Translate this page into:
Does Preoperative Plasma Endothelin-1 Level Influences the Postoperative Events in Patients Undergoing Coronary Artery Bypass Grafting (CABG)? Revisiting Endothelin-1 Molecule in CABG Patients
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Endothelin-1 (ET-1) is a powerful physiological vasoconstrictor release in response to endothelial injury. Increased synthesis of endothelin is associated with myocardial ischemia and reperfusion injury. The normal level varies between 0.2 and 18.5 pg/mL that maintains normal vascular homeostasis. We hypothesized that there exists a correlation between ET-1 and clinical outcome in patient undergoing elective coronary artery bypass grafting (CABG) surgery under cardiopulmonary bypass.
Fifty-eight patients undergoing elective on-pump CABG were enrolled in the study. Blood sample for plasma ET-1 was taken before anesthesia induction. The median ET-1 level was 5 pg/mL (range: 0.6–30.33 pg/mL). The inotropic and intraaortic balloon pump requirement was significantly higher among patients having baseline ET-1 level more than 14.24pg/mL (p = 0.001in each case). A similar finding was observed in the duration of mechanical ventilation, intensive care unit stay, and duration of hospital stay (r = 0.68, p = 0.000; r = 0.58, p = 0.000; and r = 0.61, p = 0.000 respectively). The occurrence of complications was also more in individuals with higher baseline ET-1 level. The p-value was significant for occurrence infection, arrhythmia, renal and respiratory problems as observed in postoperative period by using Mann–Whitney U test.
This study concludes that higher level of preoperative ET-1 levels correlates well to adverse clinical outcome in patients undergoing on-pump CABG surgery, so herein it can be used as a single independent parameter to predict postoperative outcome.
Keywords
endothelin-1
preoperative
postoperative
coronary artery bypass grafting
on-pump
clinical outcome
Introduction
Endothelin (ET), an endothelium-derived peptide with potent vasoconstrictive action, exists in three isoforms, ET-1, ET-2, ET-3.1, 2 Endothelin-1, the predominant isopeptide, is likely to be physiologically most important in regulating vascular function and maintaining vascular homeostasis. Conversely in pathological situations, it may be expressed in response to acute and chronic vascular injury. It acts on two distinct receptor subtypes, ETA and ETB.2 The dominant vascular effect of ET-1 is vasoconstriction via stimulation of the ETA receptor on vascular smooth muscle cells. Activation of the ETB receptor on vascular smooth muscle also results in vasoconstriction, whereas stimulation of endothelial cell ETB receptors induces vasodilatation via release in nitric oxide or prostacyclin. Besides modulating vascular tone, ET-1 evokes several biological effects including stimulation of smooth muscle cell growth and inflammatory responses.3, 4
The reported plasma levels of ET were found to be fairly divergent ranging from 0.2 to 18.5 pg/mL; however, the accepted normal plasma level of ET in healthy subjects is 1 to 2 pg/mL. Elevated levels are seen in multitude of diseases ranging from drug induced and obstructive nephropathy, prostatic cancer, ulcerative colitis and Crohn's disease, Hirschsprung's disease, and psoriasis and seborrheic keratosis.5, 6 Elevated levels of plasma ET-1 have been identified in subpopulations at risk of ischemic heart disease including smokers, diabetics, hyperlipidemic, hypertensive subjects, and in patients with generalized atherosclerotic disease.5, 6 Furthermore, the expression of ET-1 is enhanced in coronary atherosclerotic plaques, which implicates its direct causation in ischemic heart disease. An increased level also has been noted by few authors after on-pump coronary artery bypass grafting (CABG).7, 8, 9
With the above background, this research was conducted to study the association between preoperative plasma ET-I levels and clinical outcome in patients undergoing routine on-pump CABG.
Methods
After Institutional Ethics Committee approval and obtaining written informed consent, 58 adult patients scheduled for elective CABG under cardiopulmonary bypass (CPB) were included in this prospective study. Exclusion criteria were smokers, patients on mechanical ventilation, acute coronary syndrome, ejection fraction less than 55%, endocrinological disorders, patients on drugs like anti estrogen and cox-2 inhibitors, active infection, any documented arrhythmias, renal failure, CABG with valve surgery, and redo surgery.
