Translate this page into:
Transesophageal Echocardiography Probe-induced Esophageal Perforation
*Corresponding author: Ajmer Singh, Department of Cardiac Anaesthesia, Medanta the Medicity, Gurugram, Haryana, India. ajmersingh@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Singh A, Nanda C, Mehta Y. Transesophageal Echocardiography Probe-induced Esophageal Perforation. J Card Crit Care TSS. 2024;8:169-71. doi: 10.25259/JCCC_57_2023
Abstract
Transesophageal echocardiography (TEE) probe-induced esophageal perforation is rare. A 67-year-old man underwent a Bentall procedure with mitral valve replacement under TEE monitoring. Two hours later, the patient had a blood-stained aspirate from the nasogastric tube. Contrast-enhanced computed tomography of the chest showed esophageal perforation, which was treated with the fluoroscopic deployment of covered metal stents. The patient had an uneventful recovery.
Keywords
Esophageal perforation
Transesophageal echocardiography
Cardiac surgery
INTRODUCTION
Transesophageal echocardiography (TEE) is an indispensable monitoring tool during cardiac surgery. In general, considered a safe procedure, insertion and manipulation of the TEE probe can, however, result in injury to teeth, oropharynx, esophagus, or stomach. The incidence of TEE probe-induced esophageal perforation during cardiac surgery is reported as 0.03–0.09%. Although esophageal perforation is an uncommon complication, the associated mortality is very high (up to 30%).[1,2] A systemic review by Sainathan and Andaz has reported 35 esophageal perforations from 22 studies with a mortality rate of 28.5%.[3] We, herein, report a case of esophageal perforation caused by a TEE probe during cardiac surgery. The complication was managed by the endoscopic deployment of the stent.
CASE REPORT
A 67-year-old man with severe aortic regurgitation, aortic root dilation (6.5 cm × 6.0 cm), and severe mitral regurgitation was admitted for the Bentall procedure and mitral valve replacement. After obtaining informed consent, anesthesia was induced using standard drugs and monitoring. A well-lubricated TEE probe (X7-2t, Philips) was inserted smoothly using a laryngoscope, with the head in midline and the neck in the flexed position, in the absence of any contraindications. During the TEE examination, the probe was advanced or withdrawn in the neutral position. Anteflexion or retroflection of the TEE probe was avoided while the probe was inside the esophagus. When not in use, the probe was kept in “freeze” mode. The removal of the TEE probe after completion of the surgical procedure revealed some blood at the tip of the probe. Direct laryngoscopy did not show any blood clots or fresh bleeding in the oral cavity. A nasogastric tube was inserted; blood-stained aspirate was sucked out and flushed with saline. After two hours, an aspirate from the nasogastric tube showed fresh blood. An upper gastrointestinal (GI) endoscopy was performed urgently, and it showed a hiatus hernia, and a large clot filling the entire lumen of the esophagus with jagged mucosa at a distance of 25 cm from the incisors [Figure 1]. Contrast-enhanced computed tomography (CT) angiography of the chest using Gastrografin® showed a dilated esophagus, an extravasation of the contrast in the esophagus at 25 cm, and another at gastroesophageal junction suspicious of partial tears [Figure 2]. Under fluoroscopic guidance, two expandable covered metallic stents (Niti-S Beta™, Taewoong Medical, Seoul, South Korea) were deployed, and there was no further bleeding [Figure 3]. Intravenous antibiotics, proton pump inhibitors, and parenteral nutrition were continued for one week, followed by enteral nutrition through the nasogastric tube. Repeat CT angiography done at two weeks showed healed perforations, following which oral feeding was commenced. The subsequent course of the patient was unremarkable.
