Translate this page into:
Role of ECMO in E-CPR
*Corresponding author: Jumana Yusuf Haji, Consultant, Cardiac Critical care, Sir H. N. Reliance Foundation Hospital, Mumbai, Maharashtra, India. drjyhaji@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Haji JY, Singh R. Role of ECMO in E-CPR. J Card Crit Care TSS 2023;7:25-31.
Abstract
Extracorporeal cardiopulmonary resuscitation (ECPR) is the implantation of venoarterial extracorporeal membrane oxygenation (VA-ECMO) in a patient who experienced a sudden and unexpected pulseless condition attributable to cessation of cardiac mechanical activity. The aim of ECPR is to provide adequate perfusion to the end organs when the potentially “reversible” conditions were managed. ECPRs are mostly done in tertiary care center in India. There is little scope for out of hospital arrest as poor quality of CPR and response time exists with lack of awareness about ECPR, which hinders its wider usage even in IHCA. Emergency department doctors need to be involved to counsel, recognize candidates activate, and initiate ECPR.
Keywords
E-CPR
Conventional CPR
extracorporeal CPR
INTRODUCTION
Extracorporeal cardiopulmonary resuscitation (ECPR) is the implantation of venoarterial extracorporeal membrane oxygenation (VA-ECMO) in a patient who experienced a sudden and unexpected pulseless condition attributable to cessation of cardiac mechanical activity. The aim of ECPR is to provide adequate perfusion to the end organs when the potentially “reversible” conditions were managed. ECPR is a resource-intensive therapy requiring specialized equipment and highly trained multidisciplinary experts which have usually limited to large centers with adequate facility. On the basis of ELSO registry, a ten-fold increase of ECPR procedures has been registered in the past 10 years. ECPR, as shown in [Figure 1] can be both for in hospital cardiac arrest (IHCA) and out of hospital cardiac arrest (OHCA).[1] ECPR is the application of ECMO in patients, where conventional cardiopulmonary resuscitation (CCPR) measures are unsuccessful in achieving a sustained return of spontaneous circulation (ROSC) (Sustained ROSC is deemed to have occurred when chest compressions are not required for 20 consecutive min following cardiac arrest [CA].)[2] It provides time for the delivery of interventions necessary to regain an adequate native circulation. These may include percutaneous coronary intervention (PCI) and recovery from myocardial stunning, pulmonary thrombectomy, rewarming, or toxin clearance. ECPR is a time sensitive, complex intervention that requires teamwork, clearly defined roles, and well-trained health-care providers.[3]
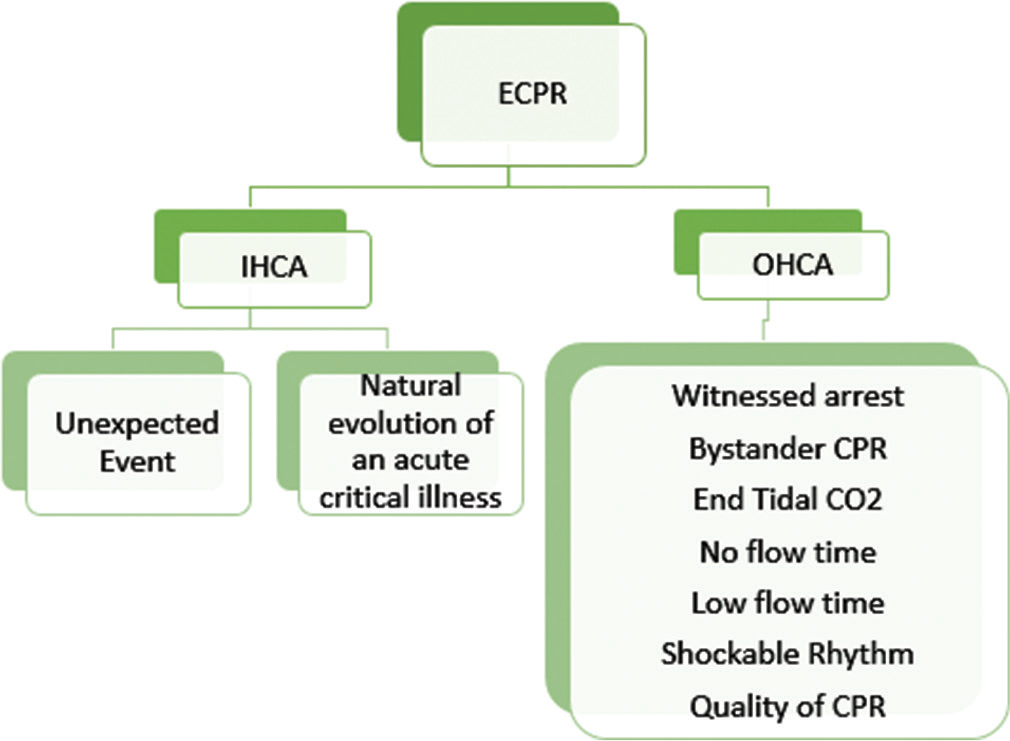
- ECPR for both in hospital and out of hospital cardiac arrest. ECPR: Extracorporeal cardiopulmonary resuscitation.
