Translate this page into:
Heparin-Induced Fever in a Cardiac Transplant Candidate
Payal Rohit Patel, MD Department of Internal Medicine, Washington University in Saint Louis/Barnes-Jewish Hospital Saint Louis, MO 63110 United States p.payal@wustl.edu
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Patient admitted to intensive care units frequently have fevers. A less common cause for fever is a drug-induced fever. For patients who are candidates for heart transplantation, persistent fevers can place a hold on their transplant candidacy until the etiology is found and the fevers resolve. We present a case of a patient with dilated cardiomyopathy who experienced fevers thought secondary to heparin that improved only with discontinuation of therapy and later underwent successful heart transplantation. Only three prior case reports of heparin-induced fevers are currently described in literature.
Keywords
cardiac transplant
cardiogenic shock
drug fever
heparin
hyperthermia
Introduction
It is estimated 50 to 75% of patients admitted in the intensive care unit (ICU) will develop a fever, defined as a core temperature elevation greater than or equal to 38°C (100.4°F).1, 2 For patients in the ICU, half of all fevers are thought to be from an infectious source and the remainder from etiologies including organ ischemia, thrombosis, neoplasia, medications, procedures, and blood transfusions.1 In cardiac care units, common causes of noninfectious fevers include myocardial infarction, pericarditis, hemorrhage, thromboembolism, and antiarrhythmic medications.2
A less commonly considered cause for fever is drug-related fever, which is estimated to be responsible for 3 to 7% of all febrile episodes.1 The definitive diagnosis is established by the temporal relationship between the fever pattern and the onset and cessation of the culprit drug.1 Although drug fevers can be associated with eosinophilia and skin rash, these are only demonstrated in 22 and 18% of patients, respectively, making it challenging to definitively diagnose drug-fever without discontinuing potentially necessary therapy.1
We present the following case of presumed heparin-induced fever in a patient admitted for cardiogenic shock who required mechanical support with the veno-arterial (V-A) extracorporeal membrane oxygenation (ECMO) followed by Impella 5.5 (Abiomed Inc, Danvers, Massachusetts, United States). Only after discontinuing heparin, the patient defervesced and underwent successful heart transplantation.
Case Presentation
The patient, a 34-year-old male with past medical history of nonischemic cardiomyopathy, ventricular tachycardia, and atrial fibrillation was transferred to our facility from an outside hospital for refractory ventricular arrhythmia. Heparin was started for history of atrial fibrillation on day 1 of admission. From days 1 to 24, the patient had intermittent mild temperature elevations to a maximum of 37.7°C (99.9°F). Due to concern for worsening cardiogenic shock, a balloon pump was inserted, and the patient was listed for heart transplantation.
On day 25, he developed a low-grade fever of 38.9°C (102°F) (Fig. 1). Due to some loose stools, Clostridioides difficile was tested and returned negative. On day 30, he developed a fever of 39°C (102.2°F) with chills and a mild cough. A full infectious workup including blood culture, urine culture, stool culture, sputum culture, and chest imaging was obtained and unremarkable. Broad spectrum antibiotics (vancomycin and cefepime) were initiated for a presumed infection. On day 31, he had a fever of 40°C (104°F) associated with leukocytosis and clinical deterioration. He was transferred to the cardiothoracic ICU for V-A ECMO support secondary to progressing cardiogenic shock and his transplant status was downgraded. On day 32, an Impella 5.5 was placed for additional cardiac support and ECMO weaning.
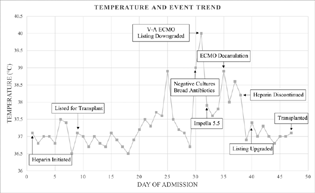
- Temperature trend and course of events leading to transplantation.
Due to persistent fevers with negative infectious evaluation, infectious diseases was consulted and recommended repeat evaluation including blood culture, fungal culture, urine culture, tracheal aspirate, chest/abdomen/pelvic imaging, cardiac imaging, and repeat testing for human immunodeficiency virus, cytomegalovirus, hepatitis, and tuberculosis; all of these returned negative. Antibiotics were further broadened to linezolid, micafungin, and meropenem to cover resistant and fungal organisms. He was successfully decannulated from ECMO on day 36 and continued mechanical support with the Impella 5.5.
Febrile episodes persisted despite clinical improvement, broad spectrum antibiotics, multiple negative infectious workups, and negative imaging. His transplant remained on hold until the etiology of the fever was determined. Given the negative infectious evaluation, a drug fever was suspected, and a complete medication review was performed. Heparin was identified as a potential cause for drug-related fever as it was the only medication consistently given throughout the admission and was discontinued on day 38. Systematic anticoagulation was changed to bivalirudin, and the patient's Impella purge solution fluid was switched from heparin to D5. Within 24 hours the patient became afebrile and remained afebrile during admission. On day 40, his heart transplantation status was upgraded, a donor was identified, and he underwent successful orthotopic heart transplantation on day 47.
