Translate this page into:
Implementation of Patient Blood Management – A Long and Winding Road but Worth Doing!
*Corresponding author: Klaus Görlinger, Department of Anaesthesiology and Intensive Care Medicine, University Hospital Essen, Essen, Germany. kgoerlinger@werfen.com
-
Received: ,
Accepted: ,
How to cite this article: Görlinger K. Implementation of Patient Blood Management – A Long and Winding Road but Worth Doing! J Card Crit Care TSS. 2024;8:1-4. doi: 10.25259/JCCC_24S1_KGIE
“Patient blood management (PBM) is a patient-centered, systematic, and evidence-based approach to improve patient outcomes by managing and preserving a patient’s own blood while promoting patient safety and empowerment.” The definition emphasizes the critical role of informed choice. PBM involves the timely, multidisciplinary application of evidence-based medical and surgical concepts aimed at (1) screening for, diagnosing, and appropriately treating anemia; (2) minimizing surgical, procedural, and iatrogenic blood losses and managing coagulopathic bleeding throughout the care; and (3) supporting the patient while appropriate treatment is initiated.[1] PBM is most effectively implemented as bundles of care.[2,3] Accordingly, the ABC toolbox of PBM contains bundles of care for (1) Anemia and Iron Deficiency, (2) Blood Loss and Bleeding, and (3) Coagulopathy.[4]
Here, coagulopathy is defined as a clinical condition in which the blood’s ability to clot is impaired or increased and is associated with prolonged or excessive bleeding or thrombosis. Pathologic coagulation tests alone are not sufficient to define coagulopathy since a rebalance of hemostasis can occur in several clinical conditions, for example, in chronic liver disease. Therefore, pathologic coagulation tests should NOT be corrected routinely in the absence of bleeding. However, this is still common practice in patients with pathologic laboratory results before invasive interventions or treated at the intensive care unit – even if large observational studies and randomized controlled trials showed no benefit but increased morbidity and mortality.[5-9] Here, implementation of PBM concepts has been shown to reduce prophylactic plasma and platelet transfusion and transfusion-related adverse events.[10-13]
Accordingly, PBM equals patient safety, which is defined by the World Health Organization (WHO) as “the absence of preventable harm to a patient during the process of health care and reduction of risk of unnecessary harm associated with health care to an acceptable minimum.[14,15] An acceptable minimum refers to the collective notions of given current knowledge, resources available, and the context in which care was delivered weighed against the risk of non-treatment or other treatment.” Inappropriate blood transfusion is definitively a safety issue that must be addressed by education and adherence to guidelines.[16,17] In some countries, such as Italy, PBM implementation is considered mandatory in light of new Italian laws on patient safety.[18] The Italian Law No. 24/2017 focuses on the safety of care by encouraging the necessary implementation of PBM in hospital settings. The failure to adopt an organized PBM program may constitute, in the event of an adverse transfusion event, a clear profile of health responsibility on the part of the management and clinicians.[19] Accordingly, PBM is considered “Good Medical Practice” following the concept of “Precision Medicine” with diagnosis first, followed by appropriate therapy and reassessment.[20,21]
