Translate this page into:
Transesophageal Echocardiographic Illustration of Postinfarction Ventricular Septal Rupture
Neeti Makhija, MD Department of Cardiac Anaesthesia and Critical Care, Cardiothoracic Centre, All India Institute of Medical Sciences Room No. 9,7th Floor, Ansari Nagar, New Delhi, 110029 India neetimakhija@hotmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Postinfarction ventricular septal rupture (VSR) is a rare but dreaded mechanical complication of myocardial infarction. Moreover, patient develops cardiogenic shock or congestive heart failure requiring early surgical intervention. To optimize surgical repair, perioperative confirmation, determining location of VSR and adequacy of repair, is mandatory. Assessment can be obtained by the transesophageal echocardiography (TEE). Use of two- and three-dimensional TEE techniques clearly delineate size and shape of septal rupture and involvement of other cardiac structures. We report a patient presenting with postinfarction VSR for elective VSR repair and surgical revascularization and implication of TEE in perioperative management.
Keywords
coronary revascularization
echocardiography
myocardial infarction
transesophageal echocardiography
ventricular septal rupture
Introduction
Postinfarction ventricular septal rupture (VSR) is a life-threatening mechanical complication of acute myocardial infarction with an incidence up to 2%.1 It is the second most common form of cardiac rupture.2 Echocardiography is an easy and noninvasive technique that clearly delineates the mechanical complication. Transthoracic echocardiography (TTE) is a valuable tool for initial diagnosis. However, transesophageal echocardiography (TEE) not only determines the VSR but also provides assessment of ventricular function, and eventual postsurgical residual VSR in the perioperative setting. Three-dimensional echocardiography adds another dimension in delineation of VSR in adjunct to two-dimensional findings.3
We report a patient presenting with postinfarction VSR for elective VSR repair and surgical revascularization and the implication of TEE in perioperative management.
Case Report
A 53-year-old man was scheduled for repair of postinfarction VSR along with coronary revascularization. The patient had an event of acute coronary syndrome with inferior wall myocardial infarction 1 month earlier. He had history of severe right-sided chest pain, diaphoresis, and progressive dyspnea. Coronary angiography revealed triple-vessel disease with left anterior descending artery (LAD) 70–80% obstruction with normal diagonals, obtuse marginal 70–80% diseased and right coronary artery (RCA) 100% occluded too was affected. Being a diabetic patient with triple-vessel disease, plan was elective surgical revascularization. On further evaluation for surgery, TTE demonstrated a VSR in the basal inferior septum causing left-to-right shunt.
Patient was therefore planned for coronary artery bypass grafting and VSR repair under cardiopulmonary bypass (CPB). Antiplatelets, anticoagulants, diuretics, and angiotensin converting enzyme inhibitor were withheld for surgery and β blocker continued. Tablet alprazolam was advised for anxiolysis. After wheeling the patient into the operating room, standard American Society of Anesthesiology (ASA) monitors were attached, large bore venous access and right radial arterial line secured. Balanced anesthesia technique with titrated doses of fentanyl, midazolam, etomidate and rocuronium were used for induction and muscle paralysis. Airway was secured and central venous access taken in the right internal jugular vein.
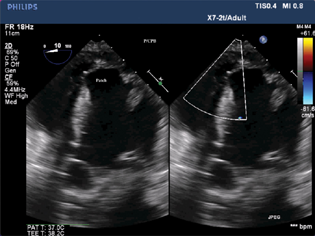
TEE was performed using an X7–2t Philips's ultrasound probe and machine (iE33 model; Philips, Bothell, Washington, United States). Deep transgastric view confirmed VSR in the mid-to-apical septum (Fig. 1, Video 1). The VSR measured 1.11 cm (Fig. 2). Midesophageal 4 chamber view revealed trivial mitral regurgitation (Fig. 3). Left ventricular (LV) ejection fraction was 44% by modified Simpson's technique. Midesophageal pulmonary vein view with pulse wave Doppler showed systolic blunting with S/D 0.6 (Fig. 4). Live three-dimensional echocardiography demonstrated VSR in the mid-to-apical septum (Fig. 5, Video 2). Rest valves were normal.
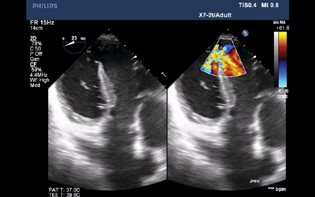
- Two-dimensional transesophageal echocardiographic deep transgastric color compared view showing ventricular septal rupture in the mid-to-apical septum.
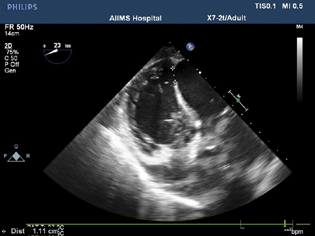
- Two-dimensional transesophageal echocardiographic deep transgastric color compared view measuring ventricular septal rupture size 1.11 cm.