Premedication consisted of 0.1mg/kg morphine and 0.5mg/kg promethazine intramuscularly. After applying pulse oximetry and five lead electrocardiogram, venous access and routine right radial artery cannulation was established. Induction of anesthesia was performed with thiopentone 5mg/kg, fentanyl 3µg/kg, and rocuronium 1mg/kg. After intubation of trachea, the lungs were ventilated with 50% oxygen in air. Ventilation was controlled with a tidal volume of 7 to 8 mL/kg and a positive end-expiratory pressure of 0 to 5 mm Hg. The ventilator rate was adjusted to maintain an arterial partial pressure of carbon dioxide of 35 to 40 mm Hg. After heparinization with 4 mg/kg, CPB was instituted. On rewarming, infusion of nitroglycerin was initiated at a dose of 0.5 to 1 µg/kg/min. All the patients were given injection Xylocard 2% 100 mg and magnesium sulfate 2 g on release on cross clamp. On coming off CPB, additional support in terms of dopamine, dobutamine, milrinone, adrenaline infusion or intraaortic balloon pump (IABP) support was started as required by different patients. The patients were shifted to intensive care unit (ICU) on mechanical ventilator. The total hours of mechanical ventilation, ICU stay, and the total hospital stay were recorded and these parameters were considered as primary outcome measures. The secondary outcomes were development of complications in terms of infection, arrhythmia, respiratory problems, renal dysfunction, neurological problems, and mortality. All the patients were followed up by an investigator who was unaware of the patient's preoperative biochemistry, findings on electrocardiogram, and clinical condition before surgery.
Blood was collected from radial artery in all patients using ethylenediamine tetraacetic acid vials prior to anesthesia induction. The blood specimen was brought from operating room to laboratory immediately and centrifuged at 2500 rpm for 15 minutes. The separated plasma was stored at −80°C until further analysis. Plasma ET 1 concentrations were determined by using enzyme linked immunoassays (R&D Systems, Inc., United States).
Sample Size Calculation and Statistical Analysis
Sample size was pre-estimated at 90% power and 0.5 effect size at 0.05 α level of significance. Effect size was estimated by piloting 15 patients. A sample size of 46 was considered to be adequate. More number of patients were included to compensate for the dropout. Data has been expressed as mean ± SD, median (range), or number percentages. Categorical data are presented as absolute number and number percentages. Normally distributed continuous variables are presented as mean and standard deviation (SD). ET-1 levels exhibited a skewed distribution and here have been expressed as median and interquarantine range. Fisher's exact test was used to test difference between independent categorical data. Difference between two independent groups of continuous data was tested by using Mann–Whitney U test. To test the strength of the association between ET-1 level or continuous variables, Spearman's rank correlation was used. Spearman coefficient of correlation was performed to evaluate the association of mechanical ventilation, ICU stay, and hospital stay with plasma ET-1 level. Mann–Whitney U test was used to evaluate the correlation of inotrope/IABP use as well as preoperative outcome parameters with that of preoperative ET-1 level. Differences are cited at 95% confidence interval. Values of p less than 0.05 were considered to be statistically significant.
Results
We demonstrated that preoperative ET-1 levels are predictor of duration of mechanical ventilation, ICU stay, and hospital stay as well as postoperative complications. The demographics and clinical profile of the study population is narrated in Table 1. Only six patients (10.34%) had history of old myocardial infarction (MI). The preoperative ET-1 level ranges from 0.6 to 30.33 pg/mL (median value: 5). Eight (13.8%) of patients needed one inotrope, three patients (5.1%) needed two inotropes, and more than two inotropes were required in three patients (5.1%) (Fig. 1). Five patients (8.6%) needed IABP to overcome ventricular dysfunction during the postoperative period (Fig. 1). The duration of mechanical ventilation, ICU stay, and hospital stay is represented in Table 2 and the details of postoperative complications are described in Table 3. We noticed a direct correlation of plasma ET-1 level with duration of mechanical ventilation, ICU stay, and hospital stay with respective coefficient of correlations of 0.68 (p = 0.002; Fig. 2), 0.58 (p = 0.001; Fig. 3), and 0.61 (p = 0.006; Fig. 4), respectively. The authors also noticed an increased in levels of plasma ET-1 level in patients with inotrope and IABP use (Fig. 1).
