Translate this page into:
Nutrition Aggrandizement while on ECMO
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Nutrition accrual on extracorporeal membrane oxygenation (ECMO) is the need of the hour. The crescendo interest in nutrition optimization on ECMO comes in the wake of the recent American Society for Parenteral and Enternal Nutrition (ASPEN) guidelines on pediatric patients.1 Due to the technical hazards of ECMO, the presence of a multitude of inotropes, hemodynamic perturbations, and the risk of ischemic bowel, the association with nutrition therapy on ECMO is controversial.2 The crescendo waxing and waning of feeding on ECMO are to be avoided. A recent review round-up of the literature assures that beginning enteral nutrition (EN) early in ECMO is secure and circumspect.3
Most of these indisposed ill ECMO patients have limited nutrients as endogenous stores; thus, it is important to administer nutritional support as early as possible in these moribund patients. So, relatively high nutritional requirements, with early institution of nutritional support, is important.4, 5 This, however, is delayed in most intensive care unit (ICU) settings. So, EN is ideal as it stimulates the secretion of intestinal hormones.6 As ECMO patients have limited nutritional reserves and high nutritional requirements are essential in these sick patients, early feeding on ECMO is essentially needed.7 As EN is begun, multifold benefits appear, some of which are enlisted in Table 1.
|
• Prevents sepsis |
|
• Stimulates structural and functional changes in the gut through the release of intestinal hormones in the gut |
|
• Is well-tolerated and safe |
|
• High vasopressor support can be started |
|
• Post cardiopulmonary bypass (CPB), an ECMO on high vasopressors, enteral nutrition (EN) is successful |
ECMO Patients are on high ECMO Support
Patients on ECMO remain on high doses of inotropes and are critically ill. These patients usually receive high doses of vasoactive agents (especially in venoarterial [VA] ECMO), sometimes there is use of steroids, which alongwith high inotropic support may prolong the length of stay in the ICU. Medications adversely affect the gastric emptying, impacting enteral feeding and subsequent caloric adequacy.
Venoarterial (VA) ECMO patients undergo malnutrition and consumptive protein catabolism. Hence, their nutritional requirements are immense (Table 2).
|
• Protein soaking up in the body during VA ECMO process leads to malnourishment in the patients |
|
• Administration of appropriate nutrition to ECMO patients is difficult because of hemodynamic instability and multiorgan failure |
|
• When the daily requirement of proteins in the VA ECMO, patients over 8 to 14 days, is met with, then it reduces the 90-day mortality by 18% |
Recent literature shows that, over time, the prevalence of both nonocclusive bowel necrosis and mesenteric ischemia is seen in ECMO patients, especially if reporting is not adhered to by the clinicians themselves. Most patients on ECMO may have had an earlier circulatory shock and the timing of inserting an ECMO, in a phase of cardiogenic shock, to date remains debatable.3
Research has, however, also concluded, that ECMO patients are on high inotrope doses; so, in these patients, external nutrition can be resorted to with a very low incidence of both nonocclusive bowel necrosis and mesenteric ischemia.8
Hollow Fiber PMPA Oxygenators aid Enteral Nutrition
The ECMO run brings with it inflammation and oxidative stress.9, 10 As newer biocompatible materials such as protein oxidation with the use of polysulfone membranes and cellulose acetate ones, were used earlier, the use of the latter in 2022 is replaced with hollow fiber, and the incidence of inflammation decreased.9, 10
ECMO and Continuous Renal Replacement Therapy
The addition of renal replacement therapy also aids in stress reduction on ECMO.11 Continuous renal replacement therapy (CRRT) with ECMO induces a systematic inflammatory response with an increase in multiorgan failure and mortality with the advent of new polymethyl pentene membrane of the ECMO oxygenators, diffusion of lipid emulsions, and heavy molecular weight-based nutrients for patient benefit as EN therapy seems to have been surmounted with these hollow fiber oxygen use. In-depth knowledge of the type of membrane and nutrient detail use is essential to circumvent these problematic issues.