NO FLOW TIME AND LOW-FLOW TIME IN ECPR
The uncertainty in the preliminary diagnosis drives the uncertainty in eligibility criteria for ECPR at all times, 24/7 a team experienced in emergent ECMO implantation on a patient in CA during continuous chest compressions is essential for successful ECPR. Timely, ECPR certainly scores over (CCPR) [Figure 2].
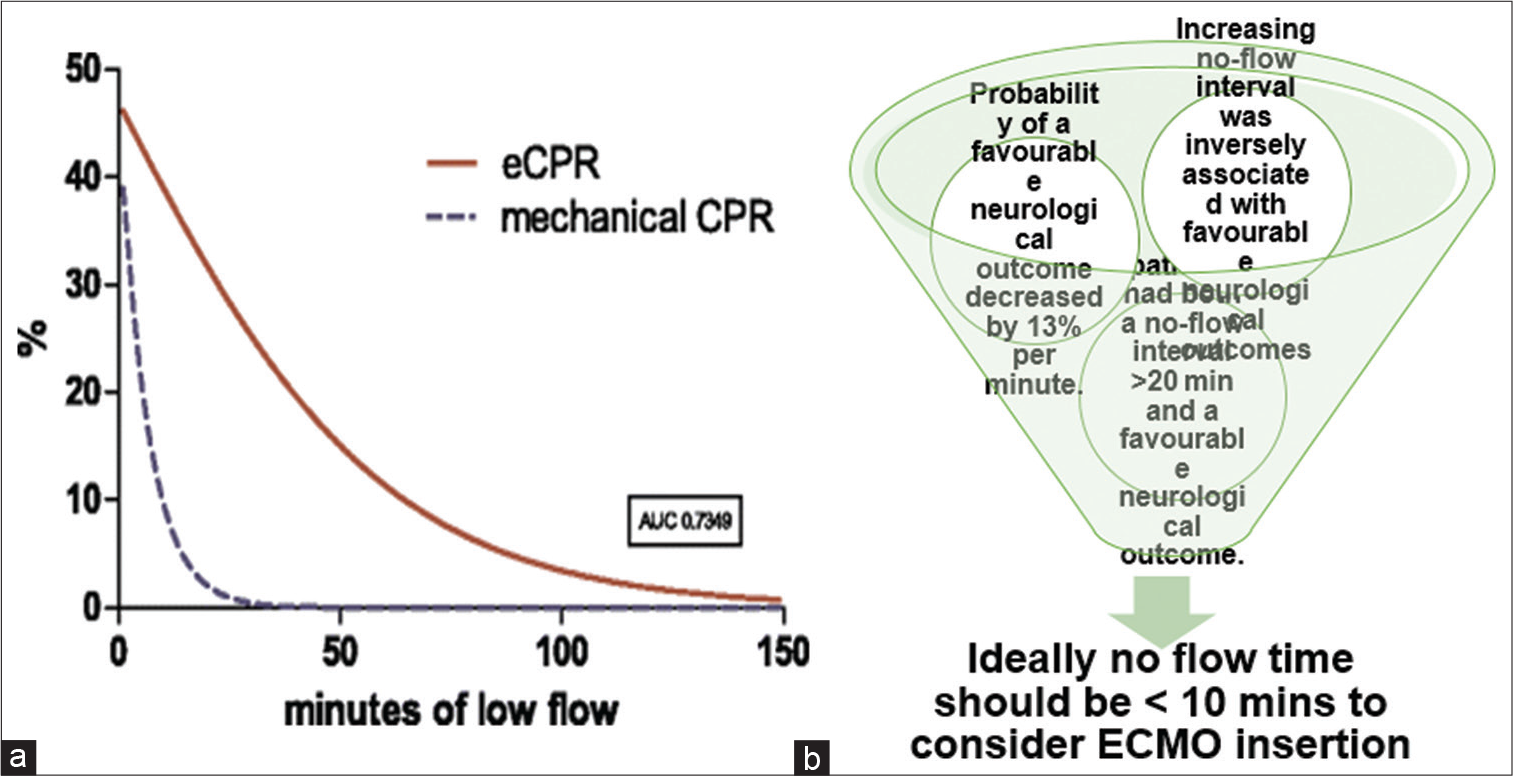
- (a) No flow time – Time to start of good quality CPR and low-flow time – time to start of ECMO. (b) Estimated survival rates for extracorporeal membrane oxygenation (ECPR) patients after every given low-flow time (red line). ECMO: Extracorporeal membrane oxygenation, ECPR: Extracorporeal cardiopulmonary resuscitation.
