Translate this page into:
Positive Expiratory Pressure Therapy Device, the Acapella in Post-ECMO Rehabilitation
-
Received: ,
Accepted: ,
How to cite this article: Sheware TB, Ruchika. Positive expiratory pressure therapy device, the acapella in post-ECMO rehabilitation. J Card Crit Care TSS 2023;7:21-4.
Abstract
Depending on the choice of cannulation techniques, ECMO can deliver purely respiratory support, respiratory support with right ventricular support, and full cardiopulmonary support. Today, with careful patient selection, ECMO is used as a rescue therapy to allow for recovery or bridge to transplant for hypoxic respiratory failure and severe refractory cardiogenic shock. The adverse effects of deep sedation and paralysis including bradycardia, ICU-acquired paresis, and ventilator-associated pneumonia pose valid concerns with reduction in lung volumes and capacities. One of the most frequently prescribed airway clearance therapy (ACT) options for patients with chronic lung conditions or decreased lung volumes is positive expiratory pressure therapy (PEP) device (Acapella) which causes reduction in hyperinflation and many other positive facts described in this review.
Keywords
ECMO
Acapella
rehabilitation
positive expiratory pressure therapy
INTRODUCTION
Extracorporeal membrane oxygenation (ECMO)
The use of cardiopulmonary bypass technologies such as ECMO allows for more aggressive lung rest strategies and cardiovascular support than could be provided otherwise. Depending on the choice of cannulation techniques, ECMO can deliver purely, respiratory support with right ventricular support, and full cardiopulmonary support. Today, with careful patient selection, ECMO is used as a rescue therapy to allow for recovery or bridge to transplant for hypoxic respiratory failure and severe refractory cardiogenic shock.
Chest physiotherapy strategies for the patient on ECMO
Once the patient gets selected for ECMO, would be kept on acceptable ventilator settings and depending on the hemodynamics of the patient and clinical indications, the passive airway clearance therapy, that is, manual ventilation/manual hyperinflation and airway suctioning need to be started to ensure adequate ventilation in lungs. When the patient becomes fit for ECMO discontinuation and decannulation, the same passive airway clearance therapy (manual ventilation/manual hyperinflation and airway suctioning) can be continued with closed sternum along with various positioning techniques and chest maneuvers (Chest Percussions and Vibrations). The main intention of applying all these techniques is to make the patient fit for extubation. Once the patient gets extubated, he may have following complications.
Post-ECMO complications
Prolonged controlled ventilation without diaphragmatic contraction may result in severe atrophy and increased duration of ventilatory support. Furthermore, the adverse effects of deep sedation and paralysis including bradycardia, ICU-acquired paresis, and ventilator-associated pneumonia pose valid concerns with reduction in lung volumes and capacities.
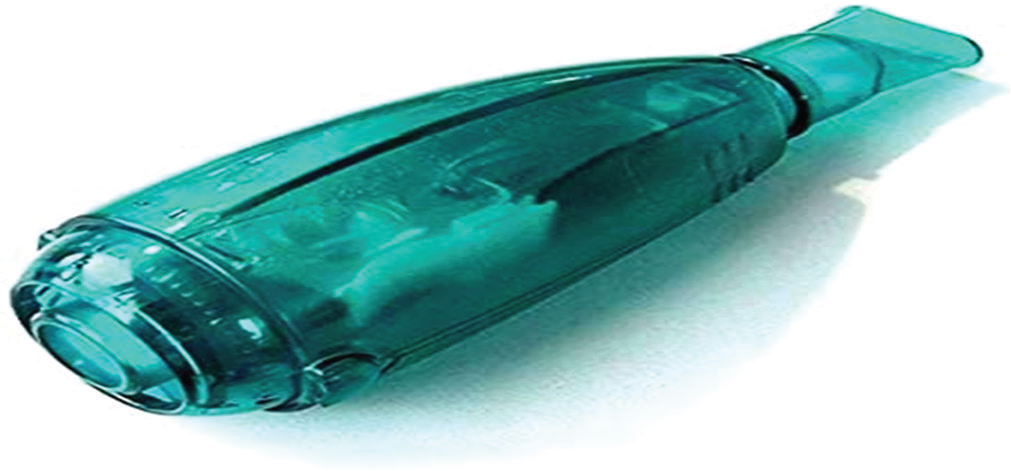
Acapella
One of the most frequently prescribed airway clearance technique (ACT) options for patients with chronic lung conditions or decreased lung volumes is positive expiratory pressure therapy (PEP) device (Acapella).
During PEP therapy, the patient exhales against a fixed-orifice resistor, generating pressures during expiration that usually range from 10 to 20 cm H2O. PEP does not require a pressurized external gas source.
The therapy which is administered by breathing through a special device helps:
Air get behind the mucus
Move mucus from lung and airway walls
To hold the airways open for longer.
