Translate this page into:
Innovative Troubleshooting of Difficult TEE Probe Insertion: Letter To Editor Response
Ashish Walian, MD, PDCC Department of Cardiac Anaesthesia, Atal Bihari Vajpayee Institute of Medical Sciences (ABVIMS) and Dr. Ram Manohar Lohia Hospital Baba Kharak Singh Marg, New Delhi 110001 India walian.ashish10@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Transesophageal echocardiography (TEE) is an integral component of modern-day cardiac surgical conduct.1 While TEE probe insertion is a relatively simple procedure usually successful in the first attempt, it is not sans risks particularly when difficulties are encountered while performing the same. The American Society of Echocardiography and Society of Cardiovascular Anesthesiologists outlines a complication rate of 0.03 to 1.2% with intraoperative or i-TEE.2 The consequences of trauma owing to multiple attempts at probe insertion can pose considerable concerns of oropharyngeal injury and/or bleeding.3, 4 This becomes further compounded in view of preoperative anticoagulants, systemic heparinization, and a predisposed patient profile (e.g., cyanotics).5
Centralizing the focus on the anatomical peculiarities, there are some potential sites of resistance to a smooth TEE probe insertion namely pyriform fossa and arytenoids.3, 6 Herein, simple positioning maneuvers can be instrumental in overcoming the same. Appropriate to the context, the SORT maneuver: (S)niffing position with an anteflexed probe (O)rientation, contralateral head (R)otation and probe (T)wisting, described by Najafi and Golzari, classifies as a noteworthy proposition for nasogastric tube (NGT) and TEE probe insertion.7 We present a case series highlighting the application of a modified version of the originally described maneuver to aid difficult TEE probe insertion in cardiac catheterization laboratory (CCL), followed by the use of the former in operation theater (OT) setting.
Case Series
Cases 1–5: CCL Setting
A 28-year-old male patient, chronic tobacco chewer, was posted for TEE-guided device closure of an atrial septal defect (ASD) in the CCL. His preoperative investigations and airway assessment were within normal limits. Following induction of general anesthesia and endotracheal tube (ETT) insertion, difficulty was encountered in TEE probe insertion despite jaw thrust and ETT cuff deflation. After three initial attempts by an experienced cardiac anesthesiologist, TEE probe insertion in the background of a modified SORT or the m-SORT maneuver was resorted to as an alternative plan or the plan B. Direct laryngoscopy-aided SORT-assisted TEE probe insertion was envisaged as the plan C. The m-SORT maneuver consisted of a jaw thrust combined with the SORT maneuver (Fig. 1A–D). We could subsequently negotiate the probe without encountering any undue resistance.
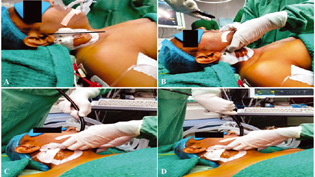
- Steps of SORT maneuver for transesophageal echocardiography (TEE) probe insertion. (A) (S)niffing position; (B) Anteflexed probe (O)rientation with jaw thrust; (C) Head (R)otation to the left; (D) (T)wisting movement with probe advancement.
The other four cases posted in CCL in whom m-SORT maneuver was applied had a similar demographic profile and underwent same procedure as the first case. In the second case, a 26-year-old female posted for TEE-guided ASD device closure, on encountering resistance to smooth insertion of TEE; we resorted to m-SORT maneuver and could easily insert the probe again. Prompted by the former, we routinely employed m-SORT maneuver for TEE-probe insertion in the subsequent three more patients posted for TEE-guided ASD device closure in the CCL. Interestingly, we could successfully achieve TEE probe insertion in the first attempt in all these patients.
Case 6: OT Setting
As an extension of the use of m-SORT maneuver for blind TEE probe insertion in the CCL, we performed SORT-assisted video-laryngoscope (VL)-guided TEE probe insertion in a 23-year-old female patient with chronic primary moderate mitral regurgitation posted for mitral valve repair. Motivated by the availability of VL in our OT (not available in CCL), we chose the aforementioned plan to delineate the plausible mechanisms by which SORT maneuver could come to rescue in circumstances of difficulty at TEE probe insertion (Fig. 2A, B).
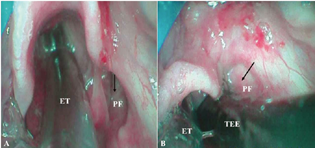
- Video laryngoscopic images of SORT-assisted TEE probe insertion. (A) Open pyriform fossa (indicated by black arrow) without SORT maneuver; (B) Obliterated pyriform fossa (indicated by black arrow) after SORT maneuver assisting smooth TEE probe insertion. ET, endotracheal tube; PF, pyriform fossa; TEE, transesophageal echocardiography probe.
In all the cases employing m-SORT maneuver, we not only could insert the probe easily but also there was no blood at the probe tip at the end of the procedure and, the patients did not complain of any postoperative throat pain or difficulty in swallowing, on follow-up.