Factors influencing the outcomes of ECPR
Patient factors Quality of CCPR
Center’s experience
Type of mechanical device used
Resource availability
Indices used to determine the outcome.
Bar plots show the relation between ECPR duration and survival to discharge or good neurological outcomes at discharge [Figure 3] when ECPR is performed at <20 min of CCP. The time required to establish ECMO support is highly dependent on the capabilities of the resuscitation team and patient factors. It may be achieved in as little as 10 min but may take longer.[4] We, therefore, advise early assessment for ECPR candidacy. It is reasonable to consider commencing cannulation after 10–20 min of failed resuscitation efforts. Beyond 20 min of refractory arrest, the probability of ROSC and survival with CCPR is <5 %.[5,6] The risks of VA-ECMO and ECPR at this point, with appropriately selected patients and providers, may be justified. The “No Flow” interval in ECPR is the time from OHCA to cardiopulmonary resuscitation (CPR). It is one of the most important determinants of outcomes after out of hospital cardiac arrest (OHCA). The low-flow time on ECPR refers to [Figure 2a and b].
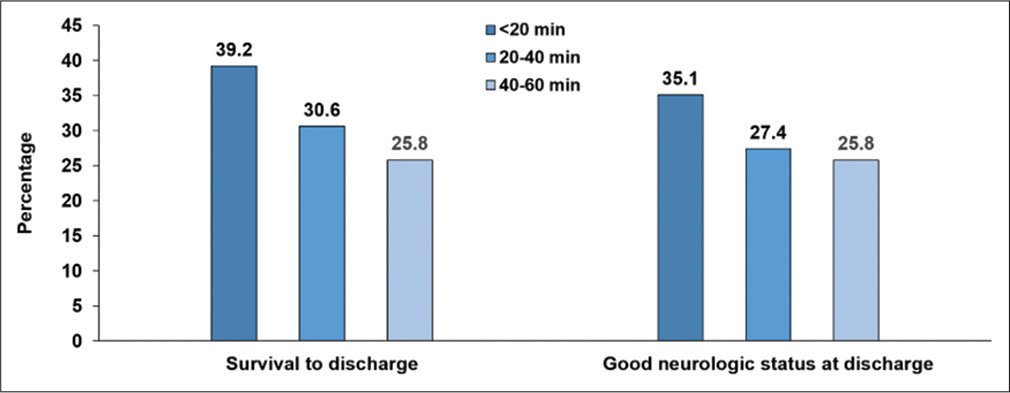
- Relation between ECPR duration and clinical outcomes. ECPR: Extracorporeal cardiopulmonary resuscitation.
