Translate this page into:
Role of Intra-operative Transesophageal Echocardiographic Examination in Inferior Vena Cava Tumor Thrombus Removal in a Case of Renal Ewing’s Sarcoma
*Corresponding author: Mohanish Badge, Department of Cardiac Anaesthesia and Critical Care, All India Institute of Medical Sciences, Delhi, New Delhi, India. mohanish.badge11@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Badge M, Choudhury M, Kapoor PM. Role of Intra-operative Transesophageal Echocardiographic Examination in Inferior Vena Cava Tumor Thrombus Removal in a Case of Renal Ewing’s Sarcoma. J Card Crit Care TSS. 2024;8:161-4. doi: 10.25259/JCCC_50_2023
Abstract
Ewing’s sarcoma belongs to primitive neuroectodermal tumors. Renal Ewing’s sarcoma is an extremely rare tumor that can progress to the inferior vena cava (IVC) or right atrium (RA). Renal tumors with IVC/RA extension entail removal of the tumor, including tumor thrombus in IVC with or without the use of cardiopulmonary bypass, depending on the tumor thrombus extent. Intra-operative transesophageal echocardiography provides the latest staging of tumor thrombus, its characteristics, and mobility, guides IVC clamping for tumor removal, aids in troubleshooting hemodynamic instability, and monitors completeness of tumor removal post-procedure. Transesophageal echocardiographic examination forms an indispensable part of intra-operative management in any case of IVC tumor thrombus removal.
Keywords
Ewing’s sarcoma
Inferior vena cava tumor thrombus
Intra-cardiac extension
Transesophageal echocardiographic examination
INTRODUCTION
The extension of a tumor into a vessel is termed an intra-vascular tumor thrombus. It is associated with numerous malignancies such as Wilms tumor, renal cell carcinoma, hepatocellular carcinoma, and intra-venous leiomyomas.[1] Ewing’s sarcoma of the kidney presents <1% of renal tumors. Ewing’s sarcoma invasion of the inferior vena cava (IVC) and right atrium (RA) is even rarer. It mostly presents in young adults with male preponderance. It can increase to huge sizes with non-specific symptoms. It usually carries a poor prognosis and requires both chemotherapy and surgical resection for treatment. The operative technique for extraction varies with the degree of tumor extension in IVC. The use of intra-operative transesophageal echocardiographic examination (TEE) allows for measuring the extent, guiding surgical removal, hemodynamic management, and reviewing the completeness of the procedure.
CASE REPORT
A 32-year-old female presented with low-grade fever and left flank pain on and off for one year. Contrast-enhanced computed tomography (CT) of the abdomen showed a 12.6 × 13.7 × 17.4 cm mass in the left kidney encasing the left renal artery. Tumor thrombus was present in the left renal vein, and IVC reached up to RA. A renal biopsy diagnosed the mass as Ewing’s sarcoma (primitive neuroectodermal tumor). The patient was started on chemotherapy – vincristine, adriamycin, and cyclophosphamide. Repeat CT showed a decrease in tumor size to 6.5 × 5.8 × 7.1 cm, indicating a good partial response to chemotherapy and tumor thrombus up to cavoatrial junction. The patient was posted for the left radical nephrectomy and IVC thrombus extraction.
