Translate this page into:
Euglycemic Diabetic Ketoacidosis with SGLT2 Inhibitor Therapy in a Patient Undergoing Off-Pump Coronary Artery Bypass: A Case Report
*Corresponding author: Rohini Mayur Balaji, Department of Cardiac Anesthesia, Apollo Hospitals, Trichy, Tamil Nadu, India. rohinimayur.b@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Balaji RM, Bhumana S, Sundarraj S, Kalyanasundaram A. Euglycemic Diabetic Ketoacidosis with SGLT2 Inhibitor Therapy in a Patient Undergoing Off Pump Coronary Artery Bypass: A Case Report. J Card Crit Care TSS. 10.25259/JCCC_73_2023 doi: 10.25259/JCCC_73_2023
Abstract
Sodium-glucose cotransporter inhibitors are a class of oral hypoglycemic agents that are being increasingly used in the subset of patients with cardiovascular disease. Euglycemic diabetic ketoacidosis (EDKA) is a potentially uncommon side effect associated with their use, which requires prompt recognition and management. The authors present a case of a 66-year-old diabetic male patient, treated with dapagliflozin, undergoing coronary artery bypass grafting, who developed EDKA in the postoperative period. The classical signs and symptoms were absent as the patient was sedated and was on ventilator support. Persistent high anion gap acidosis in the absence of hemodynamic instability prompted further testing, which revealed ketosis and ketonuria. Treatment with a dextrose-insulin solution and cessation of further doses of dapagliflozin leads to an uneventful recovery and discharge. A high index of suspicion is warranted, especially in the setting of cardiac surgery, for the diagnosis and management of this potentially catastrophic complication.
Keywords
Euglycemic diabetic ketoacidosis
Post-cardiac surgery
Sodium-glucose cotransporter-2 inhibitors
Dapagliflozin
Cardiac critical care
INTRODUCTION
Euglycemic diabetic ketoacidosis (EDKA) is a rare, potentially life-threatening complication that is associated with both type 1 and type 2 diabetes. It is characterized by the triad of high anion gap metabolic acidosis (ph <7.3, serum bicarbonate <18 mEq/L), ketosis and/or ketonuria, and euglycemia (blood glucose <200 mg/dL).[1] The incidence of EDKA is reported to be 2.6–3.2% among all admissions for diabetic ketoacidosis (DKA).[2] Various stressors in the perioperative period, such as fasting, surgical stress, gastroparesis, and infections, can trigger this phenomenon.[3,4] The use of a newer class of oral hypoglycemic agents (OHAs) and sodium-glucose cotransporter-2 inhibitors (SGLT2i) is specifically known to be associated with EDKA.[5] It poses a diagnostic challenge for clinicians as the underlying euglycemia masks the true diagnosis of ketoacidosis, especially in the setting of cardiac surgery, where acidosis has a multifactorial origin.
The authors present a case of EDKA occurring in the immediate postoperative period after off-pump coronary artery bypass (OPCAB) grafting surgery while the patient was still sedated and on ventilator support, a period during which clinical signs and symptoms may be absent.
CASE REPORT
A 66-year-old male patient presented to the emergency department with complaints of recurrent chest pain. On admission, his blood pressure was 180/90 mmHg, and his heart rate was 70 beats/min. Height and weight recorded were 168 cm and 68 kg, respectively. An ECG on admission was suggestive of myocardial ischemia. His coronary angiogram revealed a 90% distal left main coronary artery stenosis with proximal 90% stenosis of the left anterior descending (LAD) artery, diagonal and left circumflex arteries, and distal total occlusion of the right coronary artery. His echocardiogram revealed an ejection fraction of 40%, with hypokinesia of the anterior wall and apex of the left ventricle, mild mitral, and tricuspid regurgitation.
