency surgery and redo surgery were excluded from the study. Patients with the following conditions were also excluded: Left main CAD, moderate-to-severe LV dysfunction, patients on preoperative inotropic support, patients for re-exploration, patients with low cardiac output syndrome, perioperative intra-aortic balloon pump assistance (any indication), bleeding diathesis or any abnormal coagulation profile, abnormal hepatic and renal parameters, uncontrolled diabetes mellitus, chronic obstructive pulmonary disease, and allergy to LA agent (viz., ropivacaine). Special situations: Those patients who were ventilated for more than 12 hours following the surgery were also excluded from the study.
Pre-operative evaluation
All patients were posted for elective off-pump CABG, and a thorough pre-anesthetic assessment was done on the day before surgery. Relevant history was obtained, and physical and airway examinations were done. All relevant blood investigations, including coagulation profile, Chest X-ray, electrocardiography (ECG), coronary angiogram, and transthoracic echocardiography reports, were reviewed. Preoperatively, an 11-point numeric rating scale (NRS), which was scored from 0 to 10 (0 = no pain to 10 = most intense pain imaginable), was explained to patients. They were also sensitized about Patient-controlled analgesia (PCA) pump operation. As per institutional protocol, all subjects received pre-medications in the form of intramuscular morphine (0.1 mg/kg) and promethazine (0.5 mg/kg).
On the day of surgery
Once patients were inside the operation theater, 5-lead ECG leads, non-invasive blood pressure (BP) cuff, and pulse oximeter were attached, and patients were induced with injection of fentanyl (3–5 mcg/kg) and injection of etomidate (0.3 mg/kg). Injection rocuronium (0.9 mg/kg) was used to facilitate laryngoscopy and endotracheal intubation with an appropriate-size endotracheal tube. Standard institutional protocols were followed for the maintenance of anesthesia. After proper positioning, a central venous catheter and arterial line were secured.
The LA drug reconstituted was as follows – Injection ropivacaine (0.75%) 20 mL was diluted with 19 mL normal saline (NS) and 1 mL of 1 mcg/kg dexmedetomidine in a bowl. The final concentration of 40 mL ropivacaine in the LA mixture was 0.375%.
In group 2, the SIP block was performed under USG guidance by an experienced anesthesiologist. A high-frequency linear ultrasound probe (13 MHz, SonoSite M-Turbo, Bothell, WA, USA) was placed in a parasagittal plane 2 cm lateral to mid-sternum. Different muscle planes, such as pectoralis major, internal intercostal muscle and ribs, and pleura, were located [Figure 1]. The block was initially performed at T5–T6 space and subsequently repositioned to target each rib space up to T1–2 rib space. A total of three needle insertions were performed on each side at T1–T2, T3–T4, and T5–T6. After satisfactory hydrodissection with NS, a total of 36 mL of LA drug mixture was deposited between the pectoralis muscle and internal intercostal muscle at three spaces bilaterally with 6 mL volume in each site.
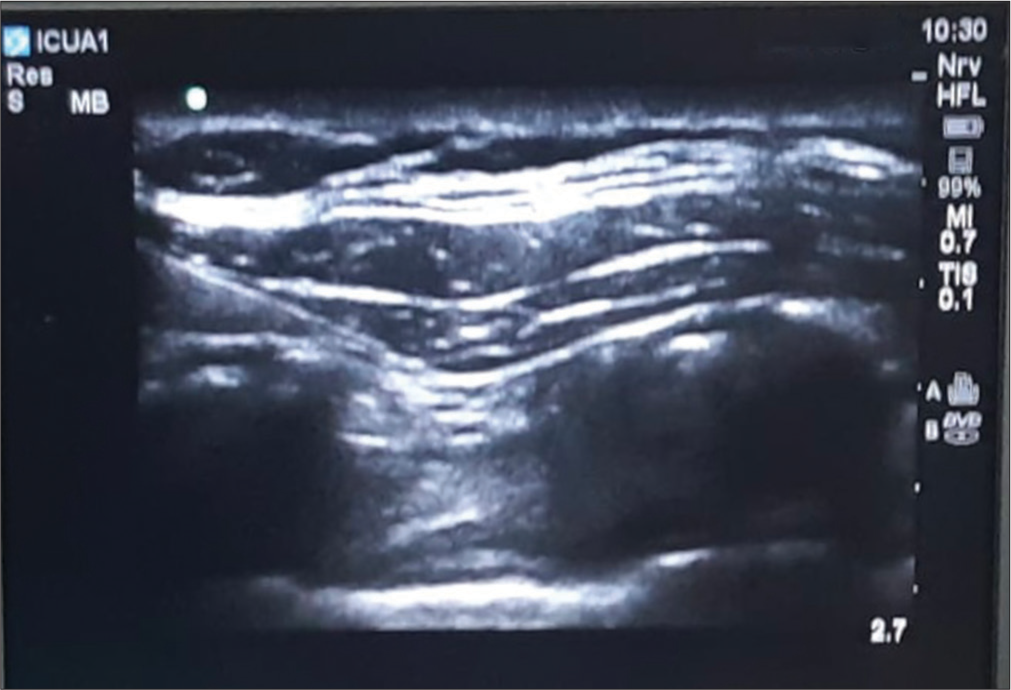
- Sonoanatomy of sub-pecto-interfascial plane block showing position of needle tip below the pectoralis major muscle.
