Translate this page into:
Postoperative Mortality in Surgically Treated Infective Endocarditis Patients and Its Correlation with EuroSCORE I
Sarvesh Pal Singh, DM Department of Cardiothoracic and Vascular Surgery, Cardio-Thoracic Centre, All India Institute of Medical Sciences New Delhi 110029 India sarveshpal.singh@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction Even after advances in medical and surgical treatment, infective endocarditis is associated with substantial morbidity and mortality. The aim of this study was to evaluate postoperative mortality in surgically treated infective endocarditis patients and its correlation with the European System for Cardiac Operative Risk Evaluation (EuroSCORE) I.
Methods This retrospective observational study included 43 patients treated surgically for infective endocarditis, between 2014 and 2019, at a tertiary care center. Mortality in surgically treated infective endocarditis patients was determined in terms of frequency (%). Patients were divided into two groups—survivors and nonsurvivors (died within 30 days of surgery). Mean EuroSCORE I of survivors and nonsurvivors was compared using the unpaired t-test with equal variance. A correlation was sought between mortality and EuroSCORE I as well. The prediction ability of EuroSCORE I for mortality was determined by the area under receiver operating characteristic curve.
Results Out of 43 patients who underwent surgery for infective endocarditis,11 patients (25.58%) died. Mean EuroSCORE I was 15.90 ± 2.02 in nonsurvivors and 7.84 ± 3.19 in survivors. EuroSCORE I was significantly higher in nonsurvivors (p < 0.05). The area under curve value was 0.9744 (p < 0.001), thus showing that EuroSCORE I predicts mortality in surgically treated infective endocarditis patients.
Conclusion The 30-day mortality in patients who underwent surgery for infective endocarditis was 25.58%. There is a significant correlation between EuroSCORE I and mortality. A EuroSCORE I value >14 predicts mortality in surgically treated infective endocarditis patients with sensitivity and specificity of 90.91 and 90.63%, respectively.
Keywords
postoperative mortality
EuroSCORE I
surgically treated infective endocarditis
Introduction
Even after many advances in medical and surgical treatment, infective endocarditis is associated with significant morbidity and mortality.1 Surgical correction of infective endocarditis is associated with the highest number of deaths seen in valvular disease patients.2
Approximately, 50 to 60% of patients with infective endocarditis require surgery.3 The common indications for operating upon such patients are heart failure, uncontrolled infection, and prevention of systemic embolism.4 Although these indications are clear, but decision to operate is guided by patient's clinical status, presence of comorbid conditions, and operative risk.5 Despite the high risk, European Society of Cardiology recommends operating to void progressive heart failure and irreversible structural damage caused by infection and to prevent systemic embolism.5
Many risk prediction models (the European System for Cardiac Operative Risk Evaluation [EuroSCORE I], EuroSCORE II, Society of Thoracic Surgeons—Infective Endocarditis [IE], PALSUSE Score [Prosthetic valve, Age >70 years, large intracardiac destruction, Staphylococcus spp., urgent surgery, Sex-female, EuroScore>10], etc.) for cardiac surgery have been developed to provide information on risk for patients and to guide decision-making.6 Out of all risk prediction models, EuroSCORE is a simple and objective system developed to predict in-hospital mortality after cardiac surgery. In a European study, mortality in surgically treated infective endocarditis patients significantly increased from 3 to 11% when EuroSCORE was more than 6.7 A study done in the Netherlands concluded that the Dutch population with aortic valve endocarditis most commonly required surgical treatment.8
The risk factors for mortality, in surgically treated infective endocarditis patients, are isolation of typical microorganism from blood cultures, C-reactive protein, age, EuroScore II, total surgical time, and postoperative complications.9
In this study, we wanted to evaluate mortality in surgically treated infective endocarditis patients and its correlation with preoperative EuroSCORE I. In our study, endocarditis was considered active if patients underwent surgery before completing a 6-week course of antibiotics treatment.
Objectives
Primary Objective
Our primary objective was to evaluate 30-day mortality in patients with infective endocarditis who underwent surgical treatment.
Secondary Objective
Our secondary objective was to assess the correlation of mortality in patients with surgically treated infective endocarditis and EuroSCORE I.
