Translate this page into:
Isolated Headache as a Symptom of the Acute Coronary Syndrome in a Case following Myocardial Revascularization
Chinmaya Nanda, MD, FIACTA Medanta Institute of Critical Care and Anaesthesiology, Medanta the Medicity Sector 38, Gurgaon, Haryana 122001 India nandachinu@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Retrosternal chest pain is the classical symptom of acute coronary syndrome (ACS). ACS sometimes presents with atypical symptoms and very rarely as headache as the only symptom. We present here a case where a patient who had undergone coronary artery bypass grafting presented with headache and on evaluation found to have complete occlusion of right coronary artery.
Keywords
acute coronary syndrome
International Classification of Headache Disorders
coronary artery disease
right coronary artery
coronary artery bypass grafting
Introduction
Acute coronary syndrome (ACS) classically presents as retrosternal pain that radiates to the left arm. It may sometimes present atypically as indigestion, pain in the back, neck or jaw, otalgia, facial pain, or syncope. Headache as the isolated symptom of coronary ischemia is very rare. Sampson and Cheitlin1 reported that only 6% of 150 patients with angina pectoris complained of headache and it was not the sole symptom.
Classification of Headache Disorders (International Classification of Headache Disorders) 20042 codes cardiac cephalgia to 10.6 in the group of secondary headaches attributed to disorders of homeostasis. Lipton et al3 in 1997 proposed the term cardiac cephalgia.
Case Report
A 55-year-old man was admitted to our hospital with a history of recent inferior wall myocardial infarction with angioplasty of right coronary artery (RCA) 2 weeks back. Coronary angiography done at that time showed discrete lesions with critical left main coronary artery stenosis and significant blockage in obtuse marginal artery. The RCA following angioplasty had no further narrowing and did not require additional revascularization. The patient was planned for coronary artery bypass grafting (CABG). Preoperative echocardiography (ECHO) revealed hypokinesia of posterior wall and akinetic inferior wall with left ventricular ejection fraction of 45%. The patient underwent off-pump CABG with reversed saphenous venous grafts to the left anterior descending and obtuse marginal artery. Patient was started on dual antiplatelets aspirin and clopidogrel after extubation. On the 7th postoperative day, the patient complained of sudden onset severe headache at rest that was not relieved with intake of nonsteroidal anti-inflammatory agent. Headache was not associated with blurring of vision and gait disturbance. Patient was conscious, oriented, and had no motor deficit. A computed tomography head without contrast was done that was unremarkable. Patient was not on nitrates. A 12-lead electrocardiogram (ECG) showed no fresh changes. Transthoracic ECHO performed on the patient showed akinetic posterior wall, inferior wall, and mid basal interventricular septum with an ejection fraction of 35%. In view of the new regional wall motion abnormalities, the patient was shifted to the cardiac catheterization laboratory. Angiography showed thrombus over the previously stented RCA (Fig. 1). Thrombectomy and stenting of RCA were done. Headache was relieved after revascularization.
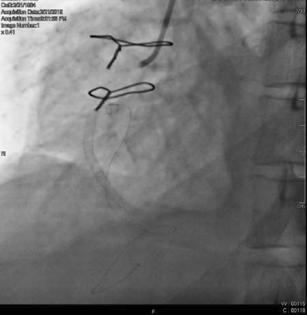
- Complete occlusion of right coronary artery post-revascularization.
Discussion
Atypical presentation of coronary artery disease (CAD) is not uncommon and is seen in females and diabetics. Headache as an isolated symptom of CAD is rare and difficult to diagnose. Bini et al4 reviewed 30 cases of cardiac cephalgia reported in literature. In cardiac cephalgia, the headache is not well defined. Pain is not localized in a specific area and it can be unilateral or bilateral. Headache is mostly severe in nature and resembles migraine. In 27% cases, headache was the only symptom of coronary ischemia and 57% cases showed pathological changes in ECG5 and elevation of cardiac enzymes.6 Most of the cases of cardiac cephalgia are seen in males and associated with anterior infarcts.7
The case reported by us had few peculiarities. This patient had normal ECG at rest but showed new regional wall motion abnormalities. Our case had involvement of RCA as against most of the cases reported in literature involving anterior infarcts. This might be the only case of cardiac cephalgia seen after myocardial revascularization.
Diagnosis of ACS in the presence of isolated headache is very difficult. Older age of presentation, associated risk factors of CAD, absence of previous history of headache, and onset of headache with exertion and relief after taking rest could be useful pointers to lead to the diagnosis of ACS. The intention of publishing this case report is to increase awareness among physicians, intensivist, and emergency room doctors that headache can be the sole symptom of ACS which is underrecognized and underreported. Acute graft thrombosis resulting in postoperative myocardial infarction is common, but they uncommonly present with headache as the sole symptom. Knowledge of cardiac cephalgia is less prevalent among physicians because it is rare in incidence and headache is not given an equal weightage of a cause of ACS. Aortic dissection should also be a differential diagnosis in patients with acute onset headache in whom any intracranial source of headache is not found.8 Prioritizing neurological workup in these cases can cause delay in diagnosis and adverse events.
Conflict of Interest
None declared.
References
- Pathophysiology and differential diagnosis of cardiac pain. Prog Cardiovasc Dis. 1971;13(6):507-531.
- [Google Scholar]
- The International Classification of Headache Disorders. 2nd edition. Cephalalgia. 2004;24(01):1-160.
- [Google Scholar]
- Cardiac cephalgia: a treatable form of exertional headache. Neurology. 1997;49(3):813-816.
- [Google Scholar]
- Severe explosive headache: a sole presentation of acute myocardial infarction in a young man. Am J Emerg Med. 2007;25(2):250-251.
- [Google Scholar]
- Acute non-ST-elevation myocardial infarction presented as occipital headache with impaired level of consciousness–a case report. Angiology. 2005;56(5):627-630.
- [Google Scholar]
- Temporoparietal headache as the initial presenting symptom of a massive aortic dissection. Case Rep Emerg Med. 2015;2015:626825.
- [Google Scholar]