Holmberg et al., in 2018, in their systematic review of 25 observational studies for the International Liaison Committee on Resuscitation’s Advanced Life Support and Pediatric Task Forces concluded that there is no conclusive evidence for or against the use of ECPR in IHCA and OHCA [Figures 4 and 5]. The studies in the systematic review had very low quality of evidence. Richardson et al., in 2017, reported 29% survival to hospital discharge in their study on 1796 ECPR patients. It is an international multicenter study done comparing ECPR patient’s outcome between 2003 and 2006 versus 2007 and 2010 versus 2011 and 2014. Risk-adjusted survival in all the three groups is the same, even though the comorbidities are higher over a period of time and also there are significant advancements in ECMO technology. The CHEER trial in 2015 showed a survival of 45% and 60% in OHCA and IHCA, respectively, following ECPR with reasonable neurological outcome. In the same year, Siao et al. studied various factors comparing conventional CPR (40 patients) and ECPR (20 patients). The overall survival at discharge with good neurological recovery was 35% and 18.3% in the ECPR and CCPR groups, respectively. The mean duration was longer in the ECPR group (69.90 ± 49.6 min) when compared with the CCPR group (34.3 ± 17.7 min) with P-value of 0.0001. About 95% in the ECPR group had more sustained ROSC, whereas the CCPR group had sustained ROSC only in 47.5% of their patients (P = 0.0009). Furthermore, good neurological outcome reported was 40% versus 7.5% in the ECPR versus CCPR groups (P = 0.0067), respectively. Matsuok et al., in their population-based study in 2019, reported an overall survival of 46.3% (87/188) and 20.3% (67/330) in the ECPR and CCPR groups, respectively, out of 518 patients studied. They also reported a favorable neurological outcome of 22.9% (43/188) in the ECPR group as against 8.5% (28/330) in the CCPR group. Dalia et al. reported his single-center experience in 2020. They reported a hospital survival of 33.8% in their 71 patients who underwent ECPR. Another important observation they made is that those patients requiring renal replacement therapy after ECPR had the highest mortality with only 5.3% surviving discharge from the hospital. In the same year, MacLaren et al. compared outcomes of various ECPR studies. In their comparison, the survival to hospital discharge of ECPR patients following OHCA ranged from 8% to 33%. In IHCA, it ranges between 19% and 60%. Various other studies also showed improved neurological outcome and survival following ECPR compared with CCPR.

- ECMO CART location in ICU and OT should be known to all the ECPR team. ECMO: Extracorporeal membrane oxygenation, ECPR: Extracorporeal cardiopulmonary resuscitation.

- Tertiary care center ECPR team being briefed about the cardiac anesthesia patients for ECPR. ECPR: Extracorporeal cardiopulmonary resuscitation.
IHCA AND ECPR
The indications for ECPR include following: Patients with IHCA refractory to ACLS treatment AND in whom the cause may be reversible; the patient with suspected acute coronary syndrome, who arrests in the ER; does not respond to standard ACLS and the cause is likely to be reversible with treatment in the cardiac catheterization laboratory; the patient in the cardiac catheterization laboratory undergoing coronary angiography who suffers a CA and who does not immediately respond to standard ACLS. The patient with suspected massive pulmonary embolism; intractable sudden onset VT VF not responding to conventional treatment due to metabolic or ischemic causes; and any other cause where there is likely to be reversibility of the underlying condition if an artificial circulation can be provided.
Complication of the initial emergent application and from those remaining on the extracorporeal oxygenation circuit includes the following. Vascular injury during cannulation aberrant placement of the cannula and unsuccessful cannulation, bleeding, leg ischemia, pneumonia, sepsis, and intracranial bleed/stroke. Post-resuscitation care all post-resuscitation targets easier to achieve post. ECPR oxygenation target CO2 target MAP target Therapeutic Hypothermia Transport for interventions and investigations.
METHOD OF ECPR AS PER CHEER TRIAL
Mechanical chest compressions using the auto pulse. Rapid intravenous administration of 30 mL/kg of ice-cold saline to induce hypothermia. Target is applied temperature of 33°C maintained for 24 h and then slow rewarming (0.24C/h). ECMO percutaneous cannulation of the femoral artery and vein by two critical care physicians and commencement of veno-arterial ECMO. Early reperfusion with urgent PCI is the key to ECPR success.
All the patients had witnessed IHCA since factors were not normalizing in 24 h there factor predict poor outcomes which are acidosis, serum lactate rising, renal failure, and liver failure [Tables 1-7 and Figure 4].