His history was significant for type 2 diabetes mellitus, with blood sugar on admission being 195 mg/dL, with hemoglobin A1c of 8.8%, treated with dapagliflozin 10 mg once daily, sitagliptin with metformin (50 mg/500 mg) twice daily for 2 years. There was no alcohol/toxin intake or any sign of infection.
He received an intravenous infusion of nitroglycerin and heparin, after which he was symptomatically better. He was scheduled for a semi-emergent OPCAB the following day.
Induction and intubation were in accordance with institutional anesthesia protocol. The left internal mammary artery (LIMA) was harvested, and adequate heparinization was confirmed before grafting. LIMA was anastomosed to the obtuse marginal, and the saphenous venous graft was anastomosed to the mid-LAD. Reversal of heparinization was done with protamine post-grafting. The intraoperative period was uneventful with the arterial blood gases (ABGs) being satisfactory at the end of surgery. The patient was shifted to the post-operative intensive care unit (ICU) without any inotropic support.
As the patient had moderate left ventricular dysfunction, and serial ABGs revealed progressive high anion gap acidosis, he was electively ventilated overnight. Serial lactates were <2 mmol/L, and the hemodynamics were stable, not requiring inotropic support, without any signs of low cardiac output.
Persistent acidosis, despite stable hemodynamics and the absence of any other obvious antecedent cause, prompted testing the patient’s urine and blood samples for ketones. Urine ketones were positive, and the blood ketone value was 4.9 (>1.5 – signifying risk of DKA). A provisional diagnosis of EDKA was made, and the patient was treated with a fluid bolus of 1 L 5% dextrose solution with 20 units of intravenous short-acting insulin over 1 h. This was followed by maintenance fluid at 150 mL/h and insulin infusion of 0.1 units/kg/h for a period of 6 h. The central venous pressure before fluid resuscitation was 6 mmHg and increased to 8 mmHg by the end of 6 h. Serial monitoring comprised glucose measurement every 2nd h, ABG every 3rd h, and potassium every 6th h. Blood gases analyzed after the resuscitation showed an improvement in the pH, increasing bicarbonate and decreasing anion gap levels. Blood sugar levels at all times remained below 200 mg/dL [Figures 1-3].
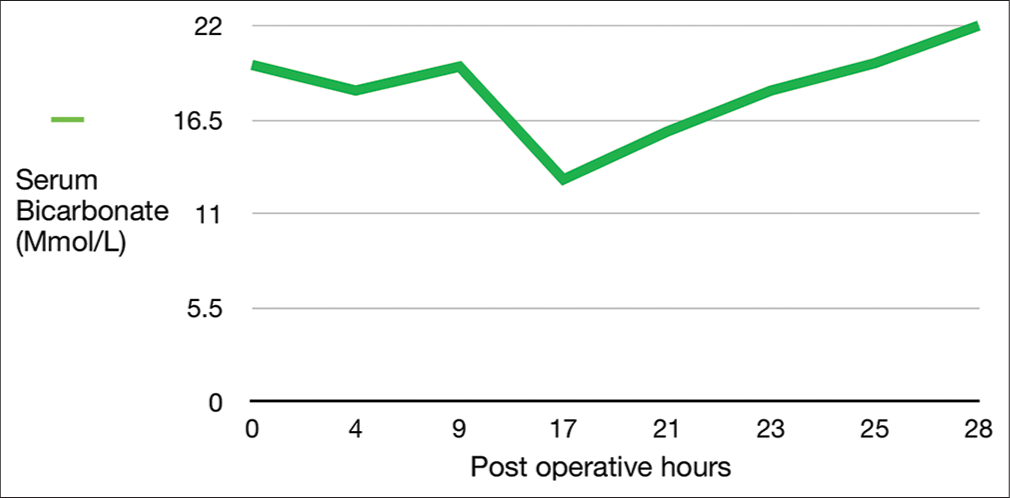
- Serum bicarbonate level.
