Translate this page into:
Peripartum Cardiomyopathy and Thrombosis – A Match Made In Hell!
*Corresponding author: Poonam Malhotra Kapoor, Department of Cardiac Anaesthesia and Critical Care, All India Institute of Medical Sciences, New Delhi, India. docpoonamaiims@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Badge M, Nagashweta LS, Rajgopalan K, Görlinger K, Kapoor PM. Peripartum Cardiomyopathy and Thrombosis – A Match Made In Hell! J Card Crit Care TSS. doi: 10.25259/JCCC_47_2024
Abstract
Pregnancy with peripartum cardiomyopathy (PPCM) is associated with a prothrombotic state. The procoagulant system is activated, signaled by the elevated levels of clotting factors. The natural anticoagulation mechanisms are suppressed, along with the fibrinolytic system. Heart failure (HF) is also known to activate platelets favoring thrombus formation. HF with reduced ejection fraction secondary to multi-factorial etiology in PPCM predisposes to intracardiac thrombus formation and embolic complication, jeopardizing maternal and fetal safety. Anticoagulation with heparin for thrombo-prophylaxis and treatment can prevent the formation and extension of the clot. Risk stratification, prompt identification of patients with intracardiac thrombus, and timely initiation of anticoagulation can mitigate the catastrophic thromboembolic episodes.
Keywords
Anticoagulation
Low-molecular-weight heparin
Peripartum cardiomyopathy
Thrombosis
Thromboembolism
INTRODUCTION
Pregnancy, a physiological process, is accompanied by adaptations in the maternal body orchestrated by hormonal changes for the thriving of the fetus till delivery. The hematological system also undergoes a transformation in all three major components – increased red cell mass, leukocytosis, and thrombocytopenia.[1] The hemostatic profile is also in constant flux throughout the gravid state. The levels of procoagulant factors such as fibrinogen, clotting factors, and vonWillebrand factors are elevated with increasing gestational age. At the other end of the spectrum, protein C and S concentrations dwindle, cumulatively leading to a hypercoagulable state.[2] Peripartum cardiomyopathy (PPCM), a rare type of dilated cardiomyopathy, is the commonest cause of heart failure (HF) in pregnancy. It is diagnosed in late pregnancy or within 6 months postpartum. The incidence is highest in African American women. The decrease in global ventricular systolic function and the prothrombotic state due to pregnancy further compounded by PPCM predisposes to stasis and risk of thromboembolic complications and maternal as well as fetal morbidity and mortality.
PPCM AND THROMBOSIS
PPCM significantly exaggerates the risk of both arterial and venous thromboembolism, which is evident from the high percentage (4–6%) of patients reported from various registries.[3] Pregnancy is a perfect scenario to replicate Virchow’s triad – hypercoagulability, venous stasis, and endothelial injury [Figure 1].[4] Recent research elucidating the pathophysiology of PPCM reveals the complex interplay between prolactin, oxidative stress, and soluble Fms-like tyrosine kinase-1 released from the placenta, inhibiting vascular endothelial growth factor promoting endothelial cell (EC) dysfunction. The 16 KiloDalton prolactin subfragment promotes micro ribonucleic acid-146a expression, induces EC apoptosis, promotes vasoconstriction, and inhibits EC migration and proliferation.[5] The hemostatic milieu is shifted toward a prothrombotic state, with an attenuated fibrinolytic system. The systolic dysfunction, cardiac chamber dilatation, and low cardiac output contribute to intracardiac blood stasis and thrombus formation.