In group 3, the ESP block was also performed under USG guidance. Patients were turned into the left lateral position for the institution of bilateral erector spinae block. A high-frequency linear USG probe (13 MHz, SonoSite M-Turbo, Bothell, WA, USA) was placed 2–3 cm lateral to the T5 spinous process, and all muscle planes, such as the trapezius, rhomboid major, and erector spinae muscle are then identified superficial to the transverse process. In plane approach, in which a block needle is inserted superior to the USG probe from cephalad to caudal, has been used. Once the needle tip is below the erector spinae, a small bolus of NS is injected for an appreciable hydrodissection. After confirmation, 20 mL of 0.375% ropivacaine along with 0.5 µg/kg of dexmedetomidine were injected bilaterally.
In all the groups, heart rate and BPs were monitored at baseline, 5 min after the institution of the block, and 1 and 30 min after sternotomy. CABG surgery was performed through midline sternotomy under transesophageal echocardiography guidance. Total intraoperative consumption of fentanyl was noted. After skin closure, patients were shifted to the cardiothoracic vascular surgery (CTVS)-intensive care unit (ICU).
The control group (i.e., group 1) received an injection of paracetamol 1 g I.V. every six hourly as per institutional protocol. Patients were monitored at extubation and at 2, 4, 6, 8, 12, and 24 hours post-extubation using NRS for pain assessment. Concurrently, spirometry was performed to assess the total number of balls raised in the spirometer, which is a predictor of inspiratory flow rates (1 ball–600 mL, two balls–900 mL, and three balls–1200 mL). All three groups received rescue analgesia through a PCA pump. On the perception of pain, the patient pressed a button on the handheld remote device for self-administering analgesics containing an injection of fentanyl one µg/kg with a PCA pump. The PCA pump was set with a lockout period of 1.5 hours. If NRS is persistently high (>4) even after 30 min of first rescue analgesia, a 2nd rescue analgesia as 0.5 µg/kg of fentanyl was given by the nurse and documented. Pain was classified as mild (NRS 0–4), moderate (5–7), and severe (8–10). Total consumption of fentanyl over 24 h through PCA pump and other modes of rescue analgesia was noted. All patients selected for the study had C-reactive protein (CRP), serum cortisol, and serum prolactin done at two time points. One sample was taken preoperatively, which served as a baseline value, and the other at 24 h post-surgery. The level of these biomarkers was noted at both time points.
Total consumption of IV fentanyl in the first 24 hours postoperatively was the primary outcome of our study. Secondary outcomes were NRS score at extubation and at 2, 4, 6, 8, 12, and 24 hours after extubation. Levels of CRP, cortisol, and prolactin were also noted. Total rescue analgesia received in the post-anesthesia care unit/CTVS-ICU, peak inspiratory flow rate, time to extubation, time to first oral intake, and total length of ICU stay were compared. Any untoward reactions to local anesthetic and any unexpected complications from the nerve blocks were also noted.
Statistical analysis
Stata 14.0 software was used for statistical analysis. Data were presented as numbers (percentages) or mean (SD)/median (min/max) as appropriate. Continuous baseline characteristics were compared between three groups using one-way analysis of variance (ANOVA)/Kruskal–Wallis non-parametric test, and categorical variables were compared using Chi-square test/Fischer’s exact test.
