Translate this page into:
Platelet Reactivity on ECMO: Role of VerifyNow
*Corresponding author: Omer Mohammed Mujahid, Department of Cardiac Anaesthesia and Critical Care, All India Institute of Medical Sciences, Delhi, India. omermohd1992@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mujahid OM, Kapoor PM, Prakash M, Sharma P, Badge M, Choudhury M, et al. Platelet Reactivity on ECMO: Role of VerifyNow. J Card Crit Care TSS 2023;7:129-32.
Abstract
Viscoelastic assays help in identifying disorders of clotting factors, platelet function, and detection of excessive fibrinolysis. Rotational thromboelastometry (ROTEM) assesses quantitative and qualitative aspects of whole blood coagulation which allows for the determination of the mechanism of hemostatic disturbance. This helps clinicians in targeting the correct blood component therapy transfusion. Now, using verify we aim to study platelet reactivity, VA ECMO which will reflect the platelet aggregation response to an aggregating agent like Aspirin and thus know the etiology of bleeding on VA ECMO, to know the right component therapy to be transfused with a Point of Care test. For extracorporeal membrane oxygenation, although the conventional laboratory tests are used to monitor anticoagulation on whole blood, viscoelastic tests reflect coagulation status like no other standard laboratory tests. They show the status of color propagation, formation, and stabilization. It was reported that platelet function was impaired over time in all parameters with different activators.
Keywords
Platelet Aggregation
Platelet Reactivity
ECMO
VerifyNow
INTRODUCTION
During extracorporeal membrane oxygenation (ECMO) the normal physiological hemostasis is disturbed. The contact of circulating blood to non-endothelial foreign surface shifts the hemostatic balance to a hypercoagulable state which can predispose patients to risks of thrombotic events. To overcome this and to restore, the hemostatic mechanisms of antithrombotic therapy are instituted with unfractionated heparin (UFH) to achieve therapeutic anticoagulation levels. The use of UFH can result in hemorrhagic sequelae which is a cause of significant morbidity and mortality. A fine balance has to be achieved to counter the risks of thrombosis and bleeding.[1] Patients going on ECMO may have inherent cardiac dysfunction along with poor end-organ perfusion, the end result being a possible liver dysfunction hence decreased coagulation factor production. Standard methods of monitoring anticoagulation on ECMO include measurement of activated clotting time (ACT), activated partial thromboplastin time, anti-factor Xa assay, anti-thrombin levels, all with a longer turnaround time of more than 2 h, and point-of-care tests such as thromboelastography and thromboelastometry with a shorter turnaround time of 15–20 min.[2]
Viscoelastic assays help in identifying disorders of clotting factors, platelet function, and detection of excessive fibrinolysis. Rotational Thromboelastometry (ROTEM) assesses quantitative and qualitative aspects of whole blood coagulation which allows for determination of the mechanism of hemostatic disturbance and helps clinicians in targeted transfusion therapy.[3]
Platelet reactivity is a term that indicates the degree of response of platelets to a stimulus which is usually an aggregating agent. The various methods to measure platelet reactivity include light transmission aggregometry, multiplate electrode aggregometry, and VerifyNow™. Among the novel techniques, VerifyNow™ has been used specifically for point-of-care measurement of platelet aggregation by antiplatelet medications such as aspirin, P2Y12 antagonists such as clopidogrel, and GPIIb/IIIa antagonists.[4]
VISCOELASTIC TESTING ON ECMO: USING ROTATIONAL THROMBOELASTOMETRY
Although conventional laboratory tests are used to monitor anticoagulation on ECMO, whole blood viscoelastic tests reflect coagulation status like no other standard laboratory tests. They show the status of clot formation, propagation and stabilization. Fibrinolysis is also demonstrated, unlike any other laboratory test. Fibrinogen levels can be measured in standard tests, point of care viscoelastic assays demonstrate the contribution of fibrinogen in clot formation, thus providing a qualitative fibrinogen contribution to clot formation. Elevated d-dimer levels may be seen in this set of patients as part of the acute phase reaction when on ECMO.