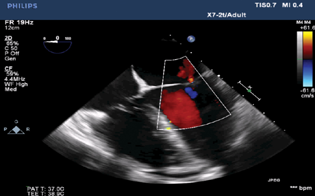
- Two-dimensional transesophageal echocardiographic midesophageal four-chamber view revealed trivial mitral regurgitation.
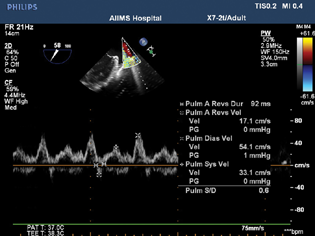
- Two-dimensional transesophageal echocardiographic midesophageal pulmonary vein view with pulse wave Doppler showed systolic blunting with S/D 0.6
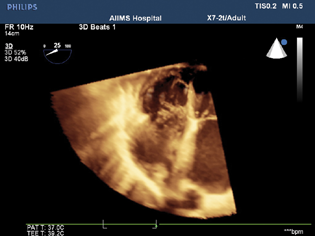
- Live three-dimensional echocardiography in deep transgastric view demonstrated ventricular septal rupture in the mid-to-apical septum.
After adequate heparinization, arterial and bicaval venous canulation, CPB was instituted. The VSR was repaired with Dacron patch, coronary revascularization in the form of left internal mammary artery to LAD and saphenous venous graft to RCA done. The aortic cross clamp and CPB time were 128 and 82 minutes, respectively. Patient was weaned from CPB with infusion adrenaline 0.05 µg/kg/min and infusion nitroglycerin 0.5 µgg/kg/min support. Postoperative TEE showed intact ventricular patch in the deep transgastric view without any shunt (Fig. 6). After adequate hemostasis and protamine neutralization, the patient was shifted to cardiac intensive care unit for further management. Ventilation was weaned and patient was extubated after 6 hours. After 5 days of hospital stay, the patient was discharged from hospital.
- Two-dimensional transesophageal echocardiographic deep transgastric color compared view showing patch closure of ventricular septal rupture.
Discussion
Perioperative management of a patient with acute VSR is challenging because it causes left-to-right shunt with volume overload of right ventricle and increased pulmonary blood flow. The severity of left to right shunt depends on balance between systemic vascular resistance (SVR) and pulmonary vascular resistance. After induction of anesthesia LV systolic function usually deteriorates with compensatory vasoconstriction, leading to increased fraction of left-to-right shunt. Sympathetic stimuli as a result of tracheal intubation cause increased SVR with increased the shunt flow. Therefore, induction of general anesthesia and intubation must be accomplished with minimal or no hemodynamic changes in ventricular function or SVR. So, we used balanced anesthesia technique for induction of anesthesia with drugs such as fentanyl, midazolam, etomidate, and rocuronium, which resulted in minimal hemodynamic changes during intubation. Our particular case suggests that the combination of fentanyl, etomidate, and midazolam is useful for induction with maintained hemodynamic, even in patients with left-to-right shunt due to VSR. Most important concerns in anesthetic management of VSR are to reduce LV afterload and to optimize systemic blood pressure at the same time.4 Further, reduction in afterload is needed to prevent deterioration of the shunt during the pre-bypass period and in the post-bypass period, to prevent tension to the newly repaired septal wall.4 To fulfil these requirements, intravenous nitroglycerin infusion was used in addition to adrenaline infusion for our patient. Nitroglycerin has been shown to reduce LV afterload. We used infusion adrenaline for maintaining systemic perfusion pressure in addition to maintaining ventricular function. We also used sevoflurane as volatile anesthetic agent for maintenance of anesthesia during the procedure. Volatile anesthetics causes myocardial preconditioning and afterload reduction, thereby are beneficial to a patient with postinfarction VSR.
In summary, we presented a surgical patient with postinfarction VSR. General anesthesia was induced with fentanyl, midazolam, and etomidate that successfully suppressed fluctuations in hemodynamic variables associated with induction of anesthesia and tracheal intubation. Nitroglycerin and adrenalin infusion was administered for reduction in LV afterload and inotropic support, which successfully prevented the deterioration of left-to-right shunt. Intraoperatively, TEE plays a vital role in guiding the surgical technique and determine the success of surgery. Use of two- and three-dimensional TEE techniques clearly delineate size and shape of VSR and the adequacy of surgical closure.
Conflict of Interest
None declared.
Reference
- Mechanical complications of acute myocardial infarction. Cardiol Clin. 2013;31(4):519-531. , vii–viii
- [Google Scholar]
- Postinfarction ventricular septal rupture: repair by endocardial patch with infarct exclusion. J Thorac Cardiovasc Surg. 1995;110(5):1315-1322.
- [Google Scholar]
- Transesophageal two- and three-dimensional echocardiographic diagnosis of combined left ventricular pseudoaneurysm and ventricular septal rupture. Echocardiography. 2002;19(4):345-349.
- [Google Scholar]
- Anesthesia for repair of ventricular septal rupture after acute myocardial infarction. J Clin Anesth. 2007;19(6):463-466.
- [Google Scholar]