| • The access cannula position should be confirmed with fluoroscopy or echocardiography before cannula securing and dressing. The tip of the drainage cannula should be positioned in the right atrium. Both cannulas should be secured once an acceptable position is achieved. • Mean arterial pressure measurement: This is best achieved with a right-sided upper limb arterial line (radial or brachial). Right upper limb blood gas sampling gives the easiest indicator of native circulation PaO2 which may represent the cerebral oxygen delivery depending on the mixing point in the aorta between native circulation and VA-ECMO blood flow.[7] • An optimal MAP target following ECPR has not been identified. We recommend titrating vasopressors to MAP target ≥60 mmHg for organ perfusion pressure and<80 mmHg to minimize risk of LV distension. • Titrate sweep gas flow mechanical ventilation if ROSC has occurred by frequent arterial blood gases monitoring to avoid hypercarbia. • Address potential drainage insufficiency (drainage line chatter) with fluids/transfusion/weaning of VA-ECMO blood flow if excess to requirement; total circulation is made up of native cardiac output, if present, plus ECMO blood flow. • Ensure correct placement of endotracheal tube. • Central venous access. • Sedation and analgesia. • Perform bedside ultrasound: cardiac, thoracic, and abdominal imaging to identify possible complications (pneumothorax and thoracic/abdominal bleeding) and assess valve competence and LV distension. • Temperature monitoring and control. • Lead ECG. • Chest x-ray. • Establish end-tidal CO2 monitoring to assess native cardiopulmonary circulation. • Formal laboratory bloods including cross match. |
MAP: Mean arterial pressure, LV: Left ventricular, ECPR: Extracorporeal cardiopulmonary resuscitation, VA-ECMO: Venoarterial extracorporeal membrane oxygenation
| Authors | Year | Types of study | Population | Conclusion | ||
|---|---|---|---|---|---|---|
| Holmberg et al.[8] | 2018 | Systematic review of 25 observational studies for the ILCOR, advanced life support and pediatric task forces | NA | No conclusion evidences for or against the use of ECPR IHCA and OHCA | ||
| Richardson et al.[9] | 2017 | International multicenter study done comparing ECPR patients outcomes between 2003 and 2006 versus 2007 and 2010 versus 2011 and 2014 | 1796 ECPR patients | 29% survival to hospital discharge. Survival in all the three groups is the same, though the comorbidities are higher over a period of time and significant advancement in ECMO technology | ||
| CHEER trail | 2015 | Prospective pilot observational study single center | 26 patients 11°CHA and 15 IHCA | Survival of 45% and 60% in OHCA and IHCA, respectively, following ECPR with reasonable neurological outcomes. | ||
| Siao et al.[10] | 2015 | Comparing convention all CPR (40 patients) and ECPR 20 patients | Survival to discharge | ECPR 35% | CCPR 18% | |
| More sustained ROSC | ECPR 95% | CCPR 47.5% | ||||
| Duration | ECPR 69.90+49.6 min | CCPR 34.3+17.7 min | ||||
| Favorable neurological outcome | ECPR 40% | CCPR 7.5% | ||||
| Matsuok et al.[11] | 2019 | Population based study | 518 patients | Survival | 46.3% (87/188) | 20.3% (67/330 |
| Favorable neurological outcome | ECPR 22.9% (43/188) | CCPR 8.5% (28/330 | ||||
| Dalia et al.[12] | 2020 | Single-center experience | 71 patients who underwent ECPR | Hospital survival of 33.8%. RRT after ECPR had the highest mortality risk (only 5.3% surviving discharge from the hospital) | ||
| MacLaren et al.[13] | 2020 | Compared outcomes of various ECPR studies | NA | Survival to hospital discharge of ECPR patients following OHCA ranged from 8% to 33%. IHCA, it ranges between 19% and 60%. | ||
| ELSO Registry | 2020 | Data entry from all ELSO centers | Total runs | Survived ECLS | Survived to discharge | |