FIBTEM ON ROTEM IMPARTS WITHIN MINUTES, DETAILS OF THE FIBRINOLYTIC PATHWAY IN ECMO PATIENTS
Fibrinogen has an important role in the prevention and management of bleeding in cardiac surgery and ECMO. Levels of fibrinogen remain low on ECMO. FIBTEM assay (FIBTEM A5 and A10) plays an important role in hemostasis monitoring. ROTEM® serves as a rapid coagulation monitoring system with the additional value of early massive transfusion (MT) risk stratification using the FIBTEM A10 (ROC-AUC for MT: 0.83).[6] Taken together, the three ROTEM® tests included in the school study (INTEM, EXTEM, and FIBTEM) enable rapid detection of most coagulation disorders.[7,8] These potentially include hyperfibrinolysis, which cannot be assessed adequately by standard coagulation tests, although it must be acknowledged that no specific definition of hyperfibrinolysis based on ROTEM® parameters exists yet in guidelines validated.[9] INTEM, EXTEM, and FIBTEM are easily performed in our ER, and the ROTEM® device allows them to be performed simultaneously. The results may be used to facilitate prompt, goal-directed coagulation therapy according to the patient’s individual needs.[10,11]
AIIMS EXPERIENCE WITH PLATELET FUNCTION TESTING
Platelet function testing using ROTEM platelet aggregometry has been used in our institute to predict post-operative bleeding in patients undergoing coronary artery bypass grafting (CABG). In a major study on platelet function testing in CABG patients. The authors found that platelet function was impaired over time in all ROTEM parameters with different activators. They concluded that platelet function testing using ROTEM platelet analysis can help exclude platelet dysfunction as a cause of bleeding in post-cardiac surgery patients.[5]
PLATELET REACTIVITY ON ECMO; AIIMS EXPERIENCE
There is a decrease in adenosine diphosphate (ADP)-mediated platelet aggregation due to a possible decrease in ADP levels in the circulating platelets. A supranormal fibrinogen response through GPIIb-IIIa mediated platelet aggregation is seen to overcome the ADP and arachidonic acid-mediated depletion in platelet aggregation.[12] Nair et al. in their study have reported that platelet malfunction on ECMO could have been overcome by a supranormal fibrinogen response. This could be attributed to the role of fibrinogen in GPIIb-IIIa-mediated platelet aggregation. To quote the authors “From a clinical perspective this might imply the utility of fibrinogen concentrates therapy to overcome the frequently observed Platelet dysfunction.”[13]
CHALLENGES IN MEASUREMENT OF PLATELET REACTIVITY
Measurement of platelet reactivity, today for the cardiac patient on ECMO is a challenge. Reasons for the latter include imbibing a new technology, and learning newer signature graphs with interpretations; there exists a complex cascade of coagulation from the initiation, and amplification to the propagation phase of platelet aggregation. Although both ROTEM and VerifyNow, help in understanding this complex cascade of coagulation, simplistically, there is an enigma that remains. Hesitancy and resistance in adopting a newer technique which is costly needs education and encouragement for its daily administration. The simplicity of the use of platelet reactivity on ECMO patients with a sleek machine, which is easy to transport from OT to intensive care unit/cath lab makes deciphering platelet function on ECMO easily doable, overcoming, thus the above challenge, in simple steps as outlined in [Figure 1a and b].