Methodology
After obtaining clearance from the institute ethics committee (vide no IECPG-172/24.02.2021), 43 patients who underwent surgery for infective endocarditis, between January 2014 and December 2019, were included in this study. This was a retrospective observational cohort study conducted at a tertiary care hospital.
Medical records of all patients (n = 43) were reviewed to collect data. All the patients fulfilled the modified Duke criteria for the diagnosis of IE.
The following data were collected for each patient: age; sex; weight; height; body mass index; date of admission; date of operation; comorbidities—hypertension, diabetes mellitus, chronic obstructive pulmonary disease, cerebrovascular disease, and renal disease; history of smoking; preoperative use of drugs like angiotensin-converting enzyme inhibitors, angiotensin receptor blocker, digoxin, anticoagulants, β blockers, diuretics, calcium channel blockers; native valve endocarditis; or previous episodes of endocarditis IV drug use.
We assessed the following findings on echocardiography: left ventricular ejection fraction, any wall motion abnormality, valve function or any abnormality, and any vegetation and its size.
History of any dental procedure in the last 60 days, prior valve operation, prior coronary artery bypass grafting, prior or recent myocardial infarction within 90 days, any aortic surgery, cardiac arteriopathy, and complications if any (preoperative) was also obtained.
Elevated levels of C-reactive protein, total leucocyte count, and rheumatoid factor and details on inotropic support, blood and blood products transfused, and duration of mechanical ventilation were also recorded.
Based on survival, all patients (n = 43) were divided into two groups.
Group 1 (survivors). Group 1 comprised surgically treated infective endocarditis patients who were discharged.
Group 2 (nonsurvivors). Surgically treated infective endocarditis patients who died within 30 days of surgery.
Mean (±standard deviation [SD]) of EuroSCORE I was calculated for each group. A correlation was sought between mortality and EuroSCORE I. The prediction ability of EuroSCORE I for mortality in surgically treated infective endocarditis patients was determined by the area under receiver operating characteristic (ROC) curve.
Statistical Analysis
Data were analyzed using Stata 16, and qualitative data were reported as absolute and relative frequency (%). For quantitative data, mean, median, mode, and standard deviation were used. The two-sample t-test was used with equal variance to correlate mortality with EuroSCORE I for risk stratification. A p-value of less than 0.05 was considered significant.
Observation and Results
In total, 43 (33 male and 10 female) patients who underwent surgery for infective endocarditis were included in our study. Out of 43 patients,11 patients (25.58%) died (Table 1). The mean (±SD), minimum, and maximum of EuroSCORE I for group 1 and group 2 are shown in Table 1.
|
Group |
No. of patients |
Min EuroSCORE |
Max EuroSCORE |
Mean EuroSCORE |
SD |
|---|---|---|---|---|---|
|
Group 1 (S) |
32 |
3 |
14 |
7.84 |
3.19 |
|
Group 2 (NS) |
11 |
12 |
19 |
15.90 |
2.02 |
|
Total |
43 |
3 |
19 |
9.90 |
4.60 |
|
Differences |
−8.06 |
Abbreviations: EuroSCORE, European System for Cardiac Operative Risk Evaluation; NS, nonsurvivors; S, survivors; SD, standard deviation.
t-Test total score, by (death).
A two-sample t-test with equal variances was used to determine the statistical significance of the difference of means between the two groups. A p-value <0.05 was considered significant. The p-value calculated was <0.001.
To detect the cutoff value of EuroSCORE I for predicting mortality in surgically treated infective endocarditis patients, with maximum sensitivity and specificity, ROC curve was plotted (Fig. 1).
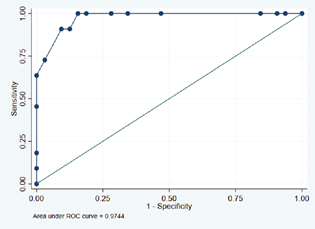
- ROC analysis for predicting mortality, in surgically treated infective endocarditis patients, using EuroSCORE I. ROC, receiver operating characteristic.
The area under ROC curve was 0.9744 (p < 0.001) as shown in Fig. 1, thus showing that EuroSCORE I has the ability to predict mortality in surgically treated infective endocarditis patients and, therefore, identify high-risk patients receiving surgical treatment for infective endocarditis.