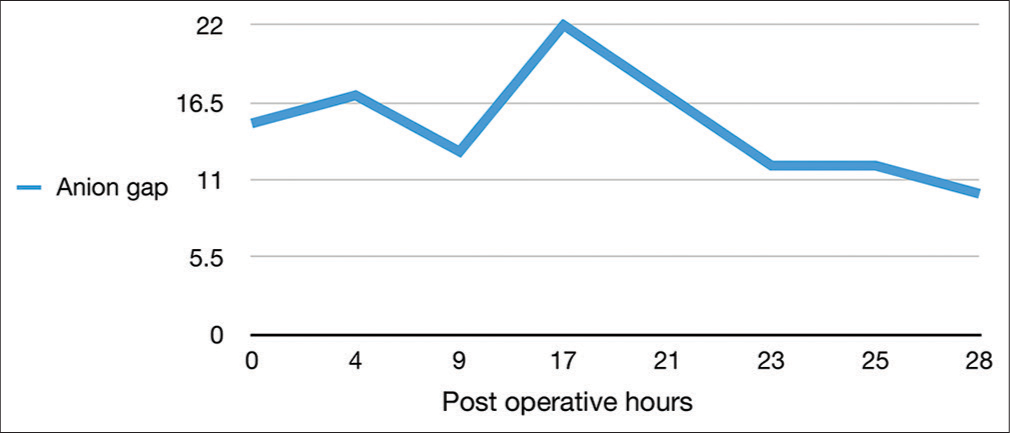
- Anion gap.
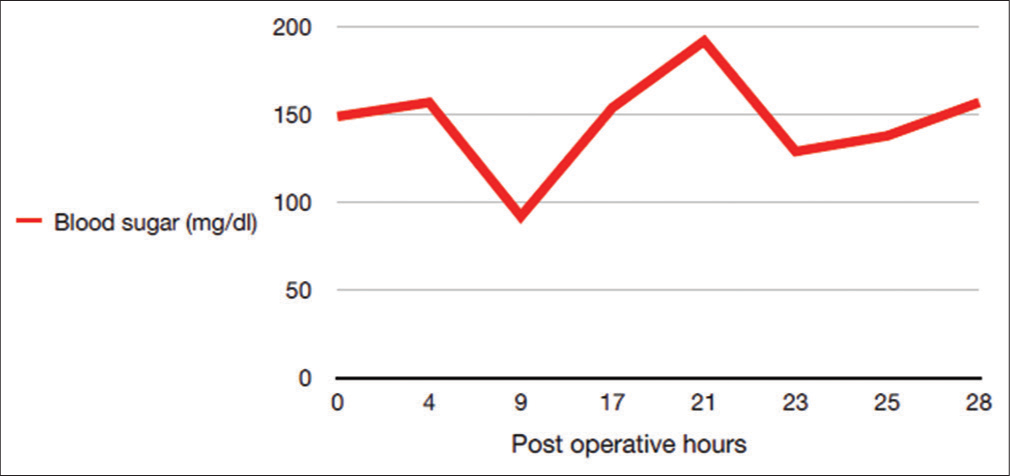
- Blood sugar level.
The patient was extubated post-resuscitation after confirming a satisfactory spontaneous breathing trial and subsequent ABG analysis. The urine output and the drain for the first 24 postoperative hours were 4 L and 1.2 L, respectively. A repeat blood and urine ketones at 48 h were negative. The rest of the ICU and hospital stay was uneventful. The patient was discharged on the 6th postoperative day.