Total fentanyl consumption (a primary outcome measure) in 1st 24 h was compared between three groups using one-way ANOVA followed by post hoc analysis (Bonferroni correction). Pain scores (a secondary outcome measure) for 0, 2, 4, 6, 8, 12, and 24 h were compared among three groups by Kruskal–Wallis non-parametric test. Other secondary outcomes were compared among the three groups using the Kruskal–Wallis non-parametric test. If P < 0.05, this means the results are statistically significant.
RESULTS
A total of 90 patients were included, with 30 patients in each group. Two patients were excluded in group 1 due to delayed extubation (>6 h), three patients were excluded in group 2 due to delayed extubation (n-2) and re-exploration (n-1), and in group 3, four patients were lost to follow-up pertaining to delayed extubation (n-2) and re-exploration (n-3). Hence, for final analysis, there were 28, 27, and 26 patients were available in groups 1, 2, and 3, respectively. Subject distribution and group allocation are outlined in the consort flow diagram [Figure 2].
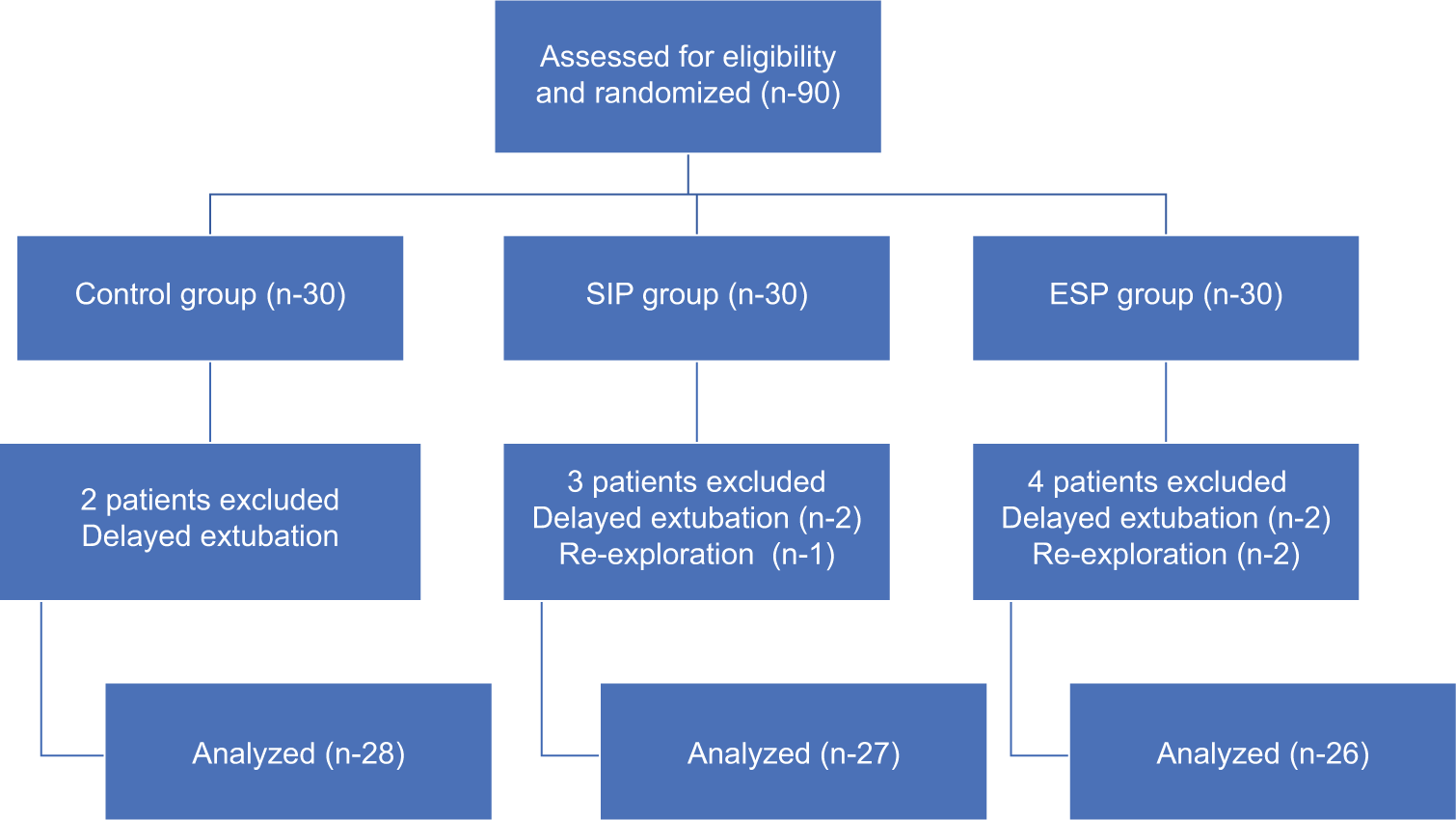
- Consort flow diagram. n: sample size, SIP: Sub-pecto-interfascial plane, ESP: Erector spinae plane.