The coordinates generated for the selection of appropriate sensitivity and specificity tradeoff are shown in Table 2.
|
EuroSCORE I |
Sensitivity |
Specificity |
Classified |
LR+ |
LR− |
|---|---|---|---|---|---|
|
Cut-off value |
|||||
|
(≥3) |
100.00% |
0.00% |
25.58% |
1.0000 |
|
|
(≥4) |
100.00% |
6.25% |
30.23% |
1.0667 |
0.0000 |
|
(≥5) |
100.00% |
9.38% |
32.56% |
1.1034 |
0.0000 |
|
(≥6) |
100.00% |
15.63% |
37.21% |
1.1852 |
0.0000 |
|
(≥8) |
100.00% |
53.13% |
65.12% |
2.1333 |
0.0000 |
|
(≥9) |
100.00% |
65.63% |
74.42% |
2.9091 |
0.0000 |
|
(≥10) |
100.00% |
71.88% |
79.07% |
3.5556 |
0.0000 |
|
(≥11) |
100.00% |
81.25% |
86.05% |
5.3333 |
0.0000 |
|
(≥12) |
100.00% |
84.38% |
88.37% |
6.4000 |
0.0000 |
|
(≥13) |
90.91% |
87.50% |
88.37% |
7.2727 |
0.1039 |
|
(≥14) |
90.91% |
90.63% |
90.70% |
9.6970 |
0.1003 |
|
(≥15) |
72.73% |
96.88% |
90.70% |
23.2727 |
0.2815 |
|
(≥16) |
63.64% |
100.00% |
90.70% |
0.3636 |
|
|
(≥17) |
45.45% |
100.00% |
86.05% |
0.5455 |
|
|
(≥18) |
18.18% |
100.00% |
79.07% |
0.8182 |
|
|
(≥19) |
9.09% |
100.00% |
76.74% |
0.9091 |
|
|
(>19) |
0.00% |
100.00% |
74.42% |
1.0000 |
Abbreviations: EuroSCORE, European System for Cardiac Operative Risk Evaluation; LR, likelihood ratio.
The cut-off value of EuroSCORE I >14 had a projected sensitivity of 90.63% and specificity of 90.7% for predicting mortality in the studied patients (Table 2). Therefore, patients of infective endocarditis with EuroSCORE I more than or equal to 14 are at a high risk of mortality.
In our study, a significant correlation was found between mortality and the amount of packed red blood cells (PRBC), fresh frozen plasma (FFP), and platelets transfused. The transfusion of blood and blood products was significantly higher in nonsurvivors compared with survivors (PRBC 48.7 ± 31.14 mL/kg vs. 14 ± 8.18 mL/kg; FFP 23 ± 13.10 mL/kg vs. 7.83 ± 4.76 mL/kg; and platelets 10.6 ± 8.83 mL/kg vs. 3.73 ± 2.61 mL/kg; p < 0.01). Similarly, the duration of mechanical ventilation was significantly higher in nonsurvivors than survivors (10.9 ± 8.11 days vs. 1.28 ± 0.68 day).
Discussion
Patients requiring surgery for active infective endocarditis have high morbidity and mortality. A retrospective study done by Varela et al in 2018 on 180 patients reported a 30-day mortality of 26.82%.10 Another retrospective study done by Patrat-Delon et al on 149 patients (median age, 64 years) with a mean EuroSCORE II of 15.8 (13.4–18.1) also reported an in-hospital mortality of 21%.6 In total, 95% of patients in their cohort had valvular regurgitation and 49% perivalvular abscess. The 30-day postoperative mortality in our patients was 25.58%. A Dutch study of 138 patients who underwent operations for infective endocarditis documented survival rates of 85, 74, and 71% at 1, 5, and 10 years, respectively.8
Many individual risk factors have been correlated with mortality in surgically treated infective endocarditis patients like age, female sex, high creatinine values (>2.0 mg/dL), left ventricular dysfunction, chronic obstructive pulmonary disease, shock, valvular abscess, isolation of specific infectious agents, etc.11 The EuroSCORE was developed in 1999 to predict early mortality in cardiac surgical patients in Europe based on objective risk factors. It mitigates the need to describe all individual risk factors separately and combines their contributory risk into one numerical value. Originally, it was established that the mortality in postoperative period for patients undergoing cardiac surgery was 3% for a EuroSCORE of 3 to 5 and it increased to 11.2% for a value of more than 6. Therefore, patients with EuroSCORE ≥6 were considered high risk for cardiac surgery.