MECHANISM OF PEP
The increase in pressure is transmitted to airways creating back pressure stenting them during exhalation, preventing premature airway closure and reducing gas trapping
Promotes collateral ventilation, allowing pressure to build up distal to the obstruction (collateral ventilation is a phenomenon found in the human lungs where alveolar structures are ventilated through channels that bypass normal airways)
Retains airways from collapsing and prolongs expiratory flow
Effective airway clearance promotes movement of mucus proximally
Also when a patient breathes out. The vibrations move mucus from the surface of the airways. After blowing through the device several times, the person will huff and cough to clear the mucus from the lung also create vibrations.[1]
INDICATIONS FOR PEP
Acute and chronic respiratory failure for reasons of surgery
Neurological or musculoskeletal dysfunction, for example, MND
Old age and immobility
To increase lung volume by increasing forced residual capacity (FRC) and tidal volume (VT)
Reduce hyperinflation/air trapping in, for example: Emphysema, bronchitis, and asthma[2]
Improve airway clearance in; cystic fibrosis (over 4 y.o); chronic bronchitis; bronchiectasis; and bronchiolitis obliterans
To maximize the delivery of bronchodilators in patient’s receiving bronchial hygiene therapy.
RELATIVE CONTRAINDICATIONS FOR PEP[3,4]
Untreated pneumothorax
Intracranial pressure >20 mm Hg
Active hemoptysis
Recent trauma or surgery to skull, face, mouth, or esophagus
Patient with acute asthma attack or acute worsening of chronic obstructive pulmonary disease unable to tolerate increased work of breathing
Acute sinusitis or epistaxis
Tympanic membrane rupture or other known or suspected inner ear pathology
Nausea.
There are no absolute contraindications to PEP that have been noted by the literature.
PHYSIOLOGY OF PEP
Increasing lung volume FRC and VT
A progressively temporary increase in FRC has been found to be proportionally correlated when increasing PEP
An increase in FRC is attained by alteration of breathing pattern that is a product of a decrease in expiratory flow and an increase in expiratory time leading to exhalation of smaller volumes
Lung volume increase is achieved by altering breathing pattern, thereby increasing VT and decreasing respiratory frequency, which is due to an increase in muscle activity of inspiratory and expiratory muscles
Improved gas exchange is a result of breathing during a prolonged period with normalized lung volumes.[5-7]
Reduction of hyperinflation
Hyperinflation is a result of air entrapment causing the lungs to over inflate. It is caused by muscle spasm, mucosal inflammation, hyper-secretions, and reduced lung elasticity due to destruction of lung parenchyma. If untreated may lead to inspiratory muscle exhaustion, decreased ventilation, and deficient gas exchange
PEP reduces expiratory flow, which in return decreases the declining pressure across the airway wall thereby reducing collapse
Increasing pressure within airways transports expiratory positive pressure (EPP) centrally and in stable airways therefore stenting them. Reduction of airway collapse increases expired volume leading to additional emptying of lung volume thus lowering FRC and improving ventilation distribution and gas exchange.
Airway clearance
It homogeneously mobilizes secretions in collapsed airways. It aims toward increasing FRC by recruiting collapsed lung volumes and uses resistance to obtain progressive homogenization emptying of the lungs
Homogenization is achieved by the facilitation of EPP to move peripherally during expiration avoiding collapsed airways, trapped gas, and atelectasis. This results in reduction of respiratory flow and an increase in expiratory flow combined with an increase in FRC. In doing so secretion is mobilized in closed or collapsed and unreachable parts of the lungs
The oscillating property is achieved by bursts and turbulent expiratory airflow due to the opening and closing of the valve. Oscillations during expiration decrease the viscoelasticity properties of mucus, affecting its movement which depends on the oscillating frequency. OscPEP is equally as effective as other Airway Clearance Technique (ACT) as PEP and Active Cycle Breathing Technique.
INSTRUCTIONS FOR THE USE OF PEP DEVICES
Physiotherapist will set device to the amount of pressure needed (Can be used as an adjunct to Active Cycle of Breathing Technique).
Instructions
Repeat below steps at least 5 times to make one cycle. Repeat the following steps as many times as directed to complete one cycle:
Loosen mucus
Sit up with your back straight and your chin slightly up. This position allows your throat to be open so air can move easily without blockage
You may need to put your elbows on a table. This may keep you from slouching and blocking air from moving freely
Take a deep breath and hold it for 2–3 s
While you hold your breath, place the mouthpiece in your mouth
Breathe out at a steady rate for 4–6 s or as long as you can. Keep your cheeks as flat as possible. You may have to use your fingers to hold your cheeks down. Try not to cough
You may be able to keep the mouthpiece in, or your mask on, as you repeat. Take a deep breath in through your nose.
