Translate this page into:
The Importance of TEE Examination in Patients with Pseudoaneurysm of Arch of Aorta Post-TEVAR Procedure
Poonam Malhotra Kapoor, MD, DNB, MNAMS, FISCU (Hony), FIACTA (Hony), FTEE (Hony) Department of Cardiac Anaesthesia and Critical Care, All India Institute of Medical Sciences Ansari Nagar, New Delhi 110029 India drpoonamaiims@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 57-year-old male patient presented to the emergency department with acute onset severe and tearing pain in the back. He was a chronic smoker and was a known hypertensive. He was admitted in view of type B aortic dissection with entry tear distal to left subclavian artery (LSCA) and underwent thoracic endovascular aortic repair (TEVAR) procedure for the same. Two stents (34–30–200mm size, Ankura, Lifetech, Nanshan District, Shenzhen, China) were placed overlapping each other to cover the dissection flap starting from distal end of left common carotid artery to proximal part of celiac artery. Post-stenting, patient developed recurrent episodes of melena, abdominal distension, and fever that were managed conservatively. Two months later, a routine follow-up computed tomographic aortic angiography revealed a focal contrast filled outpouching (2.1*1.9cm) extending from the proximal part of endovascular stent with surrounding thrombosis from anterior wall of the aortic arch. On inspecting the arch vessels, an ostial occlusion of LSCA was also discovered. Routine blood investigations were all within normal limits. Two-dimensional echocardiography showed a normal biventricular function with concentric left ventricular hypertrophy. All valves were normal.
Keywords
aorta post-TEVAR procedure
pseudoaneurysm of aortic arch
TEE examination
Introduction
Case Report
A 57-year-old male patient presented to the emergency department with acute onset severe and tearing pain in the back. He was a chronic smoker and was a known hypertensive. He was admitted in view of type B aortic dissection with entry tear distal to left subclavian artery (LSCA) and underwent thoracic endovascular aortic repair (TEVAR) procedure for the same. Two stents (34–30–200mm, Ankura, Lifetech) were placed overlapping each other to cover the dissection flap starting from distal end of left common carotid artery (LCCA) to proximal part of celiac artery (Fig. 1). Post-stenting, patient developed recurrent episodes of melena, abdominal distension, and fever that were managed conservatively. Two months later, a routine follow-up computed tomography aortic angiography revealed a focal contrast-filled outpouching (2.1*1.9cm) extending from the proximal part of endovascular stent with surrounding thrombosis from anterior wall of the aortic arch. On inspecting the arch vessels, an ostial occlusion of LSCA was also discovered. Routine blood investigations were all within normal limits. Two-dimensional echocardiography showed a normal biventricular function with concentric left ventricular hypertrophy (LVH). All valves were normal.
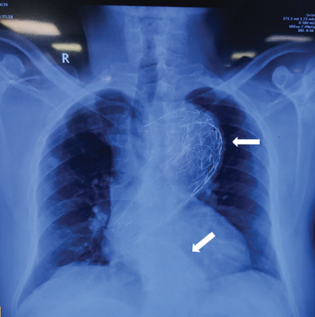
- Preoperative chest X-ray of the patient showing two stents (white arrow) in the descending thoracic aorta placed during the first thoracic endovascular aortic repair procedure for type B aortic dissection.
An interdisciplinary decision was made for type 1 debranching of the aortic arch vessels using a Y-shaped graft followed by TEVAR (Fig. 2). A preoperative anesthesia checkup was done. Oral anticoagulant was stopped 5 days prior and patient was shifted on to low molecular weight heparin that was stopped 24 hours prior to the day of surgery. Premedication was administered and patient was taken in the operating room. Anesthesia was induced with etomidate and rocuronium bromide. Maintenance was done using isoflurane with a mixture of air and oxygen. Near infrared spectroscopy (NIRS) electrodes were placed on the forehead of the patient to guide in cerebral regional saturation during the intraoperative course. After securing the endotracheal tube, a transesophageal echocardiogram (TEE) probe was inserted and continuous TEE examination was done during the whole procedure by well-experienced cardiac anesthesiologists.
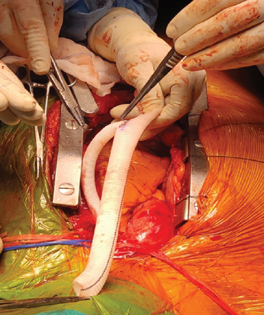
- The Y-shaped gel weave graft constructed for debranching of aortic arch vessels.
TEE examination showed the wall of the pseudoaneurysm in the arch of aorta. On color flow Doppler interrogation, there was no flow in this lumen. Endovascular stent was also visible on TEE. The flow to LSCA was compromised as demonstrated in TEE views. Surgically, a partial clamp was placed over the ascending aorta to help in the proximal anastomosis of the graft. The two distal anastomoses were done one after the other with a clamp time of 12 minutes for LCCA and 22 minutes for Innominate Artery (IA), respectively. NIRS values remained within the normal range throughout this procedure. After the anastomosis of the Y-shaped graft, hemostasis was confirmed and sternum closed (Fig. 3). Post-debranching procedure, TEE examination showed an improvement in the flow in the LSCA. LCCA and the IA did not have any significant gradient and the blood flow was adequate. The patient was then planned for a repeat TEVAR procedure to completely bypass the blood flowing in the pseudoaneurysm.