All the groups were comparable with respect to demographic data [Table 1]. Total intraoperative consumption of fentanyl was compared between the groups, and there was significantly less (P < 0.005) consumption of iv fentanyl in group 2 and group 3 as compared to group 1. Heart rate, systolic, and diastolic pressures were compared between the groups. In the control group, there is a significant increase (P < 0.001) in heart rate and systolic and diastolic BP compared to group 2 and group 3. Institution of fascial plane nerve blocks has resulted in stable hemodynamics even at times of intense stimulation, such as skin incision and sternotomy [Table 2].
| Group 1 (n=30) | Group 2 (n=30) | Group 3 (n=30) | P value | |
|---|---|---|---|---|
| Age (years) | 57.66±8.5 | 59.83±7.17 | 58.5±7.4 | 0.552 |
| Gender distribution Male Female |
27 (90) 3 (10) |
23 (76) 7 (23) |
24 (80) 6 (20) |
0.372 |
| Weight (kg) | 67.6±6.7 | 67.6±7.6 | 69.2±9.9 | 0.686 |
| Height (cm) | 163.9±5.6 | 164.6±8.01 | 165.7±8.5 | 0.659 |
| Body surface area (meter2) | 1.73±0.10 | 1.74±0.13 | 1.76±0.17 | 0.677 |
Data expressed as mean±SD and frequency (%), SD: Standard deviation, kg: Kilogram, cm: Centimeter, n: Sample size.
| Hemodynamic parameters | Group 1 (n-30) (mean±SD) |
Group 2 (n-30) (mean±SD) |
Group 3 (n-30) (mean±SD) |
P value |
|---|---|---|---|---|
| HR | ||||
| Baseline | 70.3±9.04 | 73.3±7.27 | 73±8.09 | <0.001 |
| At skin incision | 81.7±7.86 | 59.8±6.52 | 57.2±6.04 | |
| At sternotomy | 88.0±9.10 | 66.3±8.92 | 62.2±8.35 | |
| 30 min post sternotomy | 81.2±8.23 | 63.7±8.52 | 60.6±7.20 | |
| SBP (mm/hg) | ||||
| Baseline | 124.3±9.74 | 134.0±14.96 | 139.2±12.55 | <0.001 |
| At skin incision | 135.2±8.02 | 106.4±8.74 | 105.2±7.44 | |
| At sternotomy | 143.9±7.15 | 119.5±9.73 | 116.6±8.17 | |
| 30 min post sternotomy | 134.7±9.46 | 114.5±8.68 | 110.1±8.41 | |
| DBP (mm/hg) | ||||
| Baseline | 73.1±9.21 | 84.4±13.04 | 85.8±7.12 | <0.001 |
| At skin incision | 84.2±6.63 | 63.5±9.29 | 66.3±9.29 | |
| At sternotomy | 87.8±7.73 | 70.7±9.36 | 73.8±5.11 | |
| 30 min post sternotomy | 79.5±8.53 | 66.4±10.7 | 66.4±5.60 |
SD: Standard deviation, HR: Heart Rate, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, n: Sample size.
Trends of NRS scores post-extubation are shown in Figure 3, which shows significantly low NRS scores in group 2 and group 3 compared to group 1.