Discussion
The diagnosis of drug-induced fever is challenging given the necessity to exclude other causes. A definite diagnosis is only made when discontinuing the offending medication causes cessation of fevers and confirmed when rechallenging the patient with the medication reproduces fever.3 Given the timing of defervescence to cessation of heparin and otherwise negative evaluation for infectious and noninfectious causes, we believe our patient experienced drug-related fevers from heparin.
Drug-related fevers occur an average of 21 days (median of 8 days) after medication administration and present with a waxing and waning pattern of remittent and intermittent fevers.1, 3 The fevers can vary from low-grade temperatures of 37.2°C (99°F) to 42.7°C (109°F) with patients having nonspecific symptoms such as chills or remaining asymptomatic.3 Three prior case reports have documented drug fever secondary to heparin with fever onset between 10 to 14 days of medication initiation and defervescence within 48 hours of discontinuation.4, 5, 6 In our case, the patient had intermittent low-grade fevers to 37.5°C (99.5°F) prior to an escalation to 38.8°C (102°F) on day 24 and defervesced 24 hours after heparin was stopped.
Furthermore, patients with drug-related fever can experience relative bradycardia, known as Faget sign. For each degree elevation in Fahrenheit temperature above > 38.9°C (101°F) for patients in sinus rhythm, there is an expected heart rate increase of 8 to 10 beats per minute (bpm).7 The estimated range for heart rate at 38.9°C (102.0°F) is 116 to 120 bpm and at 40°C (104°F) is 132 to 140 bpm; however, our patient's maximum heart rate was 86 and 116 bpm, respectively, demonstrating a relative bradycardia.
Additionally, our patient was unable to tolerate heparin for his Impella 5.5, which is the recommended choice for anticoagulation. For patients who cannot tolerate heparin, D5 only in the purge solution combined with systematic anticoagulation via direct thrombin inhibitors is often utilized.8 For our patient, D5 only was initially used with systematic bivalirudin; however, due to pump thrombosis requiring tissue plasminogen activator, bivalirudin was mixed in dextrose for the purge solution without recurrence of pump thrombosis.
Hospitalized patients with refractory cardiogenic shock despite maximum inotrope treatment and mechanical circulatory support are frequently considered for heart transplantation.9 Unfortunately, patients who may benefit from transplantation may not be considered if they have contraindications including active infection, cirrhosis, kidney disease, uncontrolled diabetes, active malignancy, severe lung disease, morbid obesity, and psychosocial factors.10 Our patient presented the unique challenge of fevers interfering with his candidacy for heart transplantation. According to the American Society of Transplantation Infectious Diseases, evidence of an active infection, in a solid organ transplant candidate, should prompt delay in transplantation until it is treated or controlled.10 Although no infectious source was identified for our patient, persistent fevers raised concern for occult infection prompting delay in accepting offers for transplantation and prolonging hospitalization. Only after suspecting a drug-related fever, identifying heparin as a potential cause, and discontinuing the medication did the patient remain afebrile and able to restore his candidacy for transplantation.
Conclusion
In conclusion, this case demonstrates a patient in cardiogenic shock with suspected heparin-induced fever awaiting heart transplantation and the importance of considering noninfectious etiologies for fever in critically ill patients. Only after heparin was discontinued with defervescence, the patient was able to be actively listed for transplantation and undergo heart transplantation
Conflict of Interest
None declared.
Funding None.
References
- Approach to the febrile patient in the ICU. Infect Dis Clin North Am. 2009;23(3):471-484.
- [Google Scholar]
- Approach to Managing Febrile Patients in the ICU. Gen Med (Los Angeles). 2016;4(5):274.
- [Google Scholar]
- Heparin-induced fever: a case report and literature review. J Burn Care Res. 2019;40(5):723-724.
- [Google Scholar]
- Heparin-induced fever in neurointensive care unit: a rarity yet a possibility. J Neuroanaesth Crit Care. 2022;9:53-55.
- [Google Scholar]
- Utilization of a dextrose-only purge solution for an LVAD in patients with suspected HIT: a case series. J Pharm Pract. 2021;34(6):966-969.
- [Google Scholar]
- The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010;29(8):914-956.
- [Google Scholar]
- Screening of donor and candidate prior to solid organ transplantation-guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13548.
- [Google Scholar]






