Translate this page into:
Plugging the Unplugged: Simultaneous Percutaneous Closure of Anterior Mitral Leaflet and Aortic Root Perforation
Chinmaya Nanda, MD, FIACTA Medanta Institute of Critical Care and Anaesthesiology, Medanta the Medicity Sector 38, Gurgaon, Haryana,122001 India nandachinu@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
There are very few case reports of percutaneous device closure of anterior mitral leaflet perforation. We describe here a case of simultaneous percutaneous closure of aortic root perforation and anterior mitral perforation. These cases are challenging as they are presently done in high-risk patients with no guidelines described to date.
Keywords
percutaneous device closure
anterior mitral leaflet perforation
transesophageal echocardiography
Introduction
Mitral valve leaflet perforations are generally rare and mostly due to infective endocarditis.1 Other causes of perforation can be iatrogenic or due to autoimmune diseases like systemic lupus erythematosus or antiphospholipid syndrome. There is fibrous continuity between the anterior mitral leaflet (AML) and the aortic valve. The middle of the AML corresponds to the anatomical location of the commissure lying in between the left and noncoronary sinuses of the aortic valve. Because of their proximity, either valve can be injured during the surgical intervention of the other.
Case Report
A 40-year-old patient was admitted with ethanol-related chronic liver disease with liver cirrhosis Child Pugh Grade C. He was a prospective liver transplant recipient. He presented with shortness of breath New York Heart Association III, abdominal distension, and pedal edema. The patient had a recent history of congestive cardiac failure because of severe mitral and aortic regurgitation. Transesophageal echocardiography (TEE) performed showed a bicuspid aortic valve with perforation of one cusp along with periaortic abscess leading to severe aortic regurgitation. The jet of aortic regurgitation hitting the AML leads to perforation of AML causing severe mitral regurgitation. Left ventricular ejection was 55%, right ventricular function was normal, dilated left atrium was 5.3 cm, and left ventricle was 6.1/3.8 cm. Multiple sets of blood cultures prior to the procedure were sterile.
The patient was a very high-risk candidate for double valve repair/replacement in view of his advanced liver disease and he would not have survived for long with conservative medical therapy. Following a heart team discussion, the patient was planned for percutaneous closure of leaks in the mitral and aortic valves with informed high-risk consent and a plan for surgical conversion if the percutaneous procedure was not successful. There was no similar case report in searching the literature.
Various device options were available, namely Amplatzer Vascular Plug III, Amplatzer Atrial Septal Occluder (A-ASD), and Amplatzer Duct Occluder II. The procedure was performed in the hybrid operation theater under general anesthesia with two-dimensional TEE and fluoroscopy guidance. AML perforation was closed with ASD device closure of size 16 and aortic root rent closed with ASD device closure of size 8 (Fig. 1). The procedure involved unique challenges like crossing the defect, selecting the appropriate device, and the behavior of AML after device deployment (Fig. 2). Post-procedure, there was no mitral regurgitation and only mild aortic regurgitation (Fig. 3). The procedure was uneventful.
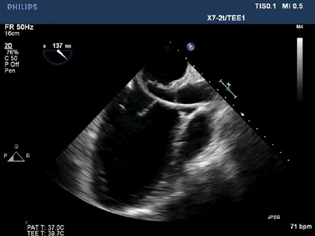
- Fluoroscopy showing catheter across anterior mitral leaflet perforation.
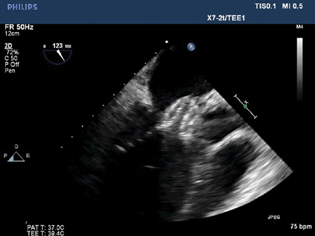
- Two-dimensional transesophageal echocardiography showing atrial septal occluder device placement across anterior mitral leaflet and aortic root perforation.
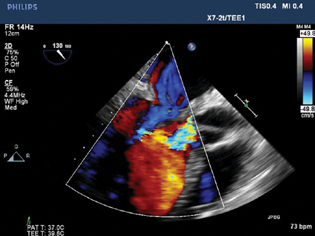
- Transesophageal echocardiography color Doppler showing no residual mitral regurgitation and a significant reduction in aortic regurgitation after device closure.
Discussion
Very few cases of percutaneous repair of AML Perforation have been reported in the literature.2, 3, 4, 5, 6, 7 To our best knowledge, this is the first case being reported in English literature where an AML perforation and aortic root rent were closed simultaneously using a percutaneous approach. Guidelines for percutaneous closure of AML perforation do not exist. Long-term follow-up for the outcome of these procedures has not been studied. Further research is needed to establish the mid- and long-term outcomes of these percutaneous techniques. These procedures are now limited to high-risk surgical candidates and cases where patients do not opt for surgical repair. Real-time three-dimensional TEE can be very helpful in guiding these procedures.
Conflict of Interest
None declared.
References
- Perforation of the anterior mitral leaflet caused by aortic valve endocarditis: diagnosis by two-dimensional, transesophageal echocardiography and color flow Doppler. J Am Soc Echocardiogr. 1992;5(2):195-198.
- [Google Scholar]
- Transcatheter repair of anterior mitral leaflet perforation in a patient with mechanical aortic valve using antegrade and retrograde approaches: case report. J Struct Heart Dis. 2018;4:234-239.
- [Google Scholar]
- Percutaneous closure of a native mitral valve perforation. Rev Esp Cardiol. 2010;63(5):597.
- [Google Scholar]
- Percutaneous repair of anterior mitral leaflet perforation. J Invasive Cardiol. 2012;24(3):134-137.
- [Google Scholar]
- First report of percutaneous closure of anterior mitral leaflet perforation using a paravalvular leak device (PLD) Postepy Kardiol Interwencyjnej. 2016;12(3):274-275.
- [Google Scholar]
- Retrograde transcatheter closure of anterior mitral valve leaflet perforation. Ann Pediatr Cardiol. 2019;12(3):312-314.
- [Google Scholar]
- Percutaneous closure of iatrogenic anterior mitral leaflet perforation: a case report. Eur Heart J Case Rep. 2020;4(4):1-5.
- [Google Scholar]