We used EuroSCORE in patients who underwent surgery for infective endocarditis to predict mortality. We used 30-day mortality as the primary outcome because we wanted to emphasize essentially surgical mortality. Also, because ours is a tertiary care referral center for the whole country, it is challenging for patients to follow-up at regular intervals. Therefore, patients do not necessarily turn up for follow-up appointments once discharged.
Statistical analysis shows that there is a significant difference between the mean value of EuroSCORE I in group 1 (survivors) and group 2 (nonsurvivors). Thus, EuroSCORE I can be used for risk stratification in infective endocarditis patients before surgery. In this study, using ROC curve, we established the cut-off value for EuroSCORE I as ≥14 to predict mortality in surgically treated infective endocarditis patients with a sensitivity of 90.91% and specificity of 90.63%.
Compared with other risk scores meant for cardiac surgical patients, EuroSCORE I is simple, easy to use, and has objective parameters that can be easily calculated based on history, laboratory tests, and echocardiographic examination.
In a retrospective observational study of 128 patients who underwent surgery for infective endocarditis, the perioperative mortality was found to be 16.4% (n = 21).12 The median EuroSCORE I and EuroSCORE II were 13.9 and 6.6%, respectively. EuroSCORE I was found to overpredict the mortality, whereas EuroSCORE II tended to underpredict it. In this study, prosthetic valve endocarditis was an independent risk factor for mortality (odds ratio 6.6).12
Limitations of Study
Ours is a retrospective observational study from a single center. The results are based on patients with infective endocarditis who were selected to undergo the surgical procedure and could be subject to selection bias. The sample size in our study is small and may not be sufficient to accurately access the predictive ability of EuroSCORE.
Conclusion
The 30-day mortality in patients who underwent surgery for infective endocarditis was 25.58%. There is a significant correlation between EuroSCORE I and mortality. A EuroSCORE I value >14 predicts mortality in surgically treated infective endocarditis patients with sensitivity and specificity of 90.91 and 90.63%, respectively.
Conflict of Interest
None declared.
References
- Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366(26):2466-2473.
- [Google Scholar]
- Outcomes for endocarditis surgery in North America: a simplified risk scoring system. J Thorac Cardiovasc Surg. 2011;141(1):98-106. .e1, 2
- [Google Scholar]
- Prophylaxis of experimental endocarditis with antiplatelet and antithrombin agents: a role for long-term prevention of infective endocarditis in humans? J Infect Dis. 2015;211(1):72-79.
- [Google Scholar]
- Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC) Eur Heart J. 2009;30(19):2369-2413.
- [Google Scholar]
- EuroSCORE II underestimates mortality after cardiac surgery for infective endocarditis. Eur J Cardiothorac Surg. 2016;49(3):944-951.
- [Google Scholar]
- European system for cardiac operative risk evaluation (Euro SCORE) Eur J Cardiothorac Surg. 1999;16(1):9-13.
- [Google Scholar]
- Survival of surgically treated infective endocarditis: a comparison with the general Dutch population. Ann Thorac Surg. 2011;91(5):1407-1412.
- [Google Scholar]
- Mortality predictors in the surgical treatment of active infective endocarditis. Rev Bras Cir Cardiovasc. 2018;33(1):32-39.
- [Google Scholar]
- Mortality risk prediction in infective endocarditis surgery: reliability analysis of specific scores. Eur J Cardiothorac Surg. 2018;53(5):1049-1054.
- [Google Scholar]
- A predictive model for early mortality after surgical treatment of heart valve or prosthesis infective endocarditis. The EndoSCORE. Int J Cardiol. 2017;241:97-102.
- [Google Scholar]
- Assessment of perioperative mortality risk in patients with infective endocarditis undergoing cardiac surgery: performance of the EuroSCORE I and II logistic models. Interact Cardiovasc Thorac Surg. 2016;22(2):141-148.
- [Google Scholar]