On November 21, 2018, an Indian interdisciplinary expert group working in governmental and private healthcare institutions met for the first time to review and discuss the status quo and current practice of PBM in India and the feasibility of applying appropriate standard-of-care guidelines for a broader implementation of PBM in India. The proceedings of this meeting were published in the Journal of Anesthesiology and Clinical Pharmacology in April 2021.[22] On the one hand, misconceptions, lack of education, and change culture have been identified as important barriers to PBM implementation.[23-27] On the other hand, awareness, knowledge, evidence, ethics, economics, education (4 Es), communication, collaboration, consensus, continuum of care (4 Cs), motivation, implementation, improvement (data from audits demonstrating improvement in patient outcomes and health economics), and sustainability (long-term adherence to PBM guidelines) have been identified as drivers for cultural change from transfusion medicine to PBM.[28-34] Since PBM is a multidisciplinary and multi-professional team approach, the hospital transfusion or PBM committee plays an essential role in PBM implementation, and the anesthesiologist may take the lead here.[35-37] This brings us to the 6 Ws of PBM implementation: Who is responsible (Champion), Who must be involved (e.g., Transfusion Committee, PBM Committee, Anesthesiology, Intensivists, Surgeons, Internal Medicine, Obstetrics, Hematology/Lab, Transfusion Medicine, Nursing, Administration (Controlling/ Finance)), Who must be trained (e.g., in point of care [POC] viscoelastic testing and interpretation), Where should viscoelastic testing devices be places (e.g., POC/Bedside, POC Lab, Central Lab, and Blood Bank), and Which protocols and algorithms should be agreed on and used and how adherence and improvement (e.g., transfusion requirements, complication rates, and health economics) should be monitored.[38,39]
Considering all these drivers and barriers for PBM implementation results in the following call-to-action to physicians and nurses who want to implement PBM in their institutions:
Identify wrong beliefs and knowledge gaps
Identify and abandon potential harmful or low-value care (to use these resources to start your PBM program)[40]
Identify potential PBM stakeholders and keep everybody on board (team approach)
Identify the main PBM issues in your hospital and focus on these in the beginning (hospital-centered approach)
Identify the diagnostic/therapeutic options available in your hospital/country (resources)
Convince your surgeon (outcome) and administration (cost-effectiveness) with data (publications and internal audits)[29-34]
In the end, implement PBM as a holistic concept (effectiveness).
On October 19, 2021, the WHO published a policy brief on the urgent need to implement PBM.[23] Since then, 127 PubMed-listed papers have been published with the term “Patient Blood Management” in the title.[52] However, we are still far away from worldwide PBM implementation.[53-55]
To address the importance of education and knowledge, an online certified PBM course for India, the Middle East, and South Asia was established in 2020. This PBM course has an international faculty of PBM experts and consists of six sessions/modules. To receive the certificate, participants had to attend the sessions and pass the corresponding examination with multiple-choice questions. In between, this certified PBM course is endorsed and supported by multiple medical societies such as the Simulation Society (TSS), the Cardiac Society of Nepal, the College of Anesthesiologists and Intensivists of Sri Lanka, the Sri Lanka College of Transfusion Physicians, the Malaysian Society of PBM, and the Australian and New Zealand College of Anesthesiologists and is supported by Werfen. From 2020 to 2023, the number of registrations and certifications increased 10-fold and 4-fold, respectively [Figure 1].
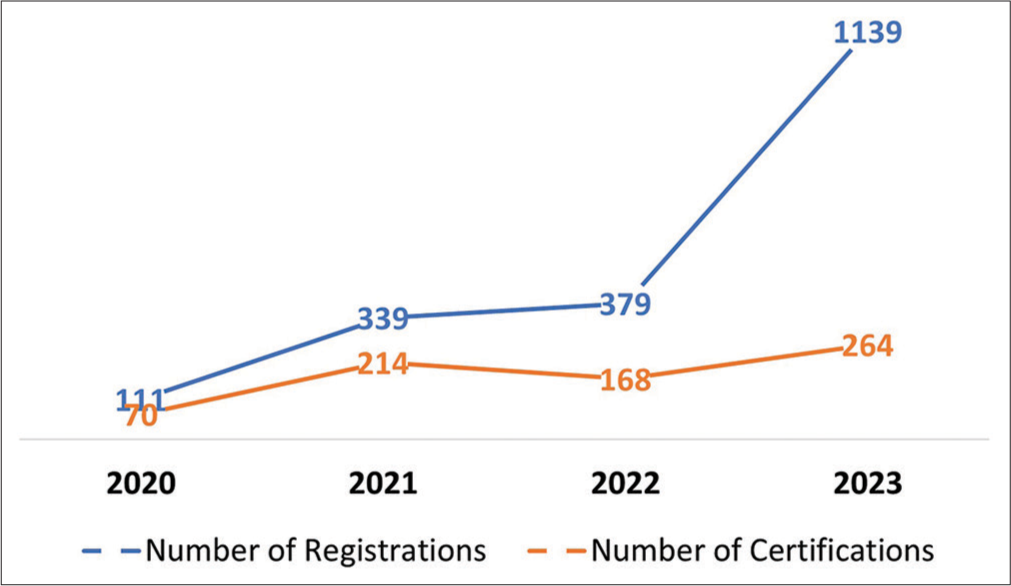
- Number of registrations and certifications for the online Certified Patient Blood Management Course for India, the Middle East, and South Asia from 2020 to 2023.