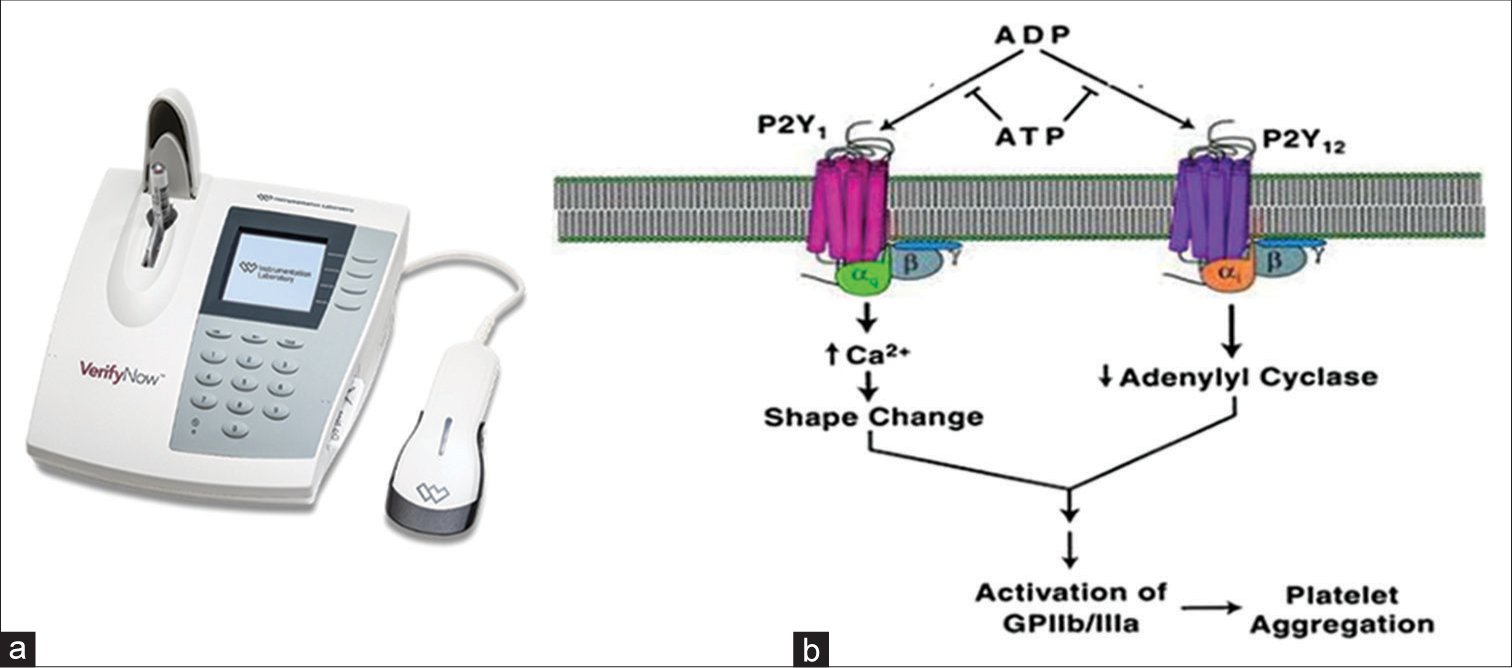
- (a) The VerifyNow machine for high platelet reactivity and low platelet reactivity values. It shows a PRU results with cartridge use of the reagent to intubate the effect of antiplatelet drugs such as prasugrel or aspirin. (b) The VerifyNow device is fully automated and near platelet testing aggregation system, and is available solely for the monitoring of the three major classes of antiplatelet drugs (e.g., GPIIb/IIIa inhibitors, aspirin, and P2Y12 receptor inhibitors/antagonists).
