Translate this page into:
Anesthetic and Extracorporeal Management of Aortic Valve Replacement with Concurrent Oral Malignancy: A Case Report and Review of Literature
*Corresponding author: Devishree Das, Department of Anaesthesiology and Critical Care, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. devishreedas111@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Das D, Patra T. Anesthetic and Extracorporeal Management of Aortic Valve Replacement with Concurrent Oral Malignancy: A Case Report and Review of Literature. J Card Crit Care TSS. doi: 10.25259/JCCC_44_2024
Abstract
Advancement of medical management warrants the survival of cancer patients. Moreover, the cardiovascular abnormality is concurrently detected as a result of oncological therapy-induced cardiotoxicity, due to impaired immunity, prevailing infection or due to accelerated degeneration. Furthermore, extracorporeal circulation exaggerates the inflammatory and immunologic response, and therefore a potential challenge to anesthesia care giver. We hereby, describe anesthetic consideration of a patient with active oral malignancy posted for aortic valve replacement and also review extracorporeal perturbation in response to malignancy.
Keywords
Aortic valve replacement
Cardiac surgery
Extracorporeal circulation
Malignancy
INTRODUCTION
The rising prevalence of cardiovascular abnormalities in the oncology setting is due to aging and chemotherapy-induced accelerated degeneration, shared risk factors, chemotherapy or radiotherapy-induced cardiotoxicity, improved diagnostics, and therapeutic approaches leading to increased survival.[1-3] However, concurrent active malignancy and associated cardiac abnormalities have a grave prognosis and warrant immediate intervention. In-hospital mortality among patients with collateral malignancy and undergoing cardiac surgeries is very high almost 4.1–17%.[4-6] Furthermore, there are scarce data regarding effect of cardiopulmonary bypass (CPB) on active malignancy and vice versa.[7,8] Therefore, we will discuss anesthetic challenges in an active oral cavity cancer patient undergoing cardiac surgery under CPB and also review extracorporeal consequences that affect perioperative management.
CASE REPORT
A 53-year-old male patient with squamous cell carcinoma of buccal mucosa and severe aortic stenosis was admitted for aortic valve replacement (AVR) followed by surgical resection of carcinoma. The patient had an ulcero-indurative lesion of 2.5 × 1.5 cm over the right retromolar trigone extending to the soft palate and alveolus since 3 years. Contrast-enhanced computed tomography revealed heterogeneous enhancing neoplastic lesion of 15 × 20 × 16 mm in retromolar trigone extending laterally into adjacent gingiva-buccal sulcus and medially up to oral gingiva with adjacent maxillary erosion and level II lymph node involvement. Biopsy confirmed moderately differentiated keratinized type squamous cell carcinoma and planned for tumor resection. Meanwhile, the patient presented with the left-sided chest pain and on echocardiography, severe aortic stenosis with a mean gradient of 80 mm of Hg and cuspal prolapse was found. Angiography revealed normal coronaries.
Anesthetic challenges were severe aortic stenosis with concomitant buccal carcinoma, friable buccal lesion, bleeding during intubation and transesophageal echocardiography (TEE) probe placement, extracorporeal-induced exaggeration of inflammation and complement activation, and coagulation abnormalities. Therefore, the patient was started on beta blockers and low-molecular-weight heparin as thromboprophylaxis. After optimization, the patient was taken up for AVR. A Multipara monitor was attached and large bore intravenous access was taken. Left-sided radial arterial line was secured. A balanced anesthesia technique was used for induction with injection midazolam, fentanyl, and etomidate, and intubation was facilitated with muscle relaxant Rocuronium. The patient was intubated with 8.5 mm ID endotracheal tube by direct visualization with C-Mac video laryngoscope to avoid direct trauma to the friable buccal mucosa. Similarly, TEE probe was inserted visualizing the denuded mucosa by C-Mac video laryngoscope [Figure 1]. Right internal jugular vein access was taken and patient’s hemodynamic was well maintained during the intraoperative period.