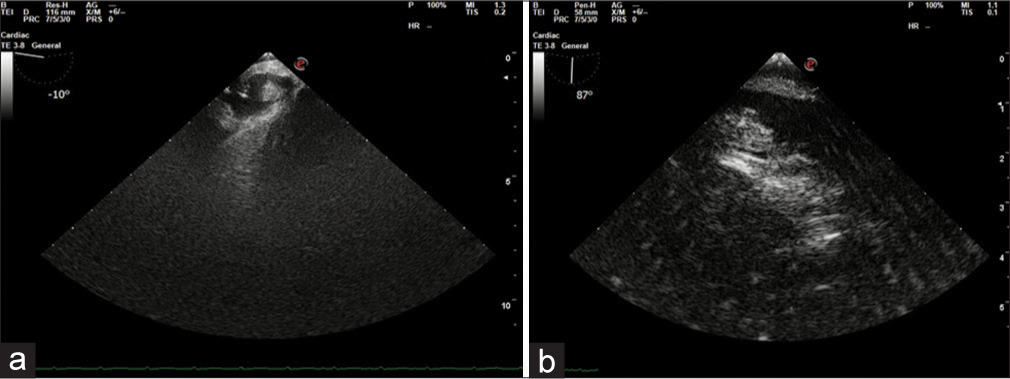
Under general anesthesia, TEE guided central venous line was inserted in the left internal jugular vein. Midesophageal (ME) bicaval view showed a venous catheter tip at the RA-superior vena cava junction [Figure 1]. Intra-operative TEE findings were concurrent with the CT findings of thrombus in IVC extending to the RA-IVC junction. The transgastric (TG) IVC short axis (SAX) view revealed a tumor thrombus obstructing approximately 70% of the IVC lumen with minimal mobility [Figure 2a]. The IVC in the long axis (LAX) showed tumor thrombus throughout the intra-hepatic IVC [Figure 2b]. TG IVC LAX view with probe withdrawn to focus IVC-RA junction showed tumor thrombus encroaching cavoatrial junction with intra-atrial extension [Figure 3]. ME bicaval view with a focus on the IVC-RA junction revealed a tumor extending in RA [Figure 4]. ME four chambers with RARV focus view showed tumor thrombus extending till the opening of the coronary sinus [Figure 5]. A comprehensive examination revealed normal valvular and ventricular function. The pre-procedure CT report mentioned a thrombus up to the cavoatrial junction hence the proposed plan was to remove the thrombus without the use of cardiopulmonary bypass (CPB). However, intra-operative TEE evaluation revealed the extension of the tumor in the RA, necessitating the use of CPB to remove the thrombus from the RA. Hence, the surgical plan was changed to perform both laparotomy and sternotomy with bicaval cannulation using CPB. After the left radical nephrectomy, CPB was instituted to retrieve the tumor thrombus. Since the tumor was adherent to the IVC wall, a partial thrombectomy could be performed. Post-CPB TEE examination revealed residual thrombus in intra-hepatic IVC in both TG IVC SAX and LAX views [Figures 6 and 7].
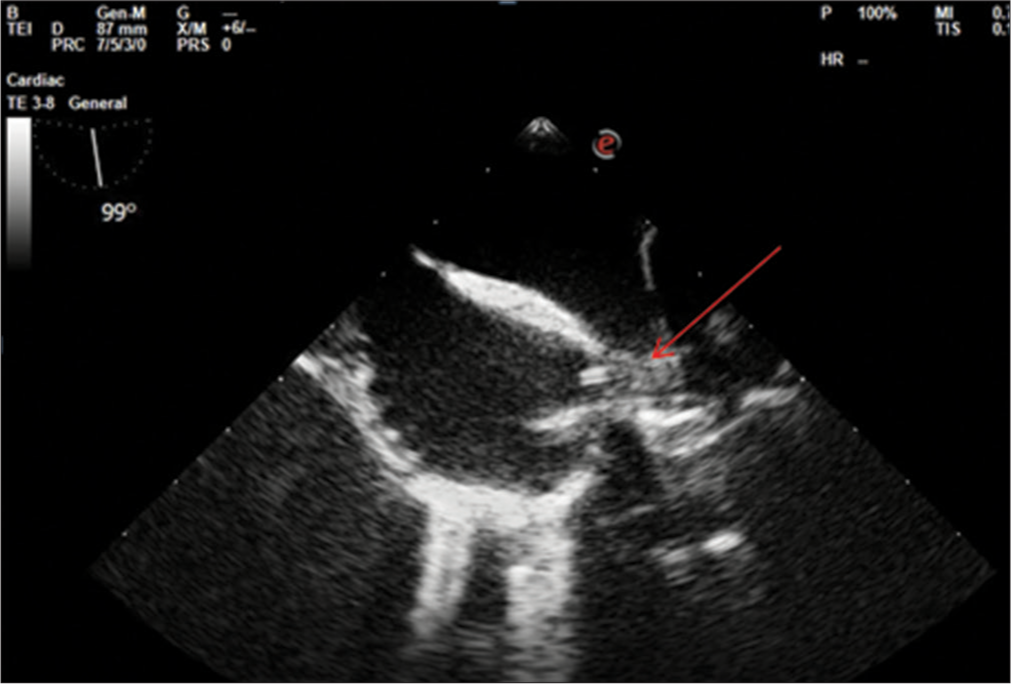
- Midesophageal bicaval view after central line insertion. Arrow showing the central line in superior vena cava.