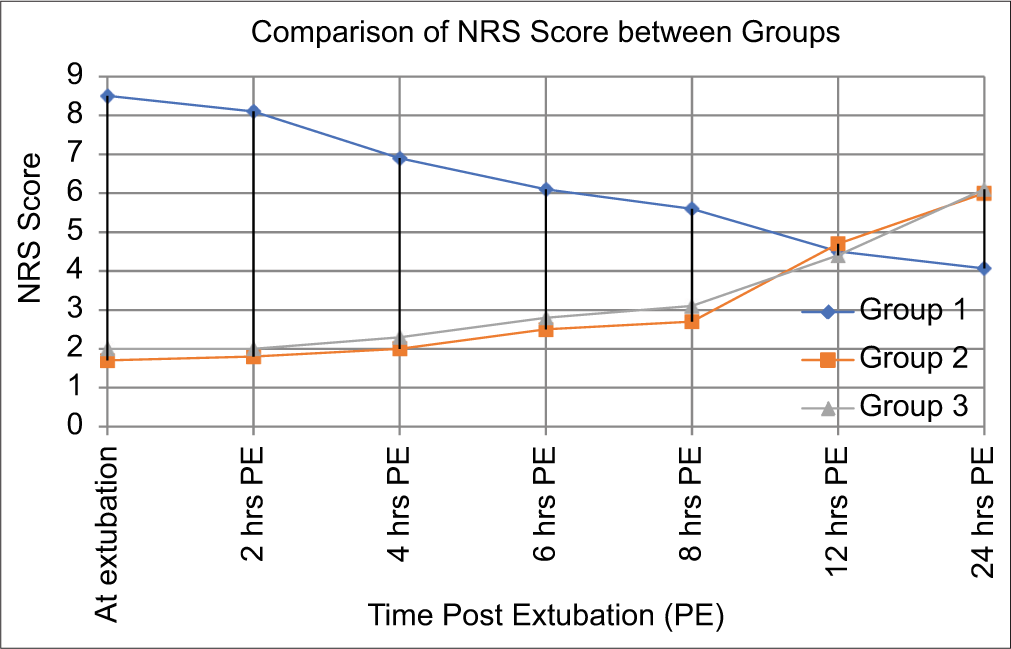
- Trends of NRS score post extubation between the groups. NRS: Numerical rating scale, PE: Post extubation.
The use of rescue analgesia is significantly lowered in group 2 and group 3. None of the patients required rescue analgesia through the PCA pump before extubation, as well as till six hours post-extubation. Consumption of rescue analgesia is significantly less (P < 0.005) in group 2 and group 3 compared to group 1 till eight hours post-extubation as well [Table 3].
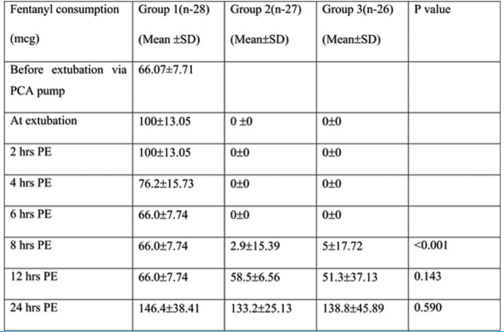 |
PE: Post extubation, SD: Standard deviation, PCA: Patient-controlled analgesia, hrs: Hours.
As far as the incentive spirometry performance is concerned, spirometry efforts were less in group 1, and no patient was able to raise more than one ball up to 6 hours post-extubation. On the contrary, all patients were able to raise two balls (correlating with 900 mL of peak tidal flow) in group 2 immediately after extubation. In group 3, 7.69% of patients were able to raise three balls as well. Spirometry efforts were always higher in group 2 and group 3 as compared to group 1. Although there were no significant differences between the three groups as regards the CRP, cortisol, and prolactin levels at the basal values (P > 0.05), there is a significant rise in their levels in group 1 as compared to baseline [Figures 4 and 5].

- Graph showing trends of cortisol level in all groups. PS: Post surgery.