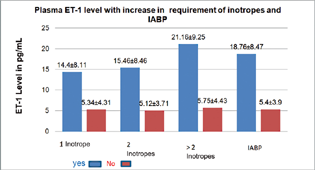
- Plasma endothelin-1 (ET-1) level in patients with increase inotropic requirement and intraaortic balloon pump (IABP) use.
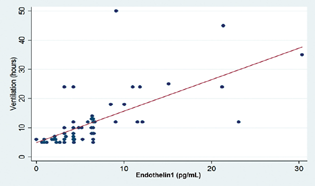
- Relation of duration of plasma endothelin-1 level and mechanical ventilation (r = 0.6881).
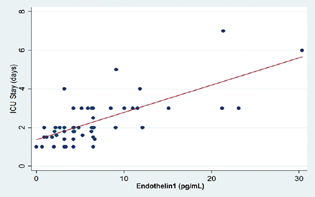
- Relation of duration of plasma endothelin-1 level and intensive care unit (ICU) stay (r = 0.5829).
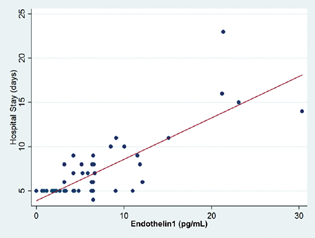
- Relation of duration of plasma endothelin-1 level and hospital stay (r = 0.6119).
|
Variable |
Median (range) |
|---|---|
|
Age (years) |
55.5 (31–84) |
|
Sex (M: F) |
(52: 6) |
|
Height (cm) |
172 (154–184) |
|
Weight (kg) |
72 (48–112) |
|
BSA (m2) |
1.85 (1.5–2.24) |
|
BMI (kg/m2) |
23.45 (17.8–37.4) |
|
Old MI (yes: no) |
6: 52 |
|
No. of grafts |
3 |
|
Endothelin-1 (pg/mL) |
5 (0.6–30.33) |
|
Duration of surgery (min) |
325 (200–380) |
|
CPB time (min) |
82 (65–120) |
|
AoXCl time (min) |
48 (35–90) |
Abbreviations: AoXCl, Aortic crossclamp; BMI, body mass index; BSA, body surface area; CPB, cardiopulmonary bypass; MI, myocardial infarction.
|
Variable |
Median (range) |
|---|---|
|
Mechanical ventilation (h) |
9 (5–50) |
|
ICU stay (d) |
2 (1–7) |
|
Hospital stay (d) |
5 (4–23) |
Abbreviation: ICU, intensive care unit.
The occurrence of complications was also seen in patients with higher ET-1 levels and the p-value was significant for infection (p = 0.006), arrhythmias (p = 0.001), renal (p = 0.004), and respiratory problems (p = 0.001) (Table 3). The correlation for neurological outcome and mortality with that of ET-1 levels could not be studied as only single patient in the study had these complications wherein the Mann–Whitney U test could not be applied.