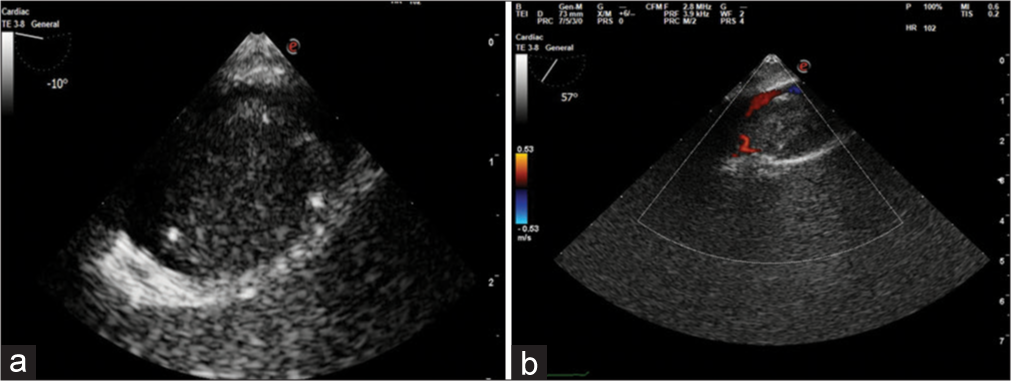
- (a) Transgastric (TG) short axis showing Tumor thrombus in inferior vena cava (IVC) compromising majority of the lumen. (b) TG IVC long axis view with color flow Doppler showing a narrow streak of flow around the thrombus.
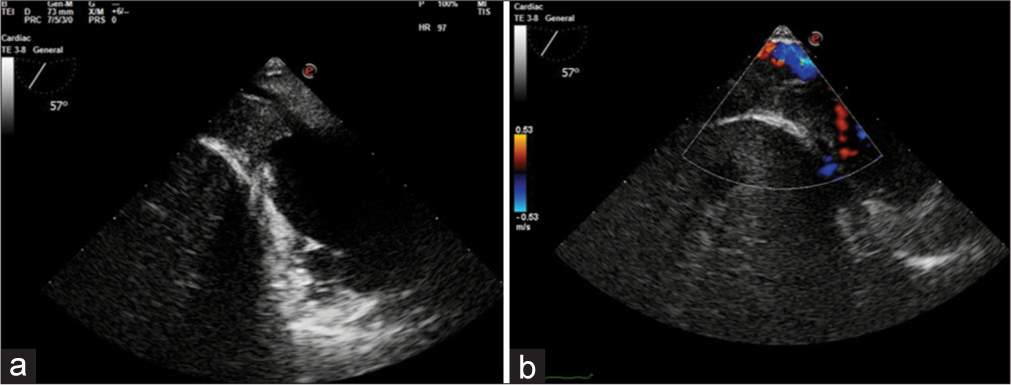
- Transgastric long axis inferior vena cava (IVC) view with probe withdrawn to focus right atrium (RA)-IVC junction – (a) showing tumor extension till RA-IVC junction and compromise of IVC lumen. (b) Color flow Doppler imaging showing turbulent flow in IVC.