DISCUSSION
SGLT2i are OHAs that act on the renal proximal convoluted tubules to prevent reabsorption of filtered glucose from the tubular lumen. They cause a reduction in blood sugar levels and improvement in glycated hemoglobin by causing glycosuria. Their use also results in natriuresis and inhibition of the sympathetic nervous system resulting in a favorable effect on blood pressure.[6,7]
Gliflozins have been shown to possess a probable role in mitigating the effects of inflammatory markers resulting in a reduction of fibrosis and oxidative stress in myocardial and renal tissue.[8,9] The natriuretic effect has been shown to decrease the ventricular preload and wall stress, which results in better indices of diastolic function.[10] Various recent trials such as the Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure trial and Empagliflozin Outcome Trial in Patients with Chronic Heart Failure with Reduced Ejection Fraction (HFrEF) have shown up to 25% reduction in hospitalizations due to heart failure and a reduction in cardiovascular mortality with SGLT2i use. This has led to the incorporation of these drugs as a Class 1 recommendation according to ACC/AHA guidelines for use in symptomatic patients who have HFrEF.[11-13] This translates to an increasing subset of patients requiring cardiac surgery who are treated preoperatively with gliflozins.
However, SGLT2i has been associated with side effects such as increased risk for genitourinary infections, acute kidney injury, ketoacidosis, and hypotension. Ketoacidosis has been attributed to increased glucagon secretion as a result of lower blood glucose levels requiring lesser insulin therapy and also a possible decreased elimination of urine ketones.[14,15]
Patients undergoing cardiac surgery develop metabolic acidosis due to various reasons, most commonly being large volume shifts requiring crystalloid administration, hypotension and subsequent tissue hypoperfusion, inotrope use, impaired glucose metabolism, and associated liver and kidney disorders.[16,17] In the perioperative cardiovascular surgical setting, it is challenging to attribute the cause of acidosis to DKA in the absence of hyperglycemia. In the absence of a high index of suspicion, it could be potentially fatal.[18]
Food and Drug Administration adverse event reporting system reported a 7-fold increase in the risk of developing ketoacidosis in patients treated with SGLT2i, of whom 71% had euglycemic ketoacidosis.[19] Murugesan et al., in their retrospective study consisting of 24 diabetic cardiac surgical patients treated with SGLT2i, show a similar incidence.[18]
There have been various recommendations regarding the pre-operative cessation of these drugs, ranging from 3 to 5 days.[20,21] In our patient, since the surgery had to be scheduled on a semi-emergency basis, there was an inadequate period of discontinuation of dapagliflozin in the pre-operative period. Furthermore, since the blood glucose level was <150 mg/dL at all times, insulin therapy was not started in the perioperative period. The symptoms of DKA, such as abdominal pain, vomiting, polyuria, and polydipsia, were absent as the patient was sedated and on ventilator support, being predisposed to an enhanced catabolic postoperative state, which led to a delay in the diagnosis until the 1st postoperative day.[22]
The authors opine that it may be imperative to routinely check blood and urine ketones in all patients on SGLT2i as standard care of practice on the day before surgery and also at clinically determined regular intervals till discharge from ICU. Retaining a high index of suspicion, prompt use of fluids and insulin, and intensive monitoring are invaluable in the prevention of catastrophic outcomes.
CONCLUSION
Due to compelling evidence available, a large proportion of diabetic patients undergoing cardiac surgery are likely to be on long-term SGLT2i therapy. A thorough history, optimal pre-operative discontinuation of the drug, regular monitoring for urine and blood ketones, prompt insulin, and fluid therapy in the setting of normoglycemia are paramount for the diagnosis and management of EDKA.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as the patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Euglycemic Diabetic Ketoacidosis: A Review. Curr Diabetes Rev. 2017;13:315-21.
- [CrossRef] [PubMed] [Google Scholar]
- Euglycemic Diabetic Ketoacidosis In: StatPearls. Treasure Island: StatPearls Publishing; 2022.
- [Google Scholar]
- SGLT2 Inhibitors: A Systematic Review of Diabetic Ketoacidosis and Related Risk Factors in the Primary Literature. Pharmacotherapy. 2017;37:187-94.
- [CrossRef] [PubMed] [Google Scholar]
- SGLT2 Inhibitor-Induced Euglycemic Diabetic Ketoacidosis: A Case Report. Kidney Med. 2020;2:218-21.