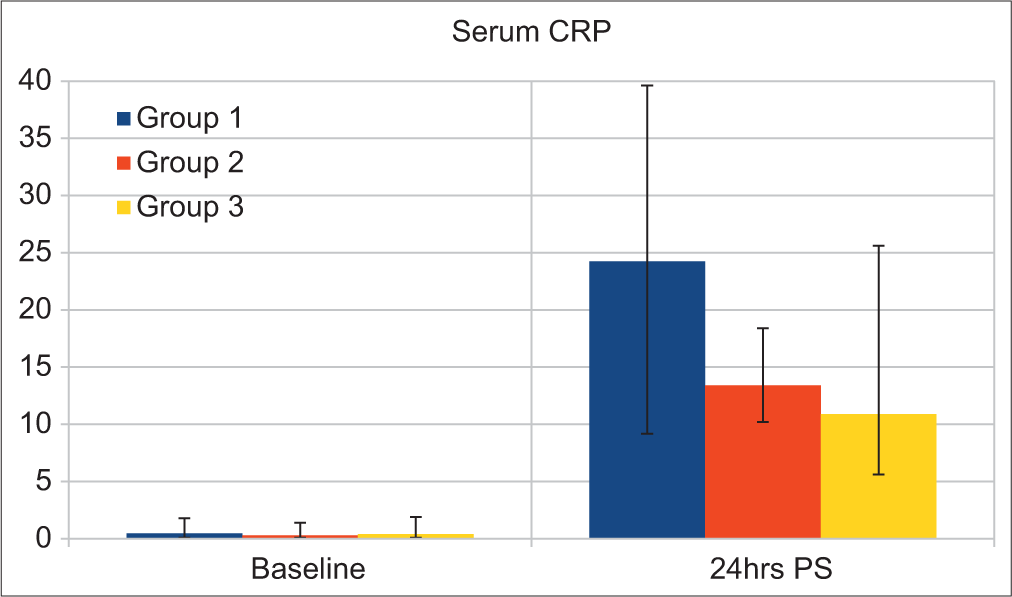
- Graph showing level of CRP in all the groups. CRP: C reactive protein, PS: Post surgery.
Total rescue analgesia and total fentanyl consumption were significantly lower in group 2 and group 3 (P < 0.05). Duration of analgesia in which NRS score <4 is approximately ten h for SIP and ESP block each. Although extubation time is similar in all three groups (as extubation depends on multiple factors other than pain in CAD patients), the total length of ICU stay was significantly lower (P < 0.05) in group 2 and group 3, suggesting their pivotal role in enhanced recovery and early mobilization [Table 4].
| Post-operative variables | Group 1(n-28) mean±SD |
Group 2(n-27) mean±SD |
Group 3(n-26) mean±SD |
P value |
|---|---|---|---|---|
| Total rescue analgesia consumption | 686.96±86.77 | 191.59±45.25 | 195.19±71.53 | <0.001 |
| Total fentanyl consumption | 1411.96±144.66 | 715.66±127.45 | 770.19±109.34 | <0.001 |
| Extubation time ( hrs) | 4.69±0.45 | 4.62±0.65 | 4.34±0.41 | 0.039 |
| Time of first oral intake ( hrs) | 6.66±0.51 | 6.62±0.65 | 6.34±0.41 | 0.070 |
| Total length of ICU stays ( days) | 3.46±0.50 | 2.07±0.26 | 2.11±0.32 | <0.001 |
Hrs: Hours, SD: Standard deviation.
DISCUSSION
Postoperative pain following CABG can be precipitated by sternotomy, LIMA harvesting, extensive tissue retraction, and mobilization or intercostal chest tube insertion.[14] Poor pain control acts as a nidus for postoperative tachycardia, hypertension, and various dysrhythmias, potentially leading to myocardial ischemia. Persistent pain in the postoperative period causes atelectasis, pulmonary infection, difficult weaning, prolonged immobilization, and the development of chronic pain.[15]
The application of regional anesthesia in cardiac surgery has now emerged as a novel as well as an effective way of pain control. Till now, many randomized controlled trials (RCTs) have been done to establish the efficacy of these blocks, but to the best of our knowledge, this is the first RCT comparing ESP and SIP blocks with conventional parenteral analgesia in the setting of off-pump CABG surgery.
As far as the timing of administration of block is concerned, many authors have different opinions. One school of thought is to institute blocks at the completion of the surgery so that an actual assessment of pain-free post-extubation period can be done. Another institution strongly favors regional blocks before the initiation of surgery and noxious stimuli.[16] However, post-surgery, patients are usually on multiple inotropes, and positioning for ESP block can cause hemodynamic instability. Moreover, following sternal closure, the integrity of the target plane for the SIP block may be lost. Considering these logistic issues and the comfort of our patients, we have decided to institute these blocks after induction of general anesthesia.