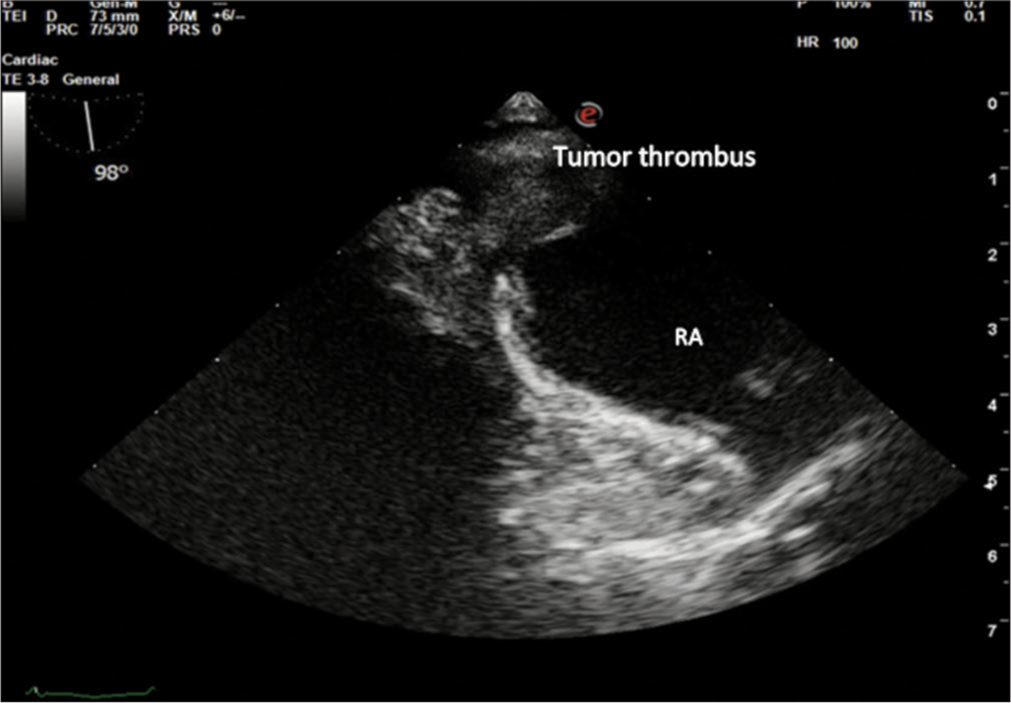
- Midesophageal bicaval view to focus opening of inferior vena cava into the right atrium (RA), showing extension of tumor thrombus into RA.
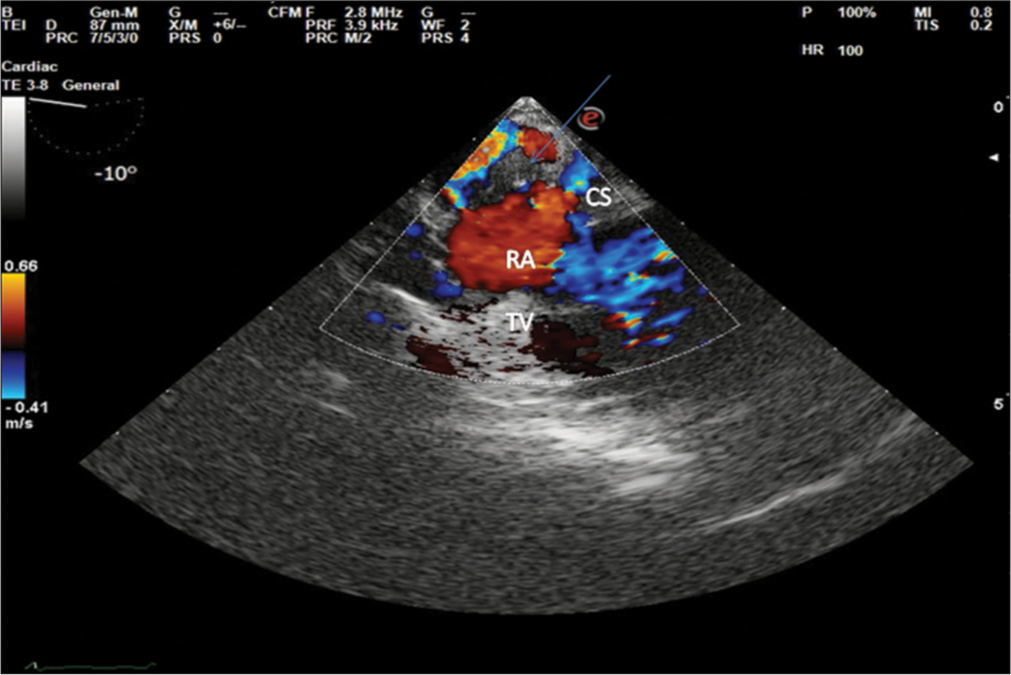
- Midesophageal four chamber view showing tumor thrombus (arrow) reaching till coronary sinus.