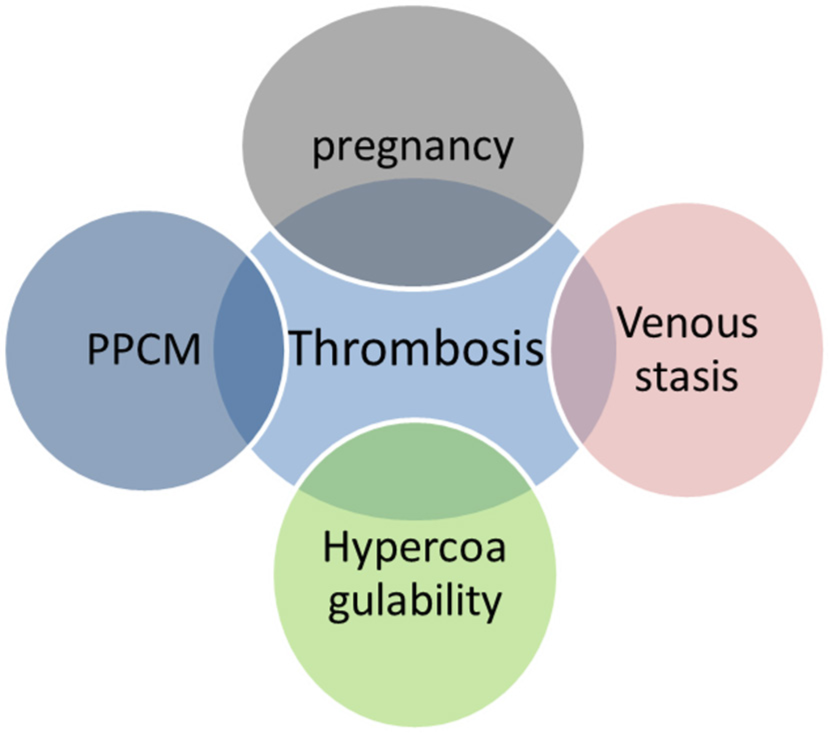
- Venn diagram depicting the inter-relationship between pregnancy, peripartum cardiomyopathy (PPCM), venous stasis, and hypercoagulability in thrombotic complications.
HF AND PLATELET DYSFUNCTION
Congestive HF is also associated with changes in platelets in the form of platelet activation. Consequently, there is whole blood aggregation, increased mean platelet volume, and elevated expression of platelet-bound and soluble p-selectin, platelet/EC adhesion molecules, and β-thromboglobulin.[6,7] Interacting with leukocytes and EC, they serve as mediators of inflammation. Platelet to leucocyte ratio particularly with monocytes and lymphocytes could usher as a novel marker of inflammation. PPCM is also a form of HF with reduced ejection fraction (EF). In a retrospective study, elevated platelet count was found to be associated with left ventricular (LV) thrombus formation.[8] Further studies are required to validate the role of platelet count and function for thrombosis in PPCM.
INDICATION FOR ANTICOAGULATION
There lacks an universal consensus on the threshold for administering anticoagulation in PPCM and the duration of treatment. Low EF is a major determinant of the necessity of anticoagulant use. The American Heart Association 2016 guidelines propagate anticoagulation in LVEF <30%.[9] The European Society of Cardiology (ESC) 2016 guidelines suggest using LVEF <35% as the cutoff value. Its 2019 position statement states the use of anticoagulation in prophylactic dose in reduced EF,[10] but “reduced EF” has not been specifically defined. Therapeutic anticoagulation is recommended in patients with visualization of intracardiac thrombus on imaging, systemic embolism, and paroxysmal or persistent atrial fibrillation. There are also conflicting data on bromocriptine used in the postpartum period aggravating the thrombotic risk including, cerebrovascular, and myocardial infarction. The ESC 2018 guideline on the management of cardiovascular diseases in pregnancy recommends prophylaxis with heparin in females on bromocriptine.[11]
ANTICOAGULATION DURING PREGNANCY AND POSTPARTUM
Heparin in both unfractionated and low-molecular-weight forms is the drug of choice for anticoagulation in pregnancy. Low–molecular-weight heparin (LMWH) is derived from the depolymerization of unfractionated heparin (UFH) resulting in the formation of fragments that are about one-third the size of UFH molecule.[12,13] These LMWHs, such as enoxaparin and dalteparin, also activate antithrombin III but predominantly act on factor Xa versus thrombin. Therefore, their activity is best monitored using anti-Xa assays and not with activated clotting time/activated partial thromboplastin time, as with UFH.[14,15] LMWH supersedes UFH due to its long half-life, allowing once or twice daily dose, predictable anticoagulation response, and decreased heparin-induced thrombocytopenia and heparin-induced osteoporosis incidence.[16] UFH is usually reserved for patients requiring urgent delivery, surgery, or thrombolysis.[17] Other anticoagulants have either an unacceptable risk of embryopathy or are not adequately evaluated in this population [Table 1]. However, Vitamin K antagonist can be employed post-delivery.