Factors Influencing Enteral Nutrition
A patient's underlying diagnosis and vasopressor support are important factors influencing a physician's decision to implement EN. Vasopressor requirement and underlying diagnoses are the primary and secondary determinants of whether to begin EN early or not11 (Table 3).
|
• Underlying patients diagnosis, for which ECMO was initiated |
|
• Patients vasopressor requirements |
|
• Sedation levels of the ECMO patients |
|
• Low cardiac output |
|
• Prolonged hypoxia |
Enteral Nutrition is Safe in Both VA and VV ECMO
Uncertainty about nutrition in ECMO may be associated with concerns of involved paralysis and/or heavy sedation with neonatal ECMO, which may affect the gut function, in addition to the effect of VA ECMO itself, which may reduce the perfusion of the gut.12 Heavy sedation on ECMO may impair the gut function; VA ECMO may add to it by decreasing gut perfusion, low cardiac output in a peripheral hospital before ECMO or pre-ECMO hypoxia may hamper gut perfusion on VA ECMO, fluid overload with excessive intravenous fluids leads to generalized edema and anasarca with hampered gut motility. Enteral nutrition is safe in both VA and venovenous (VV) ECMO and can be well tolerated when the patient is stable on ECMO.13
However, the venous congestion of the bowel resolves with the reduction of airway pressure, subsequently improving feeding tolerance. As per the ASPEN 2019 and ESPEN 2021 guidelines, 25 to 30 Kcal/kg/day can be used for patients with a body mass index (BMI) of less than 30 units. Edema-free body weight needs to be used. Estimated energy for the obese patient (BMI > 30) can be estimated as 22 to 25 kcal/kg/day of the ideal body weight ( Flowchart 1 ; Box 1 ; Table 4 ).
|
Protein requirements up to |
3 g/kg/d |
|
Non protein nitrogen calories greater than |
60 kcal/kg/d |
|
Positive nitrogen balances more than |
240 mg/kg/d |
|
Nitrogen intake |
>400 mg/kg/d |
|
Sodium requirements without diuretics is |
4–7 mEq/kg/d |
|
• Enteral feeding in neonates on ECMO should be initiated when the patients on ECMO, has clinically stabilized • Provision of adequate dietary proteins promotes a positive protein balance and promotes the anabolic effect of insulin |
|
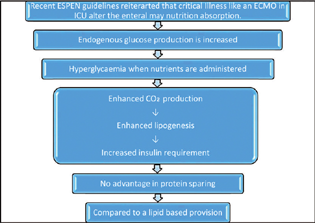
- Recent ESPEN guidelines reiterarted that critical illness such as an ECMO in the ICU may alter the enteral nutrition absorption.
A paucity of data on nutritional requirements in ECMO and inadequate nutrition leads to higher infection rates in ECMO,2 higher ICU length of stay (LOS), length of mechanical ventilation, and mortality in most observational studies.15 Enteral feed interruptions exist in the ICU for reasons such as hemodynamic instability, gastrointestinal complications, and interruptions for procedures. Most studies on VV ECMO especially were fed by the gastric route of feeding.16 In some studies on both VV and VA ECMO, the enteral route of feeding is also common. However, there was no mention of the gastric residual volume in both the above studies.
No clinical guidelines exist for nutrition in ECMO in the adult population but only exist for neonates in both VV ECMO and VA ECMO enteral nutrition seems to be well accepted by most patients. The nutrition support clinician's expertise is essential in providing appropriate nutrition support for the patient undergoing ECMO support. It is apparent that the clinical practice guidelines for nutrition support in adult ECMO patients are well accepted for now. The ASPEN 2010 guidelines can be referred to in the case of neonates, requiring ECMO support. In the 2019 clinical guidelines for validating, the body composition came up for assessment in clinical populations.1 The use of postpyloric feeding ranged from 6% to 35% across studies. Lukas et al reported reluctance to insert postpyloric feeding tubes due to coagulopathy and bleeding concerns in their patient cohort. It has been reported that in postoperative cardiac patients receiving postpyloric feeding, energy delivery was higher compared with those fed solely via the gastric route.