|
Complication |
Number (%) |
Plasma ET-1 level in pg/mL, mean ± SD |
p-Value |
|---|---|---|---|
|
Infection |
0.0068 |
||
|
Yes |
4 (6.9) |
17.49 ± 10.42 |
|
|
No |
54 (93.1) |
5.74 ± 4.47 |
|
|
Arrhythmia |
0.0001 |
||
|
Yes |
13 (22.42) |
12.27 ± 7.84 |
|
|
No |
45 (77.58) |
4.9 ± 3.75 |
|
|
Resp. problem |
0.0012 |
||
|
Yes |
4 (6.9) |
21.99 ± 6.27 |
|
|
No |
54 (93.1) |
5.4 ± 3.80 |
|
|
Renal dysfunction |
0.0046 |
||
|
Yes |
3 (5.1) |
24.28 ± 5.23 |
|
|
No |
55 (94.82) |
5.58 ± 3.98 |
|
|
CNS problems |
− |
||
|
Yes |
1 (1.7) |
9.11 |
|
|
No |
57 (98.27) |
6.5 ± 5.82 |
|
|
Death |
− |
||
|
Yes |
1 (1.7) |
8.5 |
|
|
No |
57 (98.27) |
6.52 ± 5.8 |
Abbreviations: ET-1, endothelin-1; CNS, central nervous system; SD, standard deviation.
Discussion
In patients with coronary artery disease (CAD), there occurs significant neurohormonal system activation and release in bioactive molecules that can continue well into the postoperative period. ET-1 is one such potent bioactive peptide that has been demonstrated to influence vascular resistance properties in the systemic, pulmonary, and coronary circulation.1, 2 ET-1 is a powerful vasoconstrictor, also involved in vascular remodeling. Identification of ET-1 as a target to pharmacological intervention has led to the discovery of number of compounds that can block the receptors via which ET-1 effect is mediated.10 Previous authors have also demonstrated in vitro that exposure of myocardial preparations to ET-1 influences contractile performance.3 With ET-1 established as clinically relevant in the cohorts of pulmonary hypertension, efforts have never moved to determine whether preoperative ET-1 can be used to improve risk stratification of cardiac surgical patients especially those suffering from CAD in which ET-1 is a mediator of disease to a great extent.
The number of patients undergoing CABG is always in increasing trend world wise.11, 12 Looking toward this trend, it is also expected that the number of high-risk patients as well as postoperative adverse event are also increasing. So, we believe there is no harm in thinking of any additional risk factors apart from the existing one that can contribute to the postoperative outcome. Preoperative cardiovascular testing including the functional status is mostly done in patients to undergo CABG. However, many of these populations are elderly and have limited preoperative physical activity level in whom exercise testing is not feasible. A preoperative biomarker test, therefore, could prove useful for surgical risk stratification and perioperative patient care if it is easy to measure as well as sensitive for cardiovascular pathology and adverse postoperative outcomes. This preoperative test can add to what can be anticipated by using clinical, angiographic, and echocardiographic criterion to determine postoperative outcome.
Few studies have reported that elevated ET-1 levels are associated with reperfusion injury and microvascular obstruction following percutaneous coronary revascularization in ST segment elevated MI patients.4, 13 Elevated plasma levels of ET-1 have been identified in several cardiovascular disease states, as well as during CABG operations requiring CPB.14
An increased expression of ET-1 has also been shown in patients having risk factors for the development of CAD. As these factors also contribute to the postoperative outcome of the patients, theoretically ET-1 could be a surrogate for these outcome parameters. None of our patients were diabetics or had any abnormalities that can increase ET-1 level significantly apart from hyperlipidemia and hypertension and these two factors were similar to all patients studied.
Unić et al14 in one of their researches evaluated the influence of CPB on ET-1 expression in various circulation compartments in patients undergoing myocardial revascularization. The authors demonstrated an elevated ET-1 level in on-pump patients that correlated with troponin-1 levels 24 hour postoperatively. However, off-pump myocardial revascularization attenuated ET-1 expression in all investigated vascular compartment implicating the influence of CPB on ET-1 level.11 This study is just a hypothetical one to evaluate the importance of preoperative ET-1 level that can cause extensive microvascular dysfunctional state. The dysfunction may exist presurgery or can be induced later. The presurgical status is more significant because an already insulted myocardium is prone for more damage in the subsequent period than that of a less damaged one. In this study, we measured only the baseline ET-1 level and assumed that the patients with already elevated level of this peptide must have had further escalation of the levels following CPB.