| Anticoagulant | Safety | Reason |
|---|---|---|
| LMWH | Data present supporting use in pregnancy | Do not cross placenta, dosing to be adjusted during delivery, and central neuraxial blockade |
| UFH | Data present supporting use in pregnancy | Do not cross placenta, shorter half-life, and preferred when urgent delivery is imminent |
| VKA | Avoided; Extreme caution in 2nd and 3rd trimester | Warfarin crosses placenta, embryopathy, and risk of fetal malformation |
| NOAC | Avoided | Contraindicated; scarce data |
| Synthetic Pentasaccharide | Avoided | Limited data to support use during LMWH allergy/adverse reactions |
LMWH: Low molecular weight heparin, UFH: Unfractionated heparin, VKA: Vitamin K antagonist, NOAC: Novel oral anticoagulants;  : Indicated;
: Indicated;  : Avoided
: Avoided
DISCUSSION
PPCM is a pro-thrombotic state, with a heightened risk of thrombosis during pregnancy. The thromboembolic risk continues unabated in the postpartum period, conspicuous from the prevalence of complications even after delivery. No cardiac chamber/great vessel are immune from thrombus formation. Intracardiac thrombus can develop in both the left (17%)[18] and right ventricle, atria, aorta, pulmonary artery, and superior vena cava. The major cause of morbidity and mortality is cerebrovascular embolism. Deep venous thrombosis and catastrophic pulmonary embolism have also been reported.[5,19] Biventricular thrombus was found in a 32 year, gravida seven patient, 2 months after delivery, echo revealed an EF of 15– 20%. She was treated with heparin infusion and subsequently transitioned to apixaban for 4 months.[20] In a retrospective study involving 123 PPCM patients, 22 were found to harbor intracardiac thrombus, after multivariable logistic regression analysis-LVEF, hemoglobin, and thrombocyte count were associated with the prediction of LV thrombus formation.[8] In another case, a 32-year-old postpartum patient suffered a cerebral infarct due to a large thrombus in the aortic root.[21] Comparatively lower thromboembolism episode (TEE) rates were observed in a population given thromboprophylaxis to a substantial percentage (16%) of patients.[22] Lower-segment cesarean section delivery and post-operative status were associated with higher TEE.
FUTURE RESEARCH AND DELIBERATIONS
The use of novel biomarkers in both diagnosis and prognosis in PPCM has been on a rising trend in the current decade.[23] Plasminogen Activator Inhibitor-1 (PAI-1) gene plays a crucial role in regulating fibrinolysis. Elevated levels of PAI-1 can increase the risk of thrombosis. PAI-1 has been studied for its potential role in vascular impairment through the urokinase plasminogen activator receptor/nuclear factor kappa B Cells (uPAR/NF-kB/miR-146a) pathway on endothelial activation. Polymorphism in the PAI-1 gene can decode the variability in the thrombotic episodes in PPCM. The 4G allele is associated with higher PAI-1 levels compared to the 5G allele.[24]
The pertinent questions that still remain unanswered with respect to anticoagulation – LVEF below which anticoagulation be initiated during pregnancy, duration of anticoagulation, and anticoagulant agent after postpartum. Although novel oral anticoagulants (NOAC’s) are used after delivery, the 2019 position statement of ESC mentions rivaroxaban being found in breast milk, although in a small amount in a single case study, mandating further confirmation of NOAC safety in the postpartum group.[25] With the current understanding of PPCM, serial echocardiograms in females with low EF can detect thrombus formation in the early stages, restricting its growth and chances of embolism. Thus, TEEs are a potential threat in PPCM and the use of LMWH can significantly decrease this risk.
CONCLUSION
Although substantial progress has been made in understanding of etiology, pathophysiology, and treatment options in PPCM, a major lacuna regarding identifying risk factors for TEE’s and optimal preventive and treatment strategies looms over safe pregnancy, puerperium, and postpartum period. Regular surveillance in high-risk patients can promote timely identification and initiation of thromboprophylaxis. Further prospective studies are required for risk stratification of pregnant females with PPCM benefiting from anticoagulation.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
Dr. Klaus Görlinger and Dr. Poonam Malhotra Kapoor are on the Editorial Board of the Journal. Dr. Klaus Görlinger works as the Medical Director of TEM Innovations/Werfen PBM, Munich, Germany.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Physiological Changes in Hematological Parameters during Pregnancy. Indian J Hematol Blood Transfus. 2012;28:144-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hematologic Findings in Pregnancy: A Guide for the Internist. Cureus. 2021;13:e15149.
- [CrossRef] [Google Scholar]
- Thromboembolism in Peripartum Cardiomyopathy: A Systematic Review. J Thorac Dis. 2024;16:645-60.