| Neonatal | 2035 | 1427 (70%) | 861 (42%) | |||
| Pediatric | 4945 | 2940 (59%) | 2086 (42%) | |||
| Adult | 8075 | 3363 (41%) | 2387 (29%) | |||
ILCOR: International Liaison Committee on Resuscitation’s, ECPR: Extracorporeal cardiopulmonary resuscitation, ICHA: In hospital cardiac arrest, OHCA: Out hospital cardiac arrest, CCPR: Conventional cardiopulmonary resuscitation
| • The CA is likely to be of primary cardiac or respiratory cause • The CA was witnessed by a bystander or paramedic • Chest compressions were commenced within 10 min • The CA duration (collapse to arrival at ER) has been<60 min • The patient is aged between 12 and 70 years • There are no major comorbidities that would preclude return to independent living • The patient is profoundly hypothermic (<32°C) due to accidental exposure • The patient has taken a significant overdose of a vaso-active drug (s) (e.g., beta-blocker, tricyclic acid, and digoxin) • Any other cause where there is likely to be reversibility of the CA if an artificial circulation can be provided. |
ECPR: Extracorporeal cardiopulmonary resuscitation, CA: Cardiac arrest
| • Premorbid severe neurological impairment including stroke, dementia, and traumatic brain injury • Shock thought to be secondary to sepsis or hemorrhage • Chest compressions not initiated within 10 min of commencement of cardiac arrest • Total arrest time >60 min • The presence of a valid “not for resuscitation” order • No realistic prospect of reversal of underlying cardiac or respiratory pathology • Advanced age precludes an extended ICU admission requiring mechanical support • No appropriately trained or equipped staff available to initiate ECPR. |
ECPR: Extracorporeal cardiopulmonary resuscitation
| Neurological • Reduced oxygen delivery to the brain • Reperfusion injury after establishing adequate oxygenation • Can be predicted using serial neurospecific enolase after 48 h of CA. Cardiac Stunning • Imbalance in the cellular calcium concentration • Calcium, vasodilators, cardiac pacing, and left ventricular decompression. |
| Number of ECMOs | ECPRs | Separated from ECMO | Survived to hospital discharge | Down time |
|---|---|---|---|---|
| 186 | 11 (5.6%) | 6 (54.5%) | 5 (45.5%) | 36–84 min |
ECPR: Extracorporeal cardiopulmonary resuscitation, ECMO: Extracorporeal membrane oxygenation
| It can be placed in one of the following places • Cardiac catheterization laboratory • Intensive care unit • Operating room • Emergency departments |
CREATE AN INTERDISCIPLINARY CLINICAL GROUP OF EXTRACORPOREAL LIFE SUPPORT MEMBERS DEDICATED TO PERFORMING ECPR
Cardiothoracic surgeons and intensivists take the role of ECMO specialists. Dedicated intensive care unit to manage these patients. Prepare ECMO cart – Preassembled ECMO circuit, serial dilators, cannulas of various sizes, antiseptic solutions, surgical drapes, surgical aprons, gloves, a surgical tray for vascular access, surgical blades, suture materials, and ECMO consent forms developed an ECPR kit which contains all the essential materials that can be wheeled into the ECPR site for rapid ECPR initiation. Prepare order sets – for every process and every workforce to follow through each stage of the ECMO run. Prepare ECMO activation pathway – ECMO alert in addition to code blue for activation of specialists and preparation for receiving patient in allocated locations for ECMO activation.
FINANCIAL CONSIDERATIONS OF ECPR
Cost-effectiveness in ECPR along with the quality of life analysis remains a financial constraints of ECPR. Cost-effectiveness of ECPR after IHCA remains a dilemma. The Markov decision model. Conclusion – Their study concluded cost-effectiveness in favor of ECPR, as shown in [Flowchart 1].
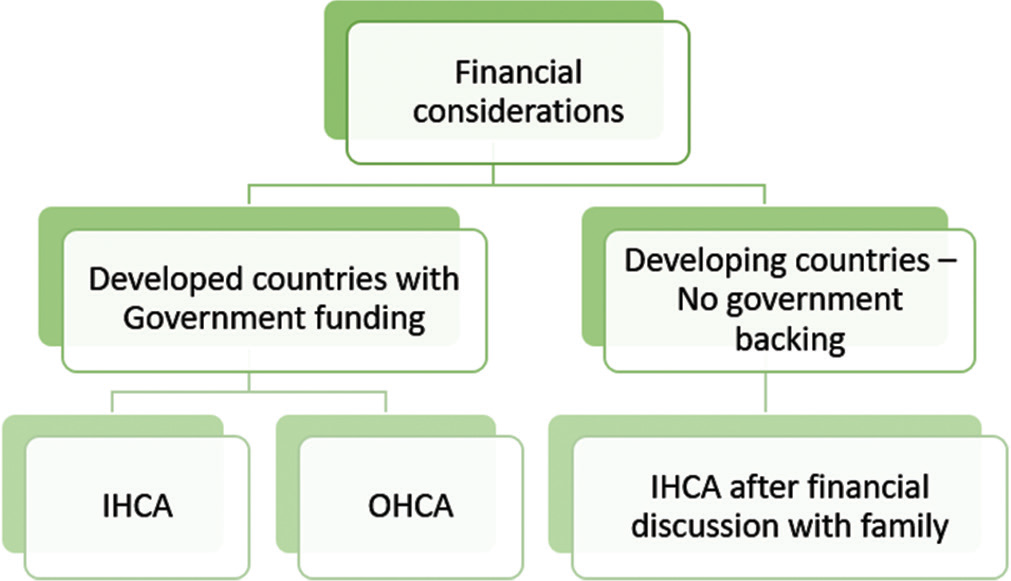
- The Markov model favor ECPR. ECPR: Extracorporeal cardiopulmonary resuscitation.