- [CrossRef] [PubMed] [Google Scholar]
- Euglycemic Diabetic Ketoacidosis Associated With Sodium-Glucose Cotransporter-2 Inhibitors after Cardiac Surgery: A Review of Current Literature. J Cardiothorac Vasc Anesth. 2022;36:3877-86.
- [CrossRef] [PubMed] [Google Scholar]
- Renal Effects of SGLT2 Inhibitors: An Update. Curr Opin Nephrol Hypertens. 2020;29:190-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sodium-Glucose Cotransporter 2 Inhibitors Mechanisms of Action: A Review. Front Med (Lausanne). 2021;8:777861.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of SGLT2 Inhibitors on Systemic and Tissue Low-grade Inflammation: The Potential Contribution to Diabetes Complications and Cardiovascular Disease. Diabetes Metab. 2018;44:457-64.
- [CrossRef] [PubMed] [Google Scholar]
- Anti-inflammatory Effects of Empagliflozin and Gemigliptin on LPS-Stimulated Macrophage via the IKK/NF-κB, MKK7/JNK, and JAK2/STAT1 Signalling Pathways. J Immunol Res. 2021;2021:9944880.
- [CrossRef] [PubMed] [Google Scholar]
- Empagliflozin Reduces Cardiovascular Events, Mortality and Renal Events in Participants with Type 2 Diabetes after Coronary Artery Bypass Graft Surgery: Subanalysis of the EMPA-REG OUTCOME® Randomised Trial. Diabetologia. 2018;61:1712-23.
- [CrossRef] [PubMed] [Google Scholar]
- Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019;381:1995-2008.
- [CrossRef] [PubMed] [Google Scholar]
- Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med. 2021;385:1451-61.
- [CrossRef] [PubMed] [Google Scholar]
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guideline. Circulation. 2022;145:e895-1032.
- [CrossRef] [Google Scholar]
- Euglycemic Diabetic Ketoacidosis in a Sedated Patient after Coronary Artery Bypass Grafting: A Case Report and Literature Review. Case Rep Med. 2021;2021:2086520.
- [CrossRef] [PubMed] [Google Scholar]
- OP61-Metabolic Acidosis after Heart Surgery and Intraoperative Red Cell Salvage. J Cardiothorac Vasc Anesth. 2017;31:S81-2.
- [CrossRef] [Google Scholar]
- Management of Metabolic Acidosis in the Post-cardiac Surgical Patient. Clin Cardiol Cardiovasc Med. 2020;4:12-5.
- [CrossRef] [Google Scholar]
- A Retrospective Analysis of the Incidence, Outcome and Factors Associated with the Occurrence of Euglycemic Ketoacidosis in Diabetic Patients on Sodium Glucose Co-transporter-2 Inhibitors Undergoing Cardiac Surgery. Ann Card Anaesth. 2022;25:460-5.
- [CrossRef] [PubMed] [Google Scholar]
- Ketoacidosis Associated with SGLT2 Inhibitor Treatment: Analysis of FAERS Data. Diabetes Metab Res Rev. 2017;33 10.1002/dmrr.2924
- [CrossRef] [PubMed] [Google Scholar]
- SGLT2 Inhibitor-associated Diabetic Ketoacidosis: Clinical Review and Recommendations for Prevention and Diagnosis. Clin Ther. 2016;38:2654-64.
- [CrossRef] [PubMed] [Google Scholar]
- Euglycemic Diabetic Ketoacidosis Due to Sodium-glucose Cotransporter 2 Inhibitor Use in Two Patients Undergoing Pancreatectomy. J Pancreat Cancer. 2018;4:95-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Word-of-Caution against Euglycaemic DKA! Turk J Anaesthesiol Reanim. 2022;50:469-70.
- [CrossRef] [PubMed] [Google Scholar]