This issue of the Journal of Cardiac Critical Care TSS, as the official journal of TSS, publishes several review papers summarizing key presentations of the last certified PBM course from 2023.[56,57] This successful educational activity will be continued in 2024 since there is still a long and winding road to go to implement PBM in India, South Asia, and beyond.
“Most of us can read the writing on the wall; we just assume it’s addressed to someone else.”
“Knowledge is Power, but Enthusiasm pulls the Switch.”
Ivern Ball, American Writer and Aphorist, *July 31, 1926, †January 12, 1992.
References
- A Global Definition of Patient Blood Management. Anesth Analg. 2022;135:476-88.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management Bundles to Facilitate Implementation. Transfus Med Rev. 2017;31:62-71.
- [CrossRef] [PubMed] [Google Scholar]
- Controversies in the Clinical Practice of Patient Blood Management. J Cardiothorac Vasc Anesth. 2021;35:1933-41.
- [CrossRef] [PubMed] [Google Scholar]
- Essential Role of Patient Blood Management in a Pandemic: A Call for Action. Anesth Analg. 2020;131:74-85.
- [CrossRef] [PubMed] [Google Scholar]
- Prophylactic Plasma Transfusion Is Not Associated with Decreased Red Blood Cell Requirements in Critically Ill Patients. Anesth Analg. 2017;124:1636-43.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence, Risk Factors, and Outcome of Transfusion-Related Acute Lung Injury in Critically Ill Children: A Retrospective Study. J Crit Care. 2015;30:55-9.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet Transfusion Versus Standard Care after Acute Stroke Due to Spontaneous Cerebral Haemorrhage Associated with Antiplatelet Therapy (PATCH): A Randomised, Open-label, Phase 3 Trial. Lancet. 2016;387:2605-13.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet Transfusions in Pediatric Intensive Care. Pediatr Crit Care Med. 2016;17:e420-9.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized Trial of Platelet-Transfusion Thresholds in Neonates. N Engl J Med. 2019;380:242-51.
- [CrossRef] [PubMed] [Google Scholar]
- Implementation of a Comprehensive Patient Blood Management Program for Hospitalized Patients at a Large United States Medical Center. Mayo Clin Proc. 2021;96:2980-90.
- [CrossRef] [PubMed] [Google Scholar]
- Viscoelastometric Versus Standard Coagulation Tests to Guide Periprocedural Transfusion in Adults with Cirrhosis: A Meta-analysis of Randomized Controlled Trials. Vox Sang. 2022;117:553-61.
- [CrossRef] [PubMed] [Google Scholar]
- Thromboelastography-Guided Therapy Enhances Patient Blood Management in Cirrhotic Patients: A Meta-analysis Based on Randomized Controlled Trials. Semin Thromb Hemost. 2023;49:162-72.
- [CrossRef] [PubMed] [Google Scholar]
- Rotational Thromboelastometry-Guided Blood Component Use in Cirrhotic Children Undergoing Invasive Procedures: Randomized Controlled Trial. Liver Int. 2022;42:2492-500.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management Equals Patient Safety. Best Pract Res Clin Anaesthesiol. 2016;30:159-69.
- [CrossRef] [PubMed] [Google Scholar]
- German Patient Blood Management Network: Effectiveness and Safety Analysis in 1.2 Million Patients. Br J Anaesth. 2023;131:472-81.
- [CrossRef] [PubMed] [Google Scholar]
- Prophylactic Plasma and Platelet Transfusion in the Critically Ill Patient: Just Useless and Expensive or Even Harmful? BMC Anesthesiol. 2015;15:86.