ETHICAL AND LEGAL CONSIDERATIONS ARE AT THE FOREFRONT
In the acute setting of ECPR as a bridge to decision and bridge to whatever seems reasonable including “withdrawal” after a few days, if no survival chances exist in [Flowchart 2].
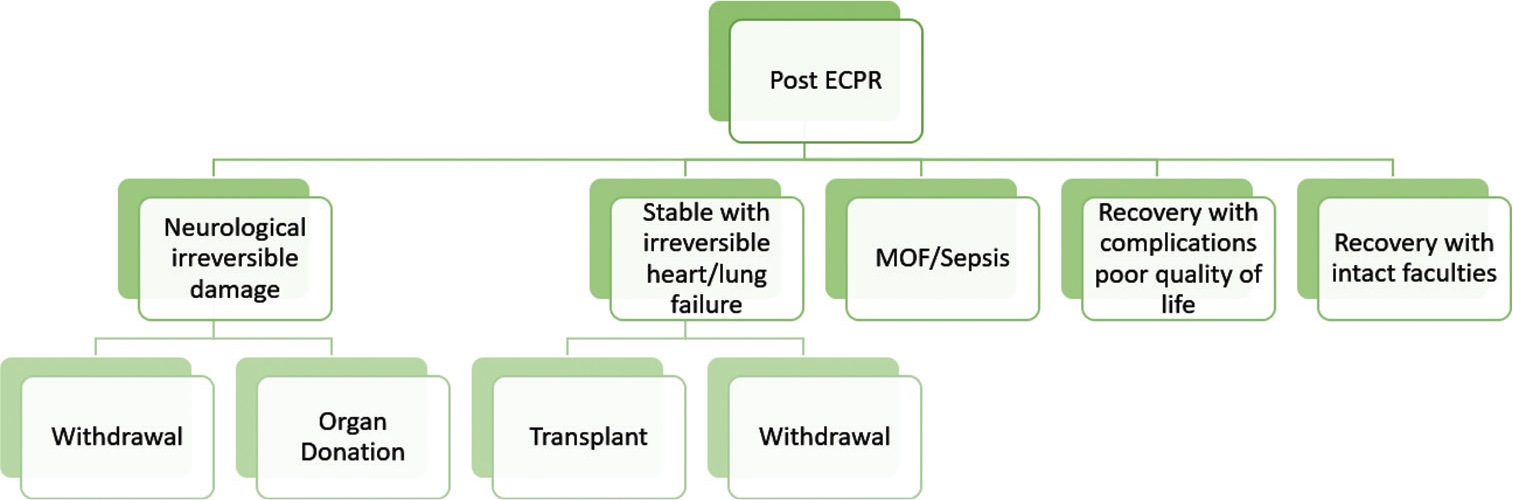
- ECPR and organ donation. ECPR: Extracorporeal cardiopulmonary resuscitation.
Organ donation in CA patients treated with extracorporeal CPR is feasible. CA is a catastrophic event with a high mortality rate. In more severe cases, while the circulation could be supported by extracorporeal CPR (eCPR: ECPR), a devastating anoxic brain injury could develop. This condition might evolve to brain death (BD) and, potentially, to organ donation in refractory CA patients treated with eCPR, the prevalence of BD is high. This population has a high potential for considering organ donation. Donated organs have a good outcome.
INDIAN ASPECT OF ECPR
ECPRs are mostly done in tertiary care center in India. There is little scope for out of hospital arrest as poor quality of CPR and response time exists with lack of awareness about ECPR, which hinders its wider usage even in IHCA. Emergency department doctors need to be involved to counsel, recognize candidates activate, and initiate ECPR. Cost constraints infrastructure and trained workforce. Legal and ethical issues around organ donation following ECPR need more clarification. Testing Brainstem death on ECMO – no clear guidelines in India of ECPR exists so far.