Cough and bring up mucus
Remove the mouthpiece from your mouth or the mask
Do 2–3 huff coughs. Take a deep breath in. Use your stomach muscles to breathe out 3 quick, forceful breaths. Make a ha, ha, ha sound[7,8]
Then, cough hard to bring up mucus. Spit the mucus out. Do not swallow the mucus
You may need to rest for 1–2 min
This cycle should continue for 10–20 min or until you have cleared all your sputum.
SCIENTIFIC LITERATURE ABOUT PEP
Following meta-analyses of the effects of PEP versus other airway clearance techniques on lung function and patient preference, a review demonstrated that there was a significant reduction in pulmonary exacerbations in people using PEP where exacerbation rate was a primary outcome measure.[9]
Another review suggests that PEP therapy appears to have similar effects on health-related quality of life, symptoms of breathlessness, sputum expectoration, and lung volumes compared to other ACTs when prescribed within a stable clinical state or during an acute exacerbation.[10]
A systematic review investigated the effect of PEP breathing after an open upper abdominal or thoracic surgery. Questionable quality standards, different protocols, and PEP devices used among the six RCTs included concur to uncertainty about PEP effect. It is not possible to assume that a prophylactic chest physiotherapy treatment is superior to a PEP device protocol in preventing within 5-day post-operative complications.
DISCUSSION
Limited evidences are available regarding effectiveness of various rehabilitative interventions or techniques in post-ECMO rehabilitation. However, in context of subjects receiving ECMO, the PEP therapy through Acapella may be effective to overcome pulmonary complications and respiratory muscle weakness post-ECMO decannulation, as Acapella therapy is backed by several evidences related to the similar complications. Hence, the effectiveness of Acapella needs to be explored further in post-ECMO rehabilitation program.
CONCLUSION
Limited evidences are available regarding effectiveness of various rehabilitative interventions or techniques in post ECMO Cardio-Pulmonary Rehabilitation. However in context of subjects receiving ECMO , the the PEP Therapy via Acapella may be effective to overcome pulmonary complications and respiratory muscle weakness post ECMO decannulation, as Acapella therapy is backed by several evidences related to the similar complications.On the other hand the patients receiving routine Cardiopulmonary Physiotherapy Rehabilitation Program: (1) positioning; (2) passive range of motion (PROM) training; (3) neuromuscular electrical stimulation (NMES); (4) surface electrical phrenic nerve stimulation (SEPNS); (5) respiratory proprioceptive neuromuscular facilitation (PNF) techniques; and (6) airway clearance techniques also got some benefit. So the effectiveness of Acapella needs to be explored further in post ECMO Rehabilitation Program along with routine Cardiopulmonary rehabilitation Program.
Declaration of patient consent
Patient’s consent not required as their identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Airway Clearance Therapy In: The Comprehensive Respiratory Therapist Exam Review (6th ed). St. Louis, Missouri: Elsevier; 2016.
- [Google Scholar]
- Cincinnati Children's. Available from: https://www.cincinnatichildrens.org/health/b/bubble-PEP [Last accessed on 20198 Jun 05]
- [Google Scholar]
- Available from: https://www.acapella-pep.com/acapella-choice-easy-to-clean-pep-device_p_14.html [Last accessed on 2022 Dec 30]
- RC Use of Positive Airway Pressure Adjuncts to Bronchial Hygiene Therapy Journal. Available from: https://www.rcjournal.com/cpgs/papcpg.html [Last accessed on 2020 Sep 25]
- [Google Scholar]
- RT PEP Devices. Available from: https://www.rtmagazine.com/products-treatment/monitoring-treatment/therapy-devices/look-positive-expiratory-pressure-devices [Last accessed on 2020 Sep 25]
- [Google Scholar]
- Business Wire Worldwide Oscillating Positive Expiratory Pressure Devices Industry to 2025 North America Dominates the Market-Research and Markets. Available from: https://www.businesswire.com/news/home/20200826005648/en/worldwide-oscillating-positive-expiratory-pressure-devices-industry [Last accessed on 2020 Sep 09]
- [Google Scholar]
- Cadiovascular and Pulmonary Physical Therapy: Evidence and Practice (4th ed). St. Louis, MO: Mosby/Elsevier; 2006.
- [Google Scholar]
- Physiologic evidence for the efficacy of positive expiratory pressure as an airway clearance technique in patients with cystic fibrosis. Phys Ther. 2004;84:524-3.
- [CrossRef] [PubMed] [Google Scholar]
- Positive expiratory pressure-common clinical applications and physiological effects. Respir Med. 2015;105:297-307.
- [CrossRef] [PubMed] [Google Scholar]
- Positive expiratory pressure physiotherapy for airway clearance in people with cystic fibrosis. Cochrane Database Syst Rev. 2015;6:CD003147.
- [CrossRef] [PubMed] [Google Scholar]