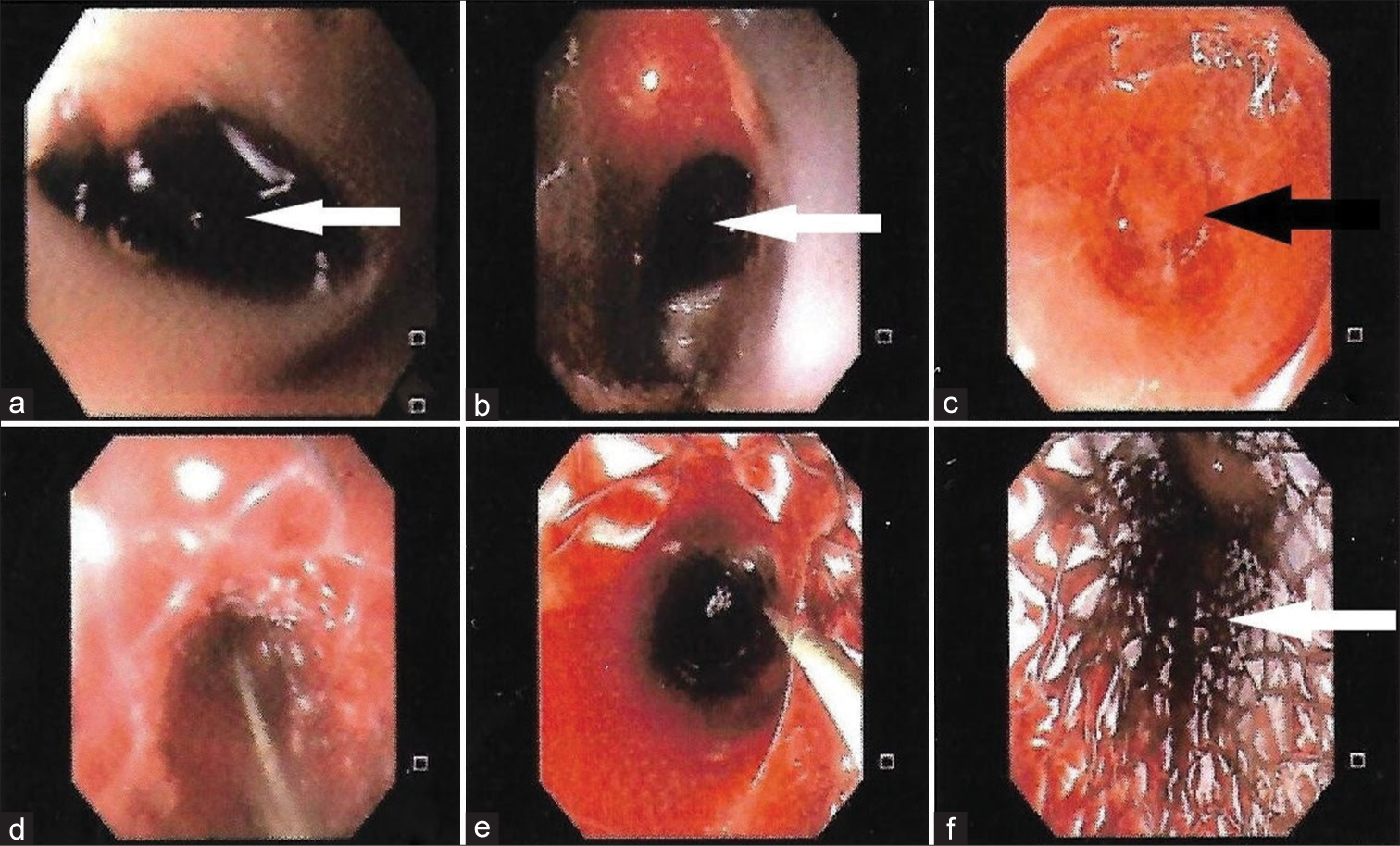
- Upper gastrointestinal endoscopy showing (a and b) blood clots in esophagus (white arrows), (c) possible site of tear (black arrow), and (d-f) deployment of covered metal stent in the esophagus (white arrow).