MONITORING ANTIPLATELET THERAPY VerifyNow
Modern antiplatelet therapy monitoring on viscoelastic POC ROTEM and VerifyNow tests is based on the inhibition of three major platelet activation pathways chiefly, cyclooxygenase-1 inhibition resulting in a reduction of thromboxane A2, P2Y12 (ADP) inhibition and GPIIb/IIIa receptor blockade. Recently the American Heart Association/the American College of Cardiology Foundation updated the consensus document and proposed updated cut-off values for high platelet reactivity (HPR) and low platelet reactivity (LPR) to ADP that might be used in future investigations of personalized anti platelet therapy. LPR to ADP is higher risk of bleeding and HPR to ADP is higher risk of thrombosis, they concluded.[14]
THE VerifyNow PRASUGREL (PRU) TEST
The verify Now, calculates the Prasugrel (or PRU Test) a PRU result is calculated based upon the rate and extent of platelet aggregation recorded in the channel containing the platelet agonist, ADP. P2Y receptor-mediated platelet aggregation and PRU test results from VerifyNow are not influenced by non-specific platelet aggregation mediated through P2Y receptors.[15] Hence, the result on VerifyNow remains specific and sensitive. On ECMO, platelet function and count are both severely impaired. Acquired factor XIII deficiency is common during ECMO therapy and associated with major bleeding events and transfusion requirements.[16]
At present, there is no ideal anticoagulant agent to make the ECMO circuit as non-thrombogenic as the native vascular endothelium. Some centers utilize a multi-system therapy protocol using dipyridamole, aspirin, aprotinin, and pentoxifylline. This protocol showed a reduction in bleeding complications and survival benefits compared to the control patients treated with heparin and ACT monitoring alone for anticoagulation.[17]
During ECMO, blood exposure to the artificial biomaterial causes platelet activation and aggregation, leading to increased thrombotic risk. Aspirin is the commonly used antiplatelet agent, which acts through non-competitive inhibition of platelet cyclooxygenase-1 and thromboxane A2 production. The addition of aspirin may reduce the clot burden in both the patient and the ECMO circuit. However, there is no data available on children supported by ECMO with aspirin use. Defective platelet aggregation on ECMO in response to all agonists is seen in patients with GPIIb-IIIa receptors or when there is severe hyperfibrinogenemia. This defect in platelet aggregation can be remedied by the addition of cryoprecipitate (source of fibrinogen) in case of hypo-fibrinogenemia developing on ECMO. The reasons for thrombocytopenia during ECMO, stems from platelet adherence to the oxygenator membrane. Platelet transfusions on ECMO are routine today. These carry risks of bacterial fungal infections and the development or worsening of pulmonary hypertension. The need for ideal management today is for fewer platelet transfusions so that the intensivist can overcome the adverse effects of transfusion and improve outcomes on ECMO. Hence, there is a need to study platelet reactivity on ECMO.[18]
CONCLUSION
Platelet reactivity on ECMO can easily be detected. The evidence for using aspirin is limited to a few adult patients receiving ECMO.[19] Furthermore, these anticoagulant antiplatelet therapies are not standardized in pediatric ECMO patients. Further studies are needed to improve anticoagulation management in children during ECMO therapy. More studies in the future are warranted to detect bleeding and thrombosis management in ECMO due to platelet aggregation problems in future. The significant variation in clinical practice and lack of standardized anticoagulation management warrants further studies in the future. It is important in the future to determine the pharmacokinetics and pharmacodynamics, as well as the safety and efficacy of these therapies on ECMO. Monitoring platelet reactivity on ECMO as a guide to these therapies is now on the horizon, with VerifyNow.[20]
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
Poonam Malhotra Kapoor and Minati Choudhury are the members of the Editorial Board.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Financial support and sponsorship
Nil.
References
- Extracorporeal Life Support: The ELSO Red Book (5th ed). Ann Arbor, Michigan: Extracorporeal Life Support Organization; 2017. p. :831.
- [Google Scholar]
- Comparison of Thromboelastometry (ROTEM®) with Standard Plasmatic Coagulation Testing in Paediatric Surgery. Br J Anaesth. 2012;108:36-41.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and Pathophysiologic Aspects of ECMO-Associated Hemorrhagic Complications. PLoS One. 2020;15:e0240117.