- (a) Transgastric (TG) inferior vena cava (IVC) short axis view: Post-thrombectomy shows residual thrombus in the IVC, note the reduced size of residual thrombus. (b) TG IVC long axis with probe withdrawn to right atrium-IVC junction, showing residual thrombus.
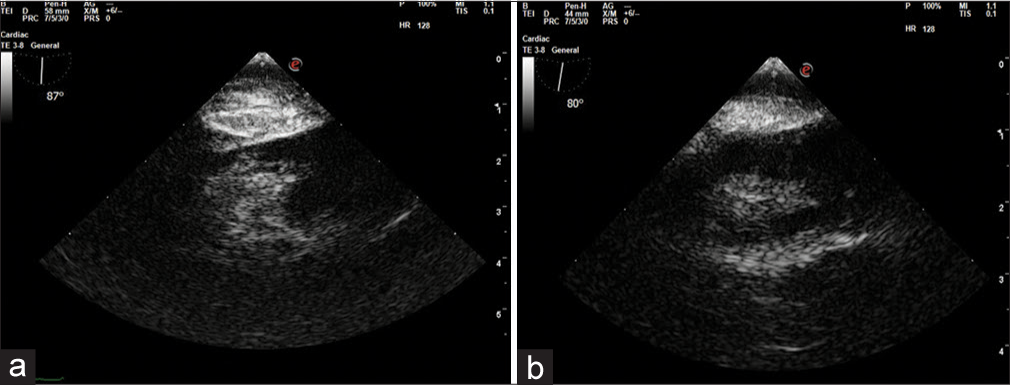
- Transgastric inferior vena cava (IVC) long axis view (a and b) showing residual tumor thrombus in intra-hepatic IVC.
DISCUSSION
Extraossesus Ewing’s sarcoma is a rare disease. Renal Ewing’s sarcoma accounts for <1% of renal neoplasms. It is an aggressive neoplasm with rapid increase in size and metastasis.[2] Approximately 50% of patients have IVC tumor thrombus at the time of presentation.[3] There are no clear guidelines for the management of this disease, and multidisciplinary treatment is recommended. The surgical approach depends on the extent of tumor progression.
The reported incidence of silent embolism on brain imaging is 63% of myxoma, 73% of papillary fibroelastosis, and 30% of left ventricular thrombus cases.[4] The same holds true for right-sided masses. Since the tumor thrombus was extending into RA, caution was exercised for central venous catheter insertion. The placement of the main venous line was done after intubation under transesophageal echocardiographic guidance, the left internal jugular vein was chosen, with the ME bicaval view in focus, and the line was inserted, avoiding any contact with the guidewire or catheter with mass. Thus preventing any untoward embolic complication.