Krishna et al.[12] have compared bilateral ESP block with conventional analgesia and Zhang et al.[10] have compared SIP block with conventional analgesia in patients undergoing cardiac surgery. Both of them have found significant differences in opioid consumption in their respective study. We have also seen a significant reduction in terms of opioid consumption in both study groups when compared to the control group. For objective measurement of the total fentanyl consumption, PCA pumps were used. Patients can themselves administer pre-determined analgesic doses by pressing a handheld button of the PCA pump on the perception of pain. It gives them higher satisfaction with better pain control. The use of a PCA pump has been shown to improve patient postoperative analgesia and improve NRS score in CABG patients.[17,18]
As far as pain score is concerned, the NRS score was significantly lower in groups 2 and 3 compared to group 1. Again, these results were in consonance with Krishna et al.[12] and Zhang et al.[10] No significant difference between Group 2 and Group 3 was found for the NRS score. The duration of postoperative analgesia was ten hours for the ESP group and ten hours for the SPIF group. Wasfy et al.[14] have demonstrated that ESP when combined with continuous infusion of local anesthetics, 48 h of pain-free duration could be achieved. We applied a single shot block with an adjuvant, so the duration of analgesia was very reasonable.
Due to effective pain relief, patient in group 2 and group 3 has higher peak inspiratory flow rates than group 1. Wasfy et al.[14] have compared bilateral continuous ESP versus multimodal analgesia and found higher peak inspiratory flow rates in the ESP group.
Cardiac surgery causes widespread systemic inflammation through a variety of mechanisms, causing an increase in stress hormones such as cortisol, prolactin, and CRP. Postoperative analgesia has been thought to play a crucial role in the attenuation of these stress markers.[19] Institution of ESP and SIP block successfully attenuated cortisol, prolactin, and CRP levels, thus quantifying the decrease in inflammatory responses after the surgery. We have also shown that the application of these blocks has resulted in early ICU discharge. No complication of these blocks was noted in any of the patients.
ESP is an interfascial plane block in which a local anesthetic is deposited anterior to the erector spinae muscle. Fascia of erector spinae extends from the nuchal fascia cranially to the sacrum caudally, thus explaining the extensive multi-dermatomal spread of the drug. Successful administration of ESP block has been reported in breast surgery,[20] abdominal surgery,[21] and spine fusion.[22] As far as cardiac surgery is concerned, successful application of these blocks in practice in both thoracotomies and sternotomies.[12]
The sternum is innervated by the intercostal nerve, which arises from the thoracic nerve T2–T6. By injecting drugs between the pectoralis muscle and intercostal muscle, SPIF block targets these nerves. For complete coverage from T2 to T6 dermatome, multiple injections are necessary bilaterally along the sternum.
In our study, both ESP and SIP blocks were comparable in terms of duration of analgesia, NRS score, perioperative fentanyl consumption, peak inspiratory flow rate, and level of stress markers. Both the blocks are relatively novel, and ultrasound has made the application of these blocks very convenient. ESP block requires positioning of the patient to a lateral position, which becomes quite cumbersome for cardiac patients with invasive lines in-situ. SIP block can be applied in a supine position; however, for a complete sensory block along the sternum, multiple injections are required. Hence, considering these pros and cons, one can always choose one block over the other for satisfactory postoperative analgesia.
A major limitation of our study is its small sample size. Furthermore, both the blocks were applied after general anesthesia, so sensory assessment of the block could not be performed and the failed block could not be documented. Bilateral block is mandatory for complete analgesia, thereby potentially increasing the local anesthetic toxicity. We have applied a single shot block; if these blocks were combined with continuous infusion, the duration of analgesia would have been increased.
CONCLUSION
Novel interfascial plane blocks such as ESP and SIP blocks are far superior to conventional parenteral analgesia visa-vis objective pain score, total opioid consumption, hemodynamic stability, incentive spirometry efforts, and the length of ICU stay. We could not find the superiority of one block over the other. Therefore, any one of the blocks can be utilized depending on the anesthesiologists’ expertise and individual patient profile.