- [CrossRef] [PubMed] [Google Scholar]
- Novel Strategies for Assessing Platelet Reactivity. Future Cardiol. 2017;13:33-47.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet Function Test in Coronary Artery Bypass Grafting: Does it Predict Postoperative Bleeding? J Card Crit Care TSS. 2021;5:186-95.
- [CrossRef] [Google Scholar]
- Patient Blood Management in India-Review of Current Practices and Feasibility of Applying Appropriate Standard of Care Guidelines. A Position Paper by an Interdisciplinary Expert Group. J Anaesthesiol Clin Pharmacol. 2021;37:3-13.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperfibrinolysis after Major Trauma: Differential Diagnosis of Lysis Patterns and Prognostic Value of Thrombelastometry. J Trauma. 2009;67:125-31.
- [CrossRef] [PubMed] [Google Scholar]
- Primary Fibrinolysis is Integral in the Pathogenesis of the Acute Coagulopathy of Trauma. Ann Surg. 2010;252:434-42.
- [CrossRef] [PubMed] [Google Scholar]
- Is there a Role for Preoperative Platelet Function Testing in Patients Undergoing Cardiac Surgery during Antiplatelet Therapy? Circulation. 2018;138:2145-59.
- [CrossRef] [PubMed] [Google Scholar]
- Goal-Directed Coagulation Management of Major Trauma Patients using Thromboelastometry (ROTEM)-Guided Administration of Fibrinogen Concentrate and Prothrombin Complex Concentrate. Crit Care. 2010;14:R55.
- [CrossRef] [PubMed] [Google Scholar]
- Transfusion in Trauma: Thromboelastometry-Guided Coagulation Factor Concentrate-Based Therapy Versus Standard Fresh Frozen Plasma-Based Therapy. Crit Care. 2011;15:R83.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of Coagulopathy on Veno-Arterial ECMO (VA) Extracorporeal Membrane Oxygenation using Platelet Aggregometry and Standard Tests: A Narrative Review. Egypt J Crit Care Med. 2018;6:73-8.
- [CrossRef] [Google Scholar]
- Prospective Observational Study of Hemostatic Alterations during Adult Extracorporeal Membrane Oxygenation (ECMO) using Point-of-care Thromboelastometry and Platelet Aggregometry. J Cardiothorac Vasc Anesth. 2015;29:288-96.
- [CrossRef] [PubMed] [Google Scholar]
- 2016 ACC/AHA Guideline Focused update on Duration of Dual Antiplatelet Therapy in Patients with Coronary Artery Disease: A Report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines: An update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/ AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients with Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of st-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation. 2016;134:e123-55.
- [CrossRef] [Google Scholar]
- Use of the VerifyNow Point of care Assay to Assess the Pharmacodynamic Effects of Loading and Maintenance Dose Regimens of Prasugrel and Ticagrelor. J Thromb Thrombolysis. 2021;51:741-7.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired Factor XIII Deficiency is Common during ECMO Therapy and Associated with Major Bleeding Events and Transfusion Requirements. J Clin Med. 2023;12:4115.
- [CrossRef] [PubMed] [Google Scholar]
- Reduction of Haemorrhagic Complications during Mechanically Assisted Circulation with the use of a Multi-System Anticoagulation Protocol. Int J Artif Organs. 1995;18:649-55.
- [CrossRef] [PubMed] [Google Scholar]
- Simulation in Thromboelastography: Platelet Mapping Assay (Part-I) Ann Card Anaesth. 2016;19:530-2.
- [CrossRef] [PubMed] [Google Scholar]
- Dual Antiplatelet Therapy (Dapt) Versus no Antiplatelet Therapy and Incidence of Major Bleeding in Patients on Venoarterial Extracorporeal Membrane Oxygenation. PLoS One. 2016;11:e0159973.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Anticoagulation during Extracorporeal Membrane Oxygenation in Children. Pediatr Rep. 2022;14:320-32.
- [CrossRef] [PubMed] [Google Scholar]