In this study, patients who required inotropes on coming off CPB or had required IABP support were seen to have higher ET-1 levels preoperatively. Though multitude of factors may determine the occurrence and the outcome in CAD patients, most of these factors are associated with higher levels of ET-1, which explain the correlation of ET-1 and the outcome of patients in the study. The demonstration of increased systemic as well as cardiac release in ET-1 during CABG implies that ET-1 may influence not only native atherosclerotic coronary arteries but also vascular grafts used in CABG. This may contribute to postoperative vascular as well as hemodynamic complications including graft failure during the postoperative period.15 As CPB leads to progressive increase in ET-1 level, the patients with a higher baseline level may have a worse situation during the perioperative period compared with those with lower baseline level. Increased use of inotropes and IABP in this study supports these facts. Our study is indirectly supported by Tool et al, who administered a selective ET-1A subtype receptor antagonist perioperatively to patients with poor left ventricular ejection fraction. These patients did not show any significant hemodynamic compromise.16
Sharma et al have also shown that the increase in ET-1 in diabetic patients is significantly higher than in nondiabetics undergoing on-pump CABG. They have attributed the poor outcome in diabetics to the higher levels of ET-1. In this study, all patients were nondiabetics.17
Bond et al in one of their researches have shown that the prolonged duration of ventilation has been correlated to the increased graft and internal mammary artery sensitivity to the ET-1. These authors revealed that both systemic and pulmonary arterial ET levels were increased by approximately 50% immediately after bypass grafting and increased by another 85% during first 24 hours postoperatively.8 Therefore, it is logical to think that this surge of ET-1 can be more with a higher preoperative level and can be more damaging. The higher levels of ET-1 in the preoperative period have correlated well with duration of ventilation, ICU, and hospital stay in this study.
The reperfusion injury caused during CABG attributed to polymorphonuclear cell activation was shown to be associated with the ET-1 by Bugajski et al. Thus, patients with higher preoperative ET-1 levels as in this study may have had higher chances of reperfusion injury resulting in higher inotropic support requirement and incidence of complications.18
There is substantial heterogeneity in ET-1 threshold and its association with postoperative outcome in individual patients. Potential reason for this heterogeneity includes variability in commercially available ET-1assays and overall cardiovascular health of a patient. Still, there is nonexistence of literature saying about the cutoff point of ET-1 that can contribute toward an adverse event and this fact needs attention. As ET-1 level is associated with the grade of endothelial injury or myocardial stress, this is more of a reason one should study the preoperative level to know the significance of existing damage that can affect the perioperative outcome. It is essential to establish different preoperative ET-1 risk threshold for different group of cardiac surgical patients for the purpose of prognostication. As ET-1 is a biomarker for atherosclerosis and severity of CAD, from a biological standpoint, elevated preoperative ET-1 is most likely to be associated with postoperative morbidity and mortality in such group of patients. Further studies focused on the hypothesis that elevated preoperative ET-1 predicts occurrence of high incidence of postoperative morbidity may identify preoperative predictive value of ET-1 test. A negative predictive value of preoperative ET-1 level is also equally important. Similar to C-reactive protein and cardiac troponin, ET-1 can be taken as a risk prediction model in CABG patient; however, further study is needed to see whether multiple preoperative biomarkers could improve surgical risk assessment and the positive predictive value can be provided by ET-1 test alone. Furthermore, more sophisticated statistical methods need to be applied to evaluate optimal ET-1 risk threshold. The final exciting word about evaluating preoperative ET-1level is its potential to be used to guide clinical care to improve patient outcome.
We demonstrated that preoperative ET-1 levels are predictor of duration of mechanical ventilation, ICU stay, and hospital stay as well as postoperative complication. The main weakness of this study is a low incidence of perioperative death and other complications due to a small cohort. Finding out the cutoff value of ET-1 was also not feasible due to similar reason.
These results of this work should be repeated in a larger cohort powered to detect objective primary outcomes in all the patients. Ideally, these results should determine the utility of ET-1 like brain natriuretic peptide or troponin in combination with existing risk stratification tools, and more importantly should determine whether interventions that reduce ET-1 levels preoperatively can prevent perioperative complications in patients undergoing CABG.