- [CrossRef] [PubMed] [Google Scholar]
- Adherence to Guidelines Improves Outcomes in Coronary Artery Surgery. Eur J Cardiothorac Surg. 2022;62:ezac197.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management Implementation in Light of New Italian Laws on Patient's Safety. Transfus Apher Sci. 2020;59:102811.
- [CrossRef] [PubMed] [Google Scholar]
- Medico-Legal and Management Issues in Patient Blood Management Era. Recenti Prog Med. 2023;114:730-4.
- [Google Scholar]
- Coagulopathy and Haemorrhagic Progression in Traumatic Brain Injury: Advances in Mechanisms, Diagnosis, and Management. Lancet Neurol. 2017;16:630-47.
- [CrossRef] [PubMed] [Google Scholar]
- Coagulopathy and Progression of Intracranial Hemorrhage in Traumatic Brain Injury: Mechanisms, Impact, and Therapeutic Considerations. Neurosurgery. 2021;89:954-66.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management in India-Review of Current Practices and Feasibility of Applying Appropriate Standard of Care Guidelines. A Position Paper by an Interdisciplinary Expert Group. J Anaesthesiol Clin Pharmacol. 2021;37:3-13.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Influencing Plasma Transfusion Practices in Paediatric Intensive Care Units Around the World. Vox Sang. 2017;112:140-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fresh Frozen Plasma Transfusion in Acute Variceal Haemorrhage: Results from a Multicentre Cohort Study. Liver Int. 2021;41:1901-8.
- [CrossRef] [PubMed] [Google Scholar]
- Overcoming Barriers to Evidence-based Patient Blood Management: A Restricted Review. Implement Sci. 2020;15:6.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers and Facilitators to Implementing Evidence Based Bleeding Management in Australian Cardiac Surgery Units: A Qualitative Interview Study Analysed with the Theoretical Domains Framework and COM-B Model. BMC Health Serv Res. 2021;21:550.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges in Patient Blood Management for Cardiac Surgery: A Narrative Review. J Clin Med. 2021;10:2454.
- [CrossRef] [PubMed] [Google Scholar]
- Improving Awareness about Patient Blood Management in Portugal: A Call for Action Arising from a Delphi Panel. Acta Med Port. 2022;35:749-57.
- [CrossRef] [PubMed] [Google Scholar]
- Protocol Guided Bleeding Management Improves Cardiac Surgery Patient Outcomes. Vox Sang. 2015;109:267-79.
- [CrossRef] [PubMed] [Google Scholar]
- Perioperative Patient Blood Management to Improve Outcomes. Anesth Analg. 2018;127:1211-20.
- [CrossRef] [PubMed] [Google Scholar]
- Multimodal Patient Blood Management Program Based on a Three-Pillar Strategy: A Systematic Review and Meta-analysis. Ann Surg. 2019;269:794-804.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management: Improving Outcomes for Millions While Saving Billions. What Is Holding It Up? Anesth Analg. 2022;135:511-23.
- [CrossRef] [PubMed] [Google Scholar]
- Data and Metrics for Patient Blood Management: A Narrative Review and Practical Guide. Anesth Analg 2023 Epub ahead of print. doi: 10.1213/ANE.0000000000006557
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management as an Emerging Concept in Quality: The Role of Nurses. J Nurs Care Qual 2023 Epub ahead of print. doi: 10.1097/NCQ.0000000000000734
- [CrossRef] [PubMed] [Google Scholar]
- Transfusion Safety Officers in the United States: Survey of Characteristics and Approaches to Implementation. Transfus Apher Sci. 2021;60:103199.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management: A Call to Anesthesiologists for Leadership. Minerva Anestesiol. 2019;85:577-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of Evidence-based Algorithms for Rotational Thromboelastometry-Guided Bleeding Management. Korean J Anesthesiol. 2019;72:297-322.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Thromboelastometry-Guided Patient Blood Management on Blood Product Acquisition, Potentially Preventable Complications, and Hospital Cost-savings In: 23rd Annual Symposium on Patient Blood Management, Haemostasis and Thrombosis. 2023.
