Translate this page into:
Truncus Arteriosus with Interrupted Aortic Arch: Aortic Arch Reconstruction Without Circulatory Arrest
Bharath V, MS, MCh Department of Cardiothoracic and Vascular Surgery, All India Institute of Medical Sciences New Delhi 110029 India drbharathv@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Truncus arteriosus (TA) with interrupted aortic arch (IAA) is a rare congenital cardiac anomaly. Traditionally, IAA would require period of deep hypothermic circulatory arrest (DHCA) for aortic arch reconstruction. DHCA may cause myocardial depression and neuro-developmental dysfunction. IAA repair is presently being performed with hypothermic low-flow selective cerebral perfusion and distal body circulatory arrest. Even though this prevents cerebral adverse effects of DHCA, there is still risk to the spinal cord and kidneys.
Here, we describe the aortic arch reconstruction by maintaining the total body perfusion without any periods of circulatory arrest in a neonate with TA with IAA.
Keywords
truncus arteriosus
interrupted aortic arch
circulatory arrest
neurocognitive dysfunction
Introduction
Truncus arteriosus (TA) is a cyanotic congenital heart disease where the conotruncal septum is deficient, leading to common outflow chamber (truncus) from both the ventricles.1 In some instances, it is associated with interrupted aortic arch (IAA). The surgical repair for TA with IAA is performed in neonatal period and less frequently in infancy.2 It includes repair of the truncus by closing the ventricular septal defect (VSD) and creating right ventricle (RV) outflow using valved conduit along with aortic arch reconstruction. These can be performed in a staged manner or as a single procedure.
Case Details
A 27-day-old neonate presented to our emergency with cyanosis and features of heart failure since birth. On evaluation, the child was found to have TA (Collett Edwards type 1; Van Praagh A-4) with IAA (Type B). The child was planned for staged corrective surgery—aortic arch reconstruction in the first stage followed by truncus repair in the second stage.
Midline sternotomy was performed and pericardium was opened. External anatomy of the heart and great vessels were inspected and preoperative diagnosis was confirmed.
The aorta and pulmonary artery were dissected and right and left pulmonary arteries (RPA and LPA) looped. A 6-French aortic cannula (Bio-Medicus; Medtronic Inc., USA) was inserted into the innominate artery (IA), and a single venous cannula was placed in the right atrial body. Both RPA and LPA were snared and cardiopulmonary bypass (CPB) started. Patent ductus arteriosus (PDA) was dissected and the left subclavian artery (LSCA) and descending thoracic aorta (DTA) were identified. DTA was dissected until the fourth intercostal artery. Innominate artery and left common carotid artery (LCCA) were dissected. A 8-French aortic cannula was inserted into the DTA, 2 cm distal to LSCA origin. Now through the CPB, both upper and lower bodies were perfused (Fig. 1).
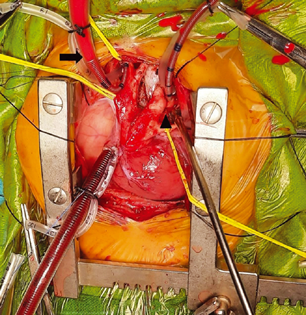
- Establishment of CPB with aortic cannulae in the innominate artery and DTA (arrow: cannula into the innominate artery; arrowhead: cannula into the DTA).
The child was cooled down to 32 degrees. Innominate artery, LCCA, and DTA were clamped. Full CPB flow was maintained. There was no change in near-infrared spectroscopy (NIRS). The heart was arrested in diastole by giving cold blood cardioplegia and topical cooling. PDA was opened and resected. Distal stump comprised LSCA and the DTA ostium was prepared. The ascending aorta was opened vertically in its lesser curvature, above the level of RPA until the base of LCCA. The LSCA and DTA stump were anastomosed to the ascending aorta in an end-to-side fashion using a 7–0 polypropylene suture (Fig. 2).
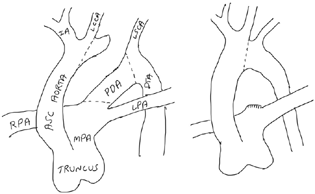
- Schematic representation of aortic arch reconstruction.
Arch deaired. All clamps were released. Hemostasis was secured and CPB was weaned off. There was no pressure gradient between the upper limb and lower limb. Due to myocardial edema, the sternum was kept open and covered with a blood bag.
Discussion
TA with IAA is a rare clinical entity. Aortic arch reconstruction was performed traditionally by total body deep hypothermic circulatory arrest (DHCA) to obtain a bloodless field in open repair of the aortic arch.3 However, it was seen that DHCA led to neurocognitive dysfunction with myocardial depression in a few children.4 To avoid this, presently, the aortic arch repair is being performed with selective low-flow antegrade cerebral perfusion with distal body circulatory arrest.5 Though this protects against cerebral complications, it entails a risk of spinal cord and renal dysfunction if the distal body circulatory arrest duration is prolonged.6
In our case, the aortic arch reconstruction was performed by maintaining the total body perfusion throughout. By doing so, the risk of spinal cord and renal injury is minimized.
Conclusion
The aim of aortic arch construction is to provide non-obstructed blood flow between the ascending aorta and DTA while maintaining cerebral perfusion. By maintaining distal perfusion through DTA during arch reconstruction, the incidence of spinal cord ischemia and renal dysfunction is minimized.
Conflict of Interest
None declared.
References
- A case of truncus arteriosus.Annales Medicinae Internae Fenniae. Helsinki, Finland: Finnish Medical Society Duodecim; 1951. p. :236-243. In:
- [Google Scholar]
- Truncus arteriosus with interruption of the aortic arch: report of a case successfully repaired. Mayo Clin Proc. 1971;46(1):40-43.
- [Google Scholar]
- Long-term outcomes following repair of truncus arteriosus and interrupted aortic arch. Eur J Cardiothorac Surg. 2020;57(2):366-372.
- [Google Scholar]
- Repair of persistent truncus arteriosus with interrupted aortic arch. Eur J Cardiothorac Surg. 2005;28(5):736-741.
- [Google Scholar]
- Aortic arch reconstruction without circulatory arrest: review of techniques, applications, and indications. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2002;5(1):116-125.
- [Google Scholar]
- Low-flow hypothermic cardiopulmonary bypass protects the brain. J Thorac Cardiovasc Surg. 1991;102(1):76-83. , discussion 83–84
- [Google Scholar]