Discussion
Hillenbrand et al review the techniques that can assist in TEE probe insertion, such as physical manipulations (lateral neck pressure, anterior cricoid displacement) and/or the use of laryngoscopy (direct/video) as the insertion aids.6 Talking of blind TEE probe insertion, maneuvering can be of particular importance wherein Najafi and Golzari SORT maneuver comprises of a comprehensive constellation of patient-related (Sniffing position and contralateral head rotation) and probe-related maneuvering (anteflexed probe orientation and twisting).7 However, the research group led by Najafi and Golzari publish a series of encouraging experiences with SORT maneuver primarily for NGT insertion.7, 8 They also give an unelaborated account of a successful TEE probe insertion utilizing SORT maneuver in an octogenarian undergoing coronary artery bypass grafting requiring TEE-guided decision making for concomitant mitral regurgitation.9
As far as our adaptation of the SORT maneuver or the m-SORT maneuver is concerned, the simultaneous inclusion of a forward jaw thrust can considerably help the TEE probe insertion procedure by widening the esophageal hiatus as elaborated by Jahangir et al in a cadaveric study.10 We speculate that the addition of a forward jaw thrust in the m-SORT maneuver can potentially become all the more relevant in background of loss of muscle tone in anesthetized patients. Moreover, head positioning can also play a pivotal role in successfully inserting a TEE probe. Aligned with the Mart and Rosen elucidation of a significant impact on the dimensions of the bilateral pyriform sinuses with head rotation,11 we also illustrate that contralateral head rotation obliterates the ipsilateral pyriform sinus thereby assisting a smooth TEE probe insertion (Fig. 2A, B). In addition, sniffing positioning thrusts away the arytenoid-cartilage from the esophageal aperture.
While m-SORT came to our rescue for blind TEE probe insertion in CCL (avoiding possible hemodynamic compromise attributable to a second laryngoscopy, relevant in a cardiac surgical cohort), there also exists literature to suggest an attenuated TEE probe tip-related injury in visually aided techniques.3 At the same time, presence of an ETT in situ also can also preclude direct visualization of the esophageal hiatus despite of using a Macintosh direct laryngoscope. Herein, Ishida et al describe an incremental value of McGRATH MAC VL for TEE probe insertion.12 Nonetheless, the role of optimal positioning and maneuvering cannot be undermined even in visually guided insertions let alone a blind method, as heralded in the index case series.
Hence, a stepwise approach to TEE insertion can be followed as to avoid any TEE-related complication where in the first step can be probe insertion using jaw-thrust, failing which m-SORT maneuver can be employed, and if this too is not successful, one can go in for m-SORT-assisted visually aided TEE probe insertion.
Conclusion
The aforementioned case series emerges as a motivation for the fraternity to be more innovative in troubleshooting a challenging TEE probe insertion. However, such maneuvering techniques necessitate further planned evaluation in larger prospective control studies.
Acknowledgment
Dr. Souvik Dey (Senior Resident, Department of Cardiac Anesthesia, Atal Bihari Vajpayee Institute of Medical Sciences (ABVIMS) and Dr. Ram Manohar Lohia Hospital) contributed in reviewing and editing the manuscript.
Conflict of Interest
First case was presented in ISACON 2021, Delhi chapter.
References
- Surgical-conundrum of a hiding ‘Bullet’: echocardiographic artefact clues the concealed fact! Indian J Anaesth. 2021;65(5):412-413.
- [Google Scholar]
- Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964.
- [Google Scholar]
- Rigid laryngoscope-assisted insertion of transesophageal echocardiography probe reduces oropharyngeal mucosal injury in anesthetized patients. Anesthesiology. 2009;110(1):38-40.
- [Google Scholar]
- Transesophageal echocardiography probe-induced hypopharyngeal and esophageal injury: a case report. J Cardiothorac Vasc Anesth. 2017;31(2):e42-e43.
- [Google Scholar]
- Bleeding in the lung complicates a routine intracardiac repair: what went wrong!!! Ann Card Anaesth. 2018;21(1):78-81.
- [Google Scholar]
- Difficult TEE probe placement: the evidence, troubleshooting techniques, and a guide to alternative monitoring options for intraoperative physicians. Semin Cardiothorac Vasc Anesth. 2019;23(4):369-378.
- [Google Scholar]
- Nasogastric tube insertion easily done: the SORT maneuver. Indian J Crit Care Med. 2016;20(8):492-493.
- [Google Scholar]
- Nasogastric tube insertion: the simple yet impossible [Internet] Atlas of Science another view on science. [cited 2021 December 09]. Accessed March 28, 2022 from
- [Publisher] [Google Scholar]
- Visually guided TEE probe insertion, making a case based on anatomic variation: a cadaveric study. Echocardiography. 2018;35(10):1616-1620.
- [Google Scholar]
- Optimal head position during transesophageal echocardiographic probe insertion for pediatric patients weighing up to 10 kg. Pediatr Cardiol. 2009;30(4):441-446.
- [Google Scholar]
- McGRATH MAC video laryngoscope for insertion of a transoesophageal echocardiography probe: a randomised controlled trial. Eur J Anaesthesiol. 2016;33(4):263-268.
- [Google Scholar]