- [Google Scholar]
- Towards a Systematic Approach for (De) Implementation of Patient Blood Management Strategies. Transfus Med. 2018;28:158-67.
- [CrossRef] [PubMed] [Google Scholar]
- A Prospective Randomized Clinical Trial of Efficacy of Algorithm-Based Point of Care Guided Hemostatic Therapy in Cyanotic Congenital Heart Disease Surgical Patients. J Card Crit Care TSS. 2020;3:8-16.
- [CrossRef] [Google Scholar]
- Utility of Platelet Function Testing in Cardiac Surgery. J Card Crit Care TSS. 2021;5:84-7.
- [CrossRef] [Google Scholar]
- Patient Blood Management in Liver Transplant-A Concise Review. Biomedicines. 2023;11:1093.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Severe Peri-Operative Bleeding: Guidelines from the European Society of Anaesthesiology and Intensive Care: Second Update 2022. Eur J Anaesthesiol. 2023;40:226-304.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management in Obstetrics: Prevention and Treatment of Postpartum Haemorrhage. A NATA Consensus Statement. Blood Transfus. 2019;17:112-36.
- [Google Scholar]
- Patient Blood Management for Neonates and Children Undergoing Cardiac Surgery: 2019 NATA Guidelines. J Cardiothorac Vasc Anesth. 2019;33:3249-63.
- [CrossRef] [PubMed] [Google Scholar]
- 2017 EACTS/EACTA Guidelines on Patient Blood Management for Adult Cardiac Surgery. J Cardiothorac Vasc Anesth. 2018;32:88-120.
- [Google Scholar]
- Society of Cardiovascular Anesthesiologists Clinical Practice Improvement Advisory for Management of Perioperative Bleeding and Hemostasis in Cardiac Surgery Patients. Anesth Analg. 2019;129:1209-21.
- [CrossRef] [PubMed] [Google Scholar]
- STS/SCA/AmSECT/SABM Update to the Clinical Practice Guidelines on Patient Blood Management. J Cardiothorac Vasc Anesth. 2021;35:2569-91.
- [CrossRef] [PubMed] [Google Scholar]
- Blood Conservation and Hemostasis in Cardiac Surgery: A Survey of Practice Variation and Adoption of Evidence-Based Guidelines. Anesth Analg. 2021;133:104-14.
- [CrossRef] [PubMed] [Google Scholar]
- Extract from the 2022 ESC Guidelines on Cardiovascular Assessment and Management of Patients Undergoing Non-cardiac Surgery-Patient Blood Management. Blood Transfus 2023 Epub ahead of print
- [CrossRef] [Google Scholar]
- The Urgent Need to Implement Patient Blood Management: Policy Brief. 2021. Geneva: WHO; Available from: https://iris.who.int/bitstream/handle/10665/346655/9789240035744-eng.pdf?sequence=1 [Last accessed on 2024 Jan 06]
- [Google Scholar]
- Patient Blood Management in Cardiac Surgery and ECMO: The Indian Scenario in 2021. J Card Crit Care TSS. 2021;5:181-3.
- [CrossRef] [Google Scholar]
- Implementation of a “Patient Blood Management” Program in Medium Sized Hospitals: Results of a Survey among German Hemotherapists. Health Sci Rep. 2022;5:e924.
- [CrossRef] [PubMed] [Google Scholar]
- ERAS Cardiac Society Turnkey Order Set for Patient Blood Management: Proceedings from the AATS ERAS Conclave 2023. J Thorac Cardiovasc Surg 2023:S0022-5223(23)00991-1. Epub ahead of print. doi: 10.1016/j.jtcvs.2023.10.034
- [CrossRef] [Google Scholar]
- Massive Transfusion/Haemorrhage Protocols versus Goal-directed Bleeding Management: Science Gone Eerie? J Card Crit Care TSS. 2024;8:16-27.
- [Google Scholar]
- Patient Blood Management: Moving above and Beyond the Optimal Use of Blood! J Card Crit Care TSS. 2024;8:28-32.
- [Google Scholar]