Intra-operative TEE is used pre-procedure to discern the level of tumor thrombus according to the Mayo Clinic classification. Excision of Level III thrombus may require adjunctive venovenous or CPB, and Level IV requires open cardiac surgery with the use of CPB. There are reports of increased diagnostic sensitivity and surgical impact with increasing level of tumor thrombus.[5] TEE views for IVC assessment include TG IVC SAX detecting the degree of lumen compromise by the thrombus. TG IVC LAX for precise recognition of the cephalic extent of the tumor, the extent of caval occlusion, and tumor head characterization. Depending on the extent of the tumor, thrombectomy could be performed by a transabdominal, trans diaphragmatic, and trans pericardiac approach with or without the use of CPB,[6] the deep hypothermic circulatory arrest could be required in more challenging cases. The use of a balloon Fogarty catheter has also been reported for IVC thrombus removal minimizing hepatic mobilization.[7] In our case, visualization of the tumor throughout the intra-hepatic IVC with extension into the RA diagnosed by intra-operative TEE classified the thrombus as Level IV as opposed to the CT diagnosis of Level III. Furthermore, the minimal mobility on TEE suggested the mass could not be removed by a balloon catheter, nor could it be removed by sequentially clamping IVC without using CPB. It demanded modification of the surgical plan to use CPB with bicaval cannulation for open cardiac surgical removal of the RA extension of the thrombus. Non-detection of tumor extension in RA preoperatively could be attributed to the rapid growth of tumor thrombus, the time gap between the CT, transthoracic echocardiography and surgery, and the high sensitivity of TEE for detection of intra-cardiac mass, and accurately diagnosing its extent. During the removal of abdominal IVC tumor thrombus, the surgeons noticed the thrombus being adherent to IVC and could not be extracted by application of clamp on IVC and removing the mass en-toto. Hence, residual thrombus was to be expected. Post-thrombectomy imaging should be looked into for residual thrombus, mobility, and its propensity for embolization. Right-sided cardiac structures should be screened for inadvertent embolization of tumor thrombus.
Advantages of intra-operative TEE
Provides the latest and accurate tumor staging
Patient-tailored surgical planning
Characteristics of thrombus – adherence, mobility, and fragility
Contrast-enhanced ultrasound – differentiate tumor thrombus versus bland thrombus[8]
Quantifying the risk of embolization
Central venous line insertion
Comprehensive cardiac evaluation – for concomitant procedures
Troubleshooting hemodynamic instability – cardiac volume, function, and pulmonary embolism
Guide vascular clamp placement for off-pump procedures
Real-time visualization of tumor extraction using a catheter
CPB management for on-pump procedures 12. Post-procedure evaluation of any residual thrombus.
CONCLUSION
With the use of TEE in a multitude of procedures in IVC tumor extraction, it is imperative for the echocardiographercum-anesthesiologist to make effective use of TEE in guiding the surgical removal and overall patient safety. Thus, intra-operative TEE use is a safe, minimally invasive imaging modality and forms a major pillar for a totalitarian approach to intra-operative patient management.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Poonam Malhotra Kapoor is the member of editorial board of the journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Tumor Thrombus: Incidence, Imaging, Prognosis and Treatment. Cardiovasc Diagn Ther. 2017;7:S165-77.
- [CrossRef] [PubMed] [Google Scholar]
- Primary Ewing's Sarcoma of the Kidney: A Rare Masquerader of Renal Cell Carcinoma on Imaging. Egypt J Radiol Nucl Med. 2020;53:53.
- [CrossRef] [Google Scholar]
- Imaging Predictors for Assessment of Inferior Vena Cava Wall Invasion in Patients with Renal Cell Carcinoma and Inferior Vena Cava Tumor Thrombus: A Retrospective Study. Chin Med J (Engl). 2020;133:2078-83.
- [CrossRef] [PubMed] [Google Scholar]
- High Prevalence of Subclinical Infarction in Asymptomatic Patients with Silent Left-sided Cardiac Masses. J Am Coll Cardiol. 2019;73:2236-7.
- [CrossRef] [PubMed] [Google Scholar]
- Defining the Role of Intraoperative Transesophageal Echocardiography during Radical Nephrectomy with Inferior Vena Cava Tumor Thrombectomy for Renal Cell Carcinoma. Urology. 2017;107:161-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cavoatrial Thrombectomy without the Use of Cardiopulmonary Bypass for Abdominal Tumors. Our Experience and State of the Art. Ann Vasc Surg. 2015;29:1020.e1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Intraoperative Transesophageal Echocardiography for Inferior Vena Caval Tumor Thrombus in Renal Cell Carcinoma. Int J Urol. 2004;11:189-92.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Intraoperative Ultrasound in Robotic-assisted Radical Nephrectomy with Inferior Vena Cava Thrombectomy in Renal Cell Carcinoma. World J Urol. 2020;38:3191-8.
- [CrossRef] [PubMed] [Google Scholar]