Conclusion
This study clearly concludes that higher levels of preoperative ET-1 level correlate well to clinical outcome of patients undergoing on-pump CABG surgery. The authors suggest that further research is needed in this field in a large cohort to consider ET-1 as a risk stratification parameter. ET-1 antagonist may be considered in the preoperative period to improve outcome in patients with high ET-1 level.
Funding/Acknowledgments
We are grateful to all those who supported this work. We would like to thank the Doctorate of Medicine students and nursing staff in cardiovascular surgical units for their help and support for this study. We acknowledge the help and support of enzyme-linked immunosorbent assay lab in the department of pediatrics, AIIMS, New Delhi and the support staff in this department. This study is partly funded from Individual Research Grant.
Conflict of Interest
None declared.
References
- Increased plasma levels of endothelin-1 and urotensin-II in patients with coronary heart disease. Heart Vessels. 2010;25(2):138-143.
- [Google Scholar]
- Hemodynamic and coronary effects of the endothelin antagonist bosentan in patients with coronary artery disease. Circulation. 1998;98(21):2235-2240.
- [Google Scholar]
- Exogenous effects and endogenous production of endothelin in cardiac myocytes: potential significance in heart failure. Am J Physiol. 1996;271:H2629-H2637. (6 Pt 2, Suppl):
- [Google Scholar]
- Usefulness of endothelin-1 assessment in acute myocardial infarction. Rev Esp Cardiol. 2011;64(2):105-110.
- [Google Scholar]
- Endothelin system: the double-edged sword in health and disease. Annu Rev Pharmacol Toxicol. 2001;41:851-876.
- [Google Scholar]
- Clinical significance of endothelin in cardiovascular disease. Curr Opin Cardiol. 1997;12(4):354-367.
- [Google Scholar]
- Natriuretic peptides and endothelin-1 in patients undergoing coronary artery bypass grafting. Gen Physiol Biophys. 2007;26(3):194-199.
- [Google Scholar]
- Endothelin-1 during and after cardiopulmonary bypass: association to graft sensitivity and postoperative recovery. J Thorac Cardiovasc Surg. 2001;122(2):358-364.
- [Google Scholar]
- Change of N-terminal pro-brain natriuretic peptide and big endothelin in patients undergoing coronary artery bypass grafting. . 2007;19:667-670.
- [Google Scholar]
- The cardiovascular physiology and pharmacology of endothelin-1. Adv Pharmacol. 2010;60:1-26.
- [Google Scholar]
- Fifty years of coronary artery bypass grafting. J Thorac Dis. 2018;10(3):1960-1967.
- [Google Scholar]
- Perspective on coronary interventions & cardiac surgeries in India. Indian J Med Res. 2010;132:543-548.
- [Google Scholar]
- Neurohumoral activation in percutaneous coronary interventions: apropos of ten vasoactive substances during and immediately following coronary rotastenting. Indian Heart J. 2001;53(3):301-307.
- [Google Scholar]
- Off-pump myocardial revascularization attenuates endothelin-1 expression in systemic, pulmonary, and coronary circulation. Wien Klin Wochenschr. 2014;126:710-717. (21-22):
- [Google Scholar]
- Endothelin and effects of endothelin-receptor activation in the mammary and radial artery. Scand Cardiovasc J. 2004;38(4):240-244.
- [Google Scholar]
- Selective endothelin-1 receptor type A inhibition in subjects undergoing cardiac surgery with preexisting left ventricular dysfunction: influence on early postoperative hemodynamics. J Thorac Cardiovasc Surg. 2010;139(3):646-654.
- [Google Scholar]
- Elevated coronary endothelin-1 but not nitric oxide in diabetics during CABG. Ann Thorac Surg. 1999;67(6):1659-1663.
- [Google Scholar]
- Plasma-mediated stimulation of neutrophil superoxide anion production during coronary artery bypass grafting: role of endothelin-1. Thorac Cardiovasc Surg. 1999;47(3):144-147.
- [Google Scholar]






