Translate this page into:
Ankle Block for Acute Pain Management in a Patient with Mitral Valve Prolapse and Infective Endocarditis with Dry Gangrene of Toes
Sambhunath Das, MD Department of Cardiac Anaesthesia and Critical Care, All India Institute of Medical Sciences (AIIMS) New Delhi India sambhunathds833@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Ankle block represents a regional anesthesia technique to provide anesthesia for the procedures related to the foot. It is mainly used as a sole anesthesia technique or as an adjunct for postoperative pain relief in foot operations. It is an infiltrative block with advantages like being technically easier, safe, having minimal side effects, and having a high success rate. Management of postoperative pain is an essential service provided by a cardiac anesthesiologist to patients undergoing operative procedures, but the knowledge in providing regional anesthesia may be used beyond the operating room or critical care unit. In the present case, we administered an ankle block to alleviate the pain in case of dry gangrene.
Keywords
ankle block
acute pain management
mitral valve prolapse
infective endocarditis
dry gangrene of toes
Introduction
Ankle block represents a regional anesthesia technique to provide anesthesia for the procedures related to foot.1 It is mainly used as a sole anesthesia technique or as an adjunct for postoperative pain relief in foot operations. It is an infiltrative block with advantages like being technically easier, safe with minimal side effects, and high success rate.2 The use of which can also be extended for the perioperative and critical care management of pain. We describe the management of acute pain in a case of gangrene of toes intractable to routine analgesics.
Case Report
A 25-year-old-female, a known case of mitral valve prolapse with severe mitral regurgitation (MR) and infective endocarditis (IE) of the mitral valve, presented to emergency department with a chief complaint of fever for 1 month and blackish discoloration of the 3rd and 4th toes with severe pain in right foot for 2 weeks. The patient was admitted for further evaluation and management.
On physical examination the 3rd and 4th toes in the right limb showed gangrenous changes. Transthoracic echo showed mitral valve prolapse with severe MR with vegetations on anterior and posterior mitral leaflets suggestive of IE of mitral valve. Septic emboli causing dry gangrene of 3rd and 4th toes on the right lower limb was diagnosed (Fig. 1). The computed tomography angiography detected complete posterior occlusion of the left common iliac artery with distal reformation of the left common iliac artery and pseudoaneurysm in the right internal iliac artery with occlusion of distal part of popliteal artery. An intravenous antibiotic was started along with anticoagulant medication in the form of injection Clexane. Analgesia with tramadol and paracetamol was continued. Surgery consultation was done and advised no active interventions. The patient had severe and intractable pain in her toes in spite of the intravenous analgesics. The cardiac anesthesiologist was consulted for the management of acute pain.

- Gangrenous change of the right 3rd and 4th toes.
Ankle block of the deep peroneal, superficial peroneal, and sural nerves of the right foot was performed under ultrasound guidance (Fig. 2); after this block patient had complete relief of her pain. A total of 10 mL of injection ropivacaine 0.75% and 5 mL of injection lignocaine 2% with injection dexmedetomidine 25 mcg as an adjuvant was used for the ankle block.
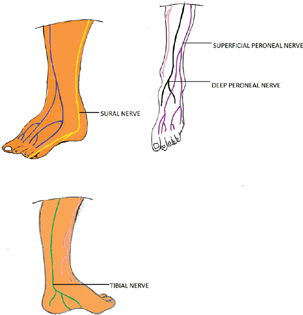
- Sensory nerve supply of the foot.
Discussion
In this case the patient had developed dry gangrene of the 3rd and 4th toes of right foot, which required no active surgical management. The patient's main concern at present was the excruciating pain in spite of routine analgesics and anticoagulant therapy. Ankle block was a good regional anesthesia and analgesia option in this situation. Since the patient had pain only over the lateral toes as mentioned, the three components (superficial peroneal, sural nerve, and deep peroneal nerve) of the ankle block was sufficient to relieve the pain.3 The patient had significant improvement in pain after the procedure. Theoretically, the block would also enhance the circulation distal to the block due to vasodilation induced by the regional anesthesia technique.4
Conclusion
Management of postoperative pain is an essential service provided by a cardiac anesthesiologist to the patients undergoing operative procedures, but the knowledge in providing regional anesthesia may be used beyond the operating room or critical care unit. In the present case we administered ankle block to alleviate the pain in case of dry gangrene.
Conflict of Interest
None declared.
Funding None.
References
- Ankle-foot peripheral nerve block for mid and forefoot surgery. Foot Ankle. 1983;4(2):86-90.
- [Google Scholar]
- Ankle block success rate: a prospective analysis of 1,000 patients. Can J Anaesth. 2005;52(2):209-210.
- [Google Scholar]
- Ultrasound-guided ankle blocks: a review of current practices. AANA J. 2015;83(5):357-364.
- [Google Scholar]
- Blood flow index as an indicator of successful sciatic nerve block: a prospective observational study using laser speckle contrast imaging. Br J Anaesth. 2018;121(4):859-866.
- [Google Scholar]