- [CrossRef] [PubMed] [Google Scholar]
- Venous Thromboembolism in Pregnancy: Challenges and Solutions. Vasc Health Risk Manag. 2023;19:469-84.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary Embolism in Patients Admitted With Peripartum Cardiomyopathy: Prevalence, Predictors, and Associated in-Hospital Adverse Events. Cureus. 2024;16:e60953.
- [CrossRef] [Google Scholar]
- The Impact of Platelet Indices on Clinical Outcome in Heart Failure: Results from the MyoVasc Study. ESC Heart Fail. 2021;8:2991-3001.
- [CrossRef] [PubMed] [Google Scholar]
- Coagulation Abnormalities in Heart Failure: Pathophysiology and Therapeutic Implications. Curr Heart Fail Rep. 2016;13:319-28.
- [CrossRef] [PubMed] [Google Scholar]
- Risk Factors for Intracardiac Thrombus in Peripartum Cardiomyopathy: A Retrospective Study in China. ESC Heart Fail. 2023;10:148-58.
- [CrossRef] [PubMed] [Google Scholar]
- Current Diagnostic and Treatment Strategies for Specific Dilated Cardiomyopathies: A Scientific Statement from the American Heart Association. Circulation. 2016;134:e579-646.
- [CrossRef] [Google Scholar]
- Peripartum Cardiomyopathy: From Genetics to Management. Eur Heart J. 2021;42:3094-102.
- [CrossRef] [PubMed] [Google Scholar]
- What is New in the 2018 ESC Guidelines for the Management of Cardiovascular Diseases during Pregnancy? Wien Klin Wochenschr. 2020;132:69-72.
- [CrossRef] [PubMed] [Google Scholar]
- Is Rotational Thromboelastometry the Answer for Rapid Prediction of Coagulopathy on Extracorporeal Membrane Oxygenation? J Card Crit Care TSS. 2017;1:108-10.
- [CrossRef] [Google Scholar]
- Viscoelastic Testing on Venoarterial Extracorporeal Membrane Oxygenation: Need or Greed? J Card Crit Care TSS. 2023;7:118-28.
- [CrossRef] [Google Scholar]
- Point-of-Care Testing at Acute Cardiac Care brings Positive Outcome. J Card Crit Care TSS. 2018;2:3-4.
- [CrossRef] [Google Scholar]
- Platelet Reactivity on ECMO: Role of VerifyNow. J Card Crit Care TSS. 2023;7:129-32.
- [CrossRef] [Google Scholar]
- Anticoagulation for Intra-cardiac Thrombi in Peripartum Cardiomyopathy: A Review of the Literature. Rev Cardiovasc Med. 2019;20:53-8.
- [CrossRef] [PubMed] [Google Scholar]
- Guidance for the Treatment and Prevention of Obstetric-associated Venous Thromboembolism. J Thromb Thrombolysis. 2016;41:92-128.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Characteristics and Long-term Predictors of Persistent Left Ventricular Systolic Dysfunction in Peripartum Cardiomyopathy. Can J Cardiol. 2016;32:362-8.
- [CrossRef] [PubMed] [Google Scholar]
- Improved outcomes in peripartum cardiomyopathy with contemporary. Am Heart J. 2006;152:509-13.
- [CrossRef] [PubMed] [Google Scholar]
- An Interesting Case of Peripartum Cardiomyopathy with Biventricular Thrombi. Cureus. 2023;15:e38748.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical Circulatory Support for the Management of Complex Peripartum Cardiomyopathy. JACC Case Rep. 2020;2:154-8.
- [CrossRef] [PubMed] [Google Scholar]
- Peripartum Cardiomyopathy in Iraq: Initial Registry-based Data and 6 Month Outcomes. ESC Heart Fail. 2021;8:4048-54.
- [CrossRef] [PubMed] [Google Scholar]
- Biomarkers in Peripartum Cardiomyopathy-What We Know and What Is Still to Be Found. Biomolecules. 2024;14:103.
- [CrossRef] [PubMed] [Google Scholar]
- In Peripartum Cardiomyopathy Plasminogen Activator Inhibitor-1 is a Potential New Biomarker with Controversial Roles. Cardiovasc Res. 2020;116:1875-86.
- [CrossRef] [PubMed] [Google Scholar]
- Pathophysiology, Diagnosis and Management of Peripartum Cardiomyopathy: A Position Statement from the Heart Failure Association of the European Society of Cardiology Study Group on Peripartum Cardiomyopathy. Eur J Heart Fail. 2019;21:827-43.
- [CrossRef] [PubMed] [Google Scholar]