FUTURE OF ECPR
Many ECPR trails are on the horizon for ECPR globally some example are:- ECPB4OHCA (Emergency Cardiopulmonary Bypass for CA) TRIAL (NCT01605409 ClinicalTrials.gov) in Austria to identify the incidence of ROSC in 48 h following CCPR versus ECPR study population of 40 patients. INCEPTION (Early Initiation of Extracorporeal Life Support in Refractory OHCA) Trial (NCT03101787 ClinicalTrials. gov) in Netherlands.[7-9] 30-day survival rate with improved neurological recovery in OHCA between CCPR and ECPR. A total of 110 patients were planned and the cerebral performance category scale of 1–3 indicates good outcome 30-day survival rate with improved neurological recovery in OHCA between CCPR and ECPR. The EROCA study (NCT03065647 ClinicalTrials.gov) in the USA.[10-12] Efficiency of emergency transport to the possible ECPR center. The sample size of the study is 30 patients and is ongoing.[13]
CONCLUSION
ECMO providers in India are often called on for instituting ECMO with impending failure window. There is a requirement for SOPs conducive to the available resources for rapid institution of ECMO. It is essential to educate and in still concept of ECPR in future CPR guidelines. Training workforce from relevant specialties to have a round the clock multidisciplinary team is need of the hour. Future brain death testing guidelines should take cognizance of patients on ECMO as potential brain dead donors. Training ECMO specialists to deal with financial Legal Ethical issues that arise while counseling in high-pressure clinical scenarios convincingly. Further studies are needed from India to clarify pre-procedural, intra-procedural, and post-procedural management of ECPR and its outcomes. Low-flow time means duration of mechanical cardiopulmonary resuscitation before full extracorporeal membrane oxygenation support. There was a significant, negative, linear correlation between time to circulatory support, and survival in the overall eCPR population (P < 0.001, r = 0.266).[14,15]
Declaration of patient consent
Patient’s consent not required as their identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Extracorporeal cardiopulmonary resuscitation in adults. Interim guideline consensus statement from the extracorporeal life support organization. ASAIO J. 2021;67:221-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American heart association, European resuscitation council, Australian resuscitation council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican heart foundation, resuscitation councils of Southern Africa) Circulation. 2004;110:3385-97.
- [CrossRef] [PubMed] [Google Scholar]
- 2019 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: Summary from the basic life support; Advanced life support; Paediatric life support; neonatal life support; Education, implementation, and teams; and first aid task forces. Circulation. 2019;140:e826-80.
- [Google Scholar]
- Coronary Artery disease in patients with out-of-hospital refractory ventricular fibrillation cardiac arrest. J Am Coll Cardiol. 2017;70:1109-17.
- [CrossRef] [PubMed] [Google Scholar]
- Duration of resuscitation efforts and functional outcome after out-of-hospital cardiac arrest: When should we change to novel therapies? Circulation. 2013;128:2488-94.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between the duration of cardiopulmonary resuscitation and favorable neurological outcomes after out-of-hospital cardiac arrest: A prospective, nationwide, population-based cohort study. J Am Heart Assoc. 2016;5:e002819.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal membrane oxygenation in cardiopulmonary disease in adults. J Am Coll Cardiol. 2014;63:2769-78.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal cardiopulmonary resuscitation for cardiac arrest: A systematic review. Resuscitation. 2018;131:91-100.
- [CrossRef] [PubMed] [Google Scholar]
- ECMO Cardio-pulmonary resuscitation (ECPR), trends in survival from an international multicentre cohort study over 12-years. Resuscitation. 2017;112:34-40.
- [CrossRef] [PubMed] [Google Scholar]
- Managing cardiac arrest with refractory ventricular fibrillation in the emergency department: Conventional cardiopulmonary resuscitation versus extracorporeal cardiopulmonary resuscitation. Resuscitation. 2015;92:70-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hospitals' extracorporeal cardiopulmonary resuscitation capabilities and outcomes in out-of-hospital cardiac arrest: A population-based study. Resuscitation. 2019;136:85-92.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal cardiopulmonary resuscitation: outcomes and complications at a quaternary referral center. J Cardiothorac Vasc Anesth. 2020;34:1191-4.
- [CrossRef] [PubMed] [Google Scholar]
- ECPR for out-of-hospital cardiac arrest: More evidence is needed. Crit Care. 2020;24:7.
- [CrossRef] [PubMed] [Google Scholar]
- Organ donation in cardiac arrest patients treated with extracorporeal CPR: A single centre observational study. Resuscitation. 2017;118:133-9.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR) Crit Care. 2017;21:157.
- [CrossRef] [PubMed] [Google Scholar]