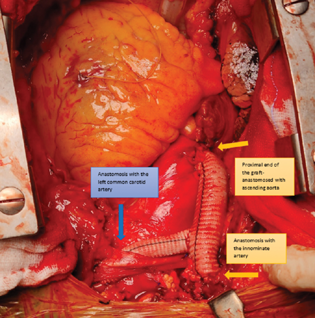
- Image showing the anastomotic sites of the 14mm graft from ascending aorta to innominate artery (yellow arrows) and 9mm graft to left common carotid artery (blue arrow).
Two days later, a redo TEVAR procedure was scheduled for the patient in the cardiology–radiology cath laboratory suite (Fig. 4). Patient was taken after a review preanesthesia checkup and general anesthesia was induced. The plan was to deploy another stent in the arch of aorta that would cut off the blood supply to the pseudoaneurysm.1, 2, 3, 4 A baseline angiography of the patient revealed the previous two aortic stents in situ along with the contrast filling the pseudoaneurysm. The Y-shaped graft was also visible in the angiography (Fig. 5). After confirming the location and size of the new stent to be placed, patient was heparinized and a 36 mm endovascular stent was taken. This was then carefully deployed over the previous 34 mm stent and oversized by 10% to cover the arch (Fig. 6). Therefore, the final stent in position covered the entire arch of aorta with the arch vessels being supplied by the surgically placed graft in situ.5, 6, 7

- Fluoroscopy image taken in cath laboratory showing the two aortic stents (black arrows) in situ along with sternal wires (red star) in the patient post-debranching surgery.
![Contrast-enhanced fluoroscopy image of the aorta demonstrating the bulge in the arch of the aorta-pseudoaneurysm (red outline and the filling up of the debranched aortic arch vessels [blue arrow]).](/content/149/2022/6/2/img/10-1055-s-0042-1756473-i2270003-5.png)
- Contrast-enhanced fluoroscopy image of the aorta demonstrating the bulge in the arch of the aorta-pseudoaneurysm (red outline and the filling up of the debranched aortic arch vessels [blue arrow]).
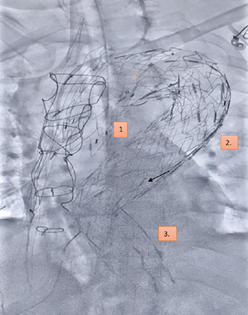
- Fluoroscopy image showing all three aortic stents (numbered) in situ after the successful deployment of the third stent in the redo thoracic endovascular aortic repair procedure, completely bypassing the blood flow in the pseudo aneurysm of the arch of aorta.
The patient was shifted to the intensive care unit following the procedure with the femoral sheaths. He was weaned from the ventilator and hemodynamically managed in the intensive care unit with special attention to avoid hypertension and sympathetic overdrive. As the consciousness was regained, muscle relaxation was reversed and trachea was extubated. Continuous invasive blood pressure monitoring with serial blood gas analysis and coagulation profile monitoring was done. Post-extubation, incentive spirometry and physiotherapy were ensued. Patient was gradually mobilized and shifted to the ward with stable vitals.
Conflict of Interest
None declared.
References
- Surgery for pseudoaneurysm of the ascending aorta: role of intraoperative 2-dimensional and real-time 3-dimensional transesophageal echocardiography. J Cardiothorac Vasc Anesth. 2010;24(5):906-908.
- [Google Scholar]
- Hybrid debranching and TEVAR of the aortic arch off-pump, in re-do patients with complicated chronic type-A aortic dissections: a critical report. J Cardiothorac Surg. 2013;8:188.
- [Google Scholar]
- Pseudoaneurysm as a late complication of chronic Stanford type A intramural hematoma requiring endovascular repair. JACC Case Rep. 2020;15:2470-2475.
- [Google Scholar]
- Traumatic aortic dissection pseudoaneurysm with multiple entry: role of transesophageal echocardiography. Ann Card Anaesth. 2018;21(4):427-429.
- [Google Scholar]
- Thoracic endovascular aortic repair for pseudoaneurysm after interrupted aortic arch repair. Ann Vasc Dis. 2018;11(4):549-552.
- [Google Scholar]
- Endovascular repair of an aortic arch pseudoaneurysm with double chimney stent grafts: a case report. J Cardiothorac Surg. 2013;8:80.
- [CrossRef] [Google Scholar]
- Endovascular treatment of thoracic aortic pseudoaneurysm through a subclavian approach in patient with aortoiliac occlusive disease: a case report. EJVES Short Rep. 2018;39:47-49.
- [Google Scholar]