This special issue of the Journal of Cardiac Critical Care TSS (JCCC) on “Cardiac Nutrition” is the next step toward the discussion of recent guidelines and literature2 on nutrition for ECMO, which has so far been an underestimated subject. It also makes the readers aware of the importance of starting early EN in their sick ICU patients, and also brings about awareness of how important to select healthy sources of proteins, fats, and oils especially keeping in mind, that renal function decline in the severely ill cardiac patients in the ICU. The editorial and review article by Dr. Yatin Mehta's team brings forth the nuances of nutrition in the diabetic, hypertensive, and ischemic cardiac patients in the ICU. The brief communication on Pandoras Box—what remains at the bottom and predicting acute kidney injury (AKI) in off pump coronary bypass grafting (OPCABG) patients with malnutrition inflammation liaison are all worth reading in this “Cardiac Nutrition” special issue. When a clinician is fully conscious/aware of his astute knowledge of nutrition, she/he initiates it at an appropriate time in the ECMO patient, despite the adverse tabernacles of ICU administration.
Acknowledgments
We would like to especially thank Dr. Sunny Duttagupta and Tanya Punj for their inspirational hardwork and contribution to JCCCTSS. We will miss them at Thieme and at JCCCTSS as we started this journal with them. We wish them greener pastures in the future.
Conflict of Interest
None declared.
References
- ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48-79.
- [Google Scholar]
- American Society for Parenteral and Enteral Nutrition Clinical Guidelines: the validity of body composition assessment in clinical populations. JPEN J Parenter Enteral Nutr. 2020;44(1):12-43.
- [Google Scholar]
- A narrative review of nutrition therapy in patients receiving extracorporeal membrane oxygenation. ASAIO J 2021
- [CrossRef] [Google Scholar]
- Nutrition considerations in the neonatal extracorporeal life support patient. Nutr Clin Pract. 1994;9(1):22-27.
- [Google Scholar]
- Early feeding strategies in preterm and critically ill neonates. Neonatal Netw. 2001;20(7):7-18.
- [Google Scholar]
- Enteral nutrition in the critically ill patient: a critical review of the evidence. Intensive Care Med. 1993;19(8):435-442.
- [Google Scholar]
- Early enteral feeding, compared with parenteral, reduces postoperative septic complications. The results of a meta-analysis. Ann Surg. 1992;216(2):172-183.
- [Google Scholar]
- Safety and outcomes of enteral nutrition in circulatory shock. JPEN J Parenter Enteral Nutr. 2020;44(5):779-784.
- [Google Scholar]
- Effect of changing from a cellulose acetate to a polysulphone dialysis membrane on protein oxidation and inflammation markers. Clin Nephrol. 2004;61(3):198-206.
- [Google Scholar]
- Vitamin E-coated cellulose acetate dialysis membrane: long-term effect on inflammation and oxidative stress. Ren Fail. 2010;32(3):287-293.
- [Google Scholar]
- Practice guidelines for nutrition in critically ill patients: a relook for Indian scenario. Indian J Crit Care Med. 2018;22(4):263-273.
- [Google Scholar]
- Nutrition support during extracorporeal membrane oxygenation (ECMO) in adults: a retrospective audit of 86 patients. Intensive Care Med. 2013;39(11):1989-1994.
- [Google Scholar]
- Plasma leakage through microporous membranes. Role of phospholipids. ASAIO J. 1992;38(3):M399-M405.
- [Google Scholar]
- Energy expenditure of patients on ECMO: A prospective pilot study. Acta Anaesthesiol Scand. 2019;63(3):360-364.
- [Google Scholar]
- Computerized energy balance and complications in critically ill patients: an observational study. Clin Nutr. 2006;25(1):37-44.
- [Google Scholar]
- Early enteral feedings in adults receiving venovenous extracorporeal membrane oxygenation. JPEN J Parenter Enteral Nutr. 2004;28(5):295-300.
- [Google Scholar]