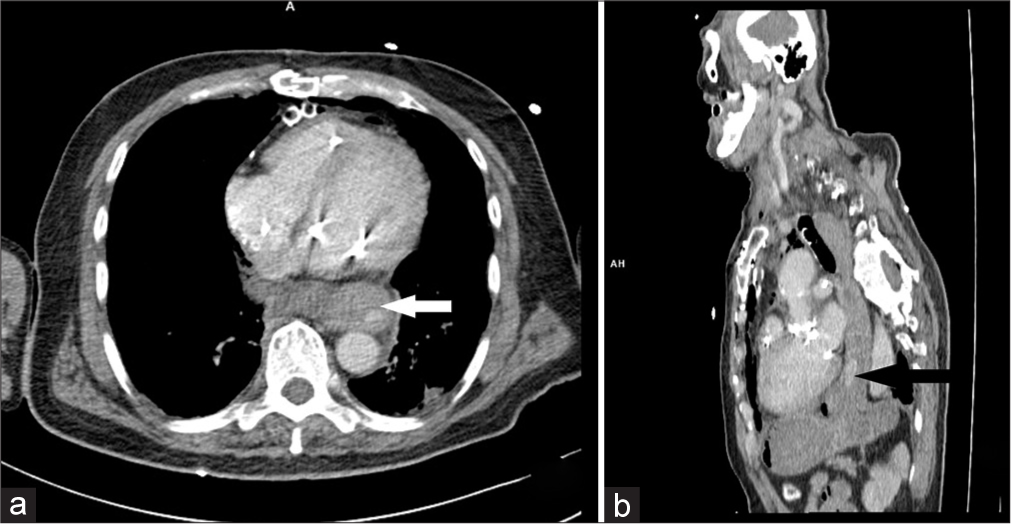
- Axial and sagittal computed tomography scans of the chest showing (a) dilated esophagus (white arrow) and (b) extravasation of the contrast (black arrow).
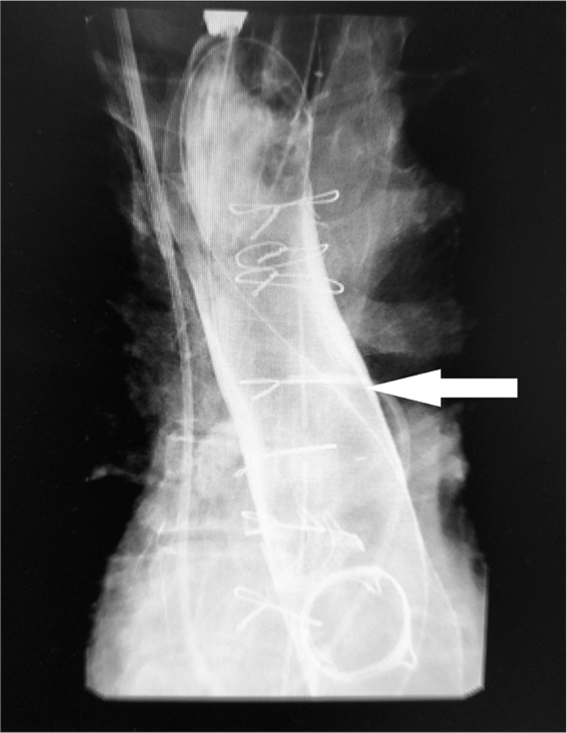
- Fluoroscopy image showing deployed stent in the esophagus (arrow).