Ethical approval
The authors declare that they have taken the Institutional Ethical Committee approval and the approval number is IECPG-405.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Pain after Cardiac Surgery: A Prospective Cohort Study of 1-Year Incidence and Intensity. Anesthesiology. 2006;105:794-800.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing the Prevalence of Chronic Pain after Sternotomy in Patients Undergoing Coronary Artery Bypass Grafting Using the Internal Mammary Artery and Other Open Heart Surgeries. Anesth Pain Med. 2014;4:e17969.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of the COX-2 Inhibitors Parecoxib and Valdecoxib after Cardiac Surgery. N Engl J Med. 2005;352:1081-91.
- [CrossRef] [PubMed] [Google Scholar]
- Ibuprofen-a Safe Analgesic During Cardiac Surgery Recovery? A Randomized Controlled Trial. J Cardiovasc Thorac Res. 2015;7:141-8.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of the Anesthesiologist in Fast-track Surgery: From Multimodal Analgesia to Perioperative Medical Care. Anesth Analg. 2007;104:1380-96.
- [CrossRef] [PubMed] [Google Scholar]
- Opioid Free Cardiac Surgery: Opportunities and Obstacles. J Cardiothorac Vasc Anesth. 2020;34:567-8.
- [CrossRef] [PubMed] [Google Scholar]
- A Novel Ultrasound-Guided Block: A Promising Alternative for Breast Analgesia. Aesthet Surg J. 2014;34:198-200.
- [CrossRef] [PubMed] [Google Scholar]
- A New Thoracic Interfascial Plane Block as Anesthesia for Difficult Weaning Due to Ribcage Pain in Critically Ill Patients. Med Intensiva. 2014;38:463-5.
- [CrossRef] [PubMed] [Google Scholar]
- Pecto-intercostal Fascial Block for Acute Poststernotomy Pain: A Case Report. A A Pract 2018. ;. ;10:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Bilateral Pectointercostal Fascial Block for Perioperative Pain Management in Patients Undergoing Open Cardiac Surgery: A Prospective Randomized Study. BMC Anesthesiol. 2021;21:175.
- [CrossRef] [PubMed] [Google Scholar]
- The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med. 2016;41:621-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral Erector Spinae Plane Block for Acute Post-Surgical Pain in Adult Cardiac Surgical Patients: A Randomized Controlled Trial. J Cardiothorac Vasc Anesth. 2019;33:368-75.
- [CrossRef] [PubMed] [Google Scholar]
- The Cardiac Anesthesia Risk Evaluation Score: A Clinically Useful Predictor of Mortality and Morbidity after Cardiac Surgery. Anesthesiology. 2001;94:194-204.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral Continuous Erector Spinae Block Versus Multimodal Intravenous Analgesia in Coronary Bypass Surgery. A Randomized Trial. Egypt J Anaesth. 2021;37:152-8.
- [CrossRef] [Google Scholar]
- Persistent Postsurgical Pain: Pathophysiology and Preventative Pharmacologic Considerations. Anesthesiology. 2018;129:590-607.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral Thoracic Paravertebral Block Combined with General Anesthesia vs. General Anesthesia for Patients Undergoing Off-pump Coronary Artery Bypass Grafting: A Feasibility Study. BMC Anesthesiol. 2019;19:101.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Patient-Controlled Analgesia on Pain Relief after Coronary Artery Bypass Graft Surgery: A Randomized Clinical Trial. J Caring Sci. 2012;1:223-9.
- [Google Scholar]
- Patient-controlled Versus Nurse-controlled Pain Treatment after Coronary Artery Bypass Surgery. Acta Anaesthesiol Scand. 2000;44:43-7.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-Guided Erector Spinae Plane Block Compared to Modified Pectoral Plane Block for Modified Radical Mastectomy Operations. Anesth Essays Res. 2019;13:334-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound Guided Erector Spinae Plane Block Reduces Postoperative Opioid Consumption Following Breast Surgery: A Randomized Controlled Study. J Clin Anesth. 2018;50:65-8.
- [CrossRef] [PubMed] [Google Scholar]
- Erector Spinae Plane Block for Different Laparoscopic Abdominal Surgeries: Case Series. Case Rep Anesthesiol. 2018;2018:3947281.
- [CrossRef] [PubMed] [Google Scholar]
- Opioid-free Analgesia for Posterior Spinal Fusion Surgery Using Erector Spinae Plane (ESP) Blocks in a Multimodal Anesthetic Regimen. Spine (Phila Pa 1976). 2019;44:E379-83.
- [CrossRef] [PubMed] [Google Scholar]