DISCUSSION
Insertion of a TEE probe can result in esophageal perforation even when the insertion is smooth. Approximately 33–75% of all esophageal perforations are iatrogenic.[4] A prolonged, constant pressure at the esophageal mucosa caused by the TEE probe can lead to indirect trauma of the GI tract. Furthermore, episodes of low blood circulation and hypoperfusion during cardiac surgery can potentially result in tissue ischemia and necrosis.[5] Other mechanisms for GI injury includes (i) secondary to thermal injury produced by vibrations of piezoelectric crystals and (ii) absorption of ultrasound energy by the adjacent tissues. Moreover, patients with severe atherosclerotic cardiovascular disease often have an impaired esophageal circulation. Hypoperfusion of the esophagus can lead to thermal injury in such patients. Predisposing factors for TEE probe-induced esophageal perforation include advanced age, esophageal pathologies (Zenker’s diverticulum, hiatus hernia, esophageal stenosis, prior esophageal surgery or radiation, and intraluminal mass), external compression by tumor, distortion caused by an enlarged left atrium, thoracic aortic aneurysms, and cervical osteophytes.[6] The patient described here had a hiatus hernia, dilated esophagus, and aortic aneurysm as risk factors.
Clinical presentation of intrathoracic perforations can be in the form of chest pain, respiratory difficulties, hemodynamic instability, breathing difficulties, low oxygen saturation, pneumothorax, subcutaneous emphysema, or sepsis. The diagnosis of a suspected esophageal perforation can be confirmed by a careful endoscopic inspection and a chest X-ray. However, if a perforation cannot be confirmed endoscopically, a swallow test using a water-soluble contrast or a chest CT should be done.
Treatment options for esophageal perforations can be conservative, endoscopic, or surgical. Conservative management is appropriate in patients with perforation in the cervical esophagus. The endoscopic management of esophageal perforations has shown more promising results if there is an early recognition (<24 hours), the small size of the defect (<1–2 cm), involvement of intrathoracic part, surgically unfit patients, and a skillful endoscopist. Endoscopic treatment can also be performed using partially-covered metal or fully-covered metal stents, or using clips.[7] The indications for surgical intervention include: a delayed diagnosis (>24 h), hemodynamic instability, lack of advanced endoscopic expertise, or a persistent leak after endoscopic treatment. Successful management of GI perforations requires a tailored and integrative approach based on clinical signs and symptoms, early or delayed presentation, hemodynamic stability, size and location of the tear, local expertise, and the availability of endoscopists and devices.[8] Timely identification and quick management have been shown to reduce the morbidity and mortality associated with esophageal perforation.
CONCLUSION
TEE-probe-induced esophageal perforation is a very rare complication. It can occur even after a smooth insertion of a TEE probe; a high degree of suspicion is essential to reach a prompt diagnosis of esophageal perforation and offer an effective treatment on time.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent was not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Complications Related to Peri-operative Transoesophageal Echocardiography-a One-year Prospective National Audit by the Association of Cardiothoracic Anaesthesia and Critical Care. Anaesthesia. 2020;75:21-6.
- [CrossRef] [PubMed] [Google Scholar]
- Low Risk of Gastroesophageal Injury Associated with Transesophageal Echocardiography during Cardiac Surgery. J Cardiothorac Vasc Anesth. 1993;7:175-7.
- [CrossRef] [PubMed] [Google Scholar]
- A Systematic Review of Transesophageal Echocardiography-induced Esophageal Perforation. Echocardiography. 2013;30:977-83.
- [CrossRef] [PubMed] [Google Scholar]
- Esophageal Emergencies: Things that will Wake you from a Sound Sleep. Gastroenterol Clin North Am. 2003;32:1035-52.
- [CrossRef] [PubMed] [Google Scholar]
- The Safety of Intraoperative Transesophageal Echocardiography: A Case Series of 7200 Cardiac Surgical Patients. Anesth Analg. 2001;92:1126-30.
- [CrossRef] [PubMed] [Google Scholar]
- Transesophageal Echocardiography-related Complications. Can J Anaesth. 2008;55:622-47.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and Management of Iatrogenic Endoscopic Perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014;46:693-711.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic Management of Gastrointestinal Leaks and Fistulae: What Option do we have? World J Gastroenterol. 2020;26:4198-217.
- [CrossRef] [PubMed] [Google Scholar]