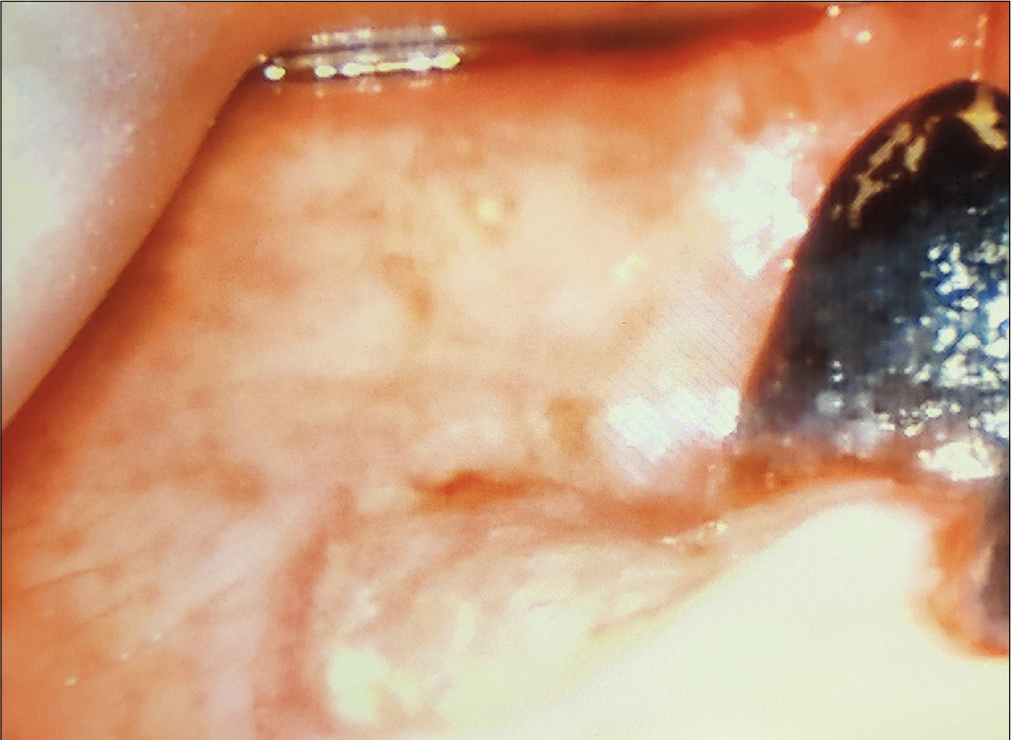
- C-Mac video laryngoscopic view showing the friable buccal mucosa.
Intraoperative TEE examination was performed using adult TEE probe (GE 7T) and ultrasound machine (GE Vivid E95 model: GE Vingmed Ultrasound AS, Horten, Norway). In the mid esophageal (ME) aortic valve (AoV) short axis view, vegetation was found to be popping out and an cavitary lesion suggesting old abscess was demonstrated in the junction of the left and right coronary cusp [Figure 2 and Video 1]. In the ME 5-chamber view, vegetation was found to arise from AoV [Figure 3 and Video 2]. ME AoV long axis view delineates the vegetation, abscess cavity, and degenerative changes of AoV [Figure 4]. On color Doppler interrogation, flow turbulence was noted across the AoV along with one regurgitant jet [Figure 5]. TEE not only gives the detailed anatomy of AoV but also illustrates the underlying pathology clearly. Therefore, the diagnosis of degenerative aortic stenosis changed to infective endocarditis of AoV with vegetation and abscess cavity. Although, TEE is necessary during perioperative period, utmost care should be taken during its insertion and it should be inserted under direct vision without injuring the ulcerative mucosa.
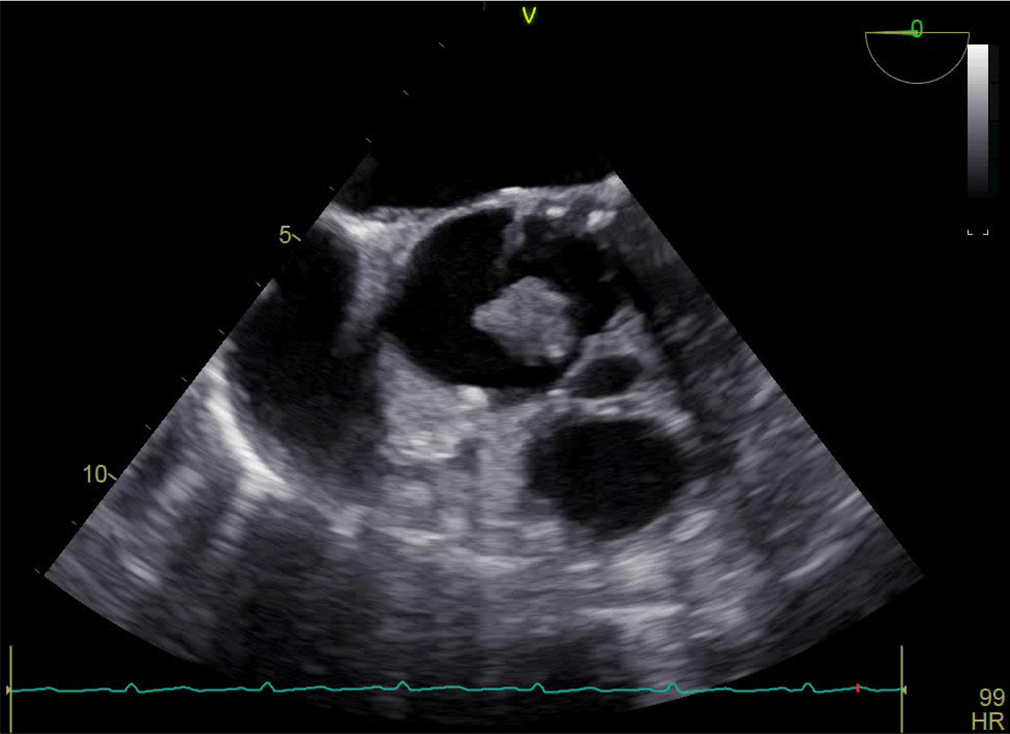
- Mid esophageal aortic valve short axis echocardiographic view illustrating vegetation and a cavitary lesion in the junction of left and right coronary cusp.
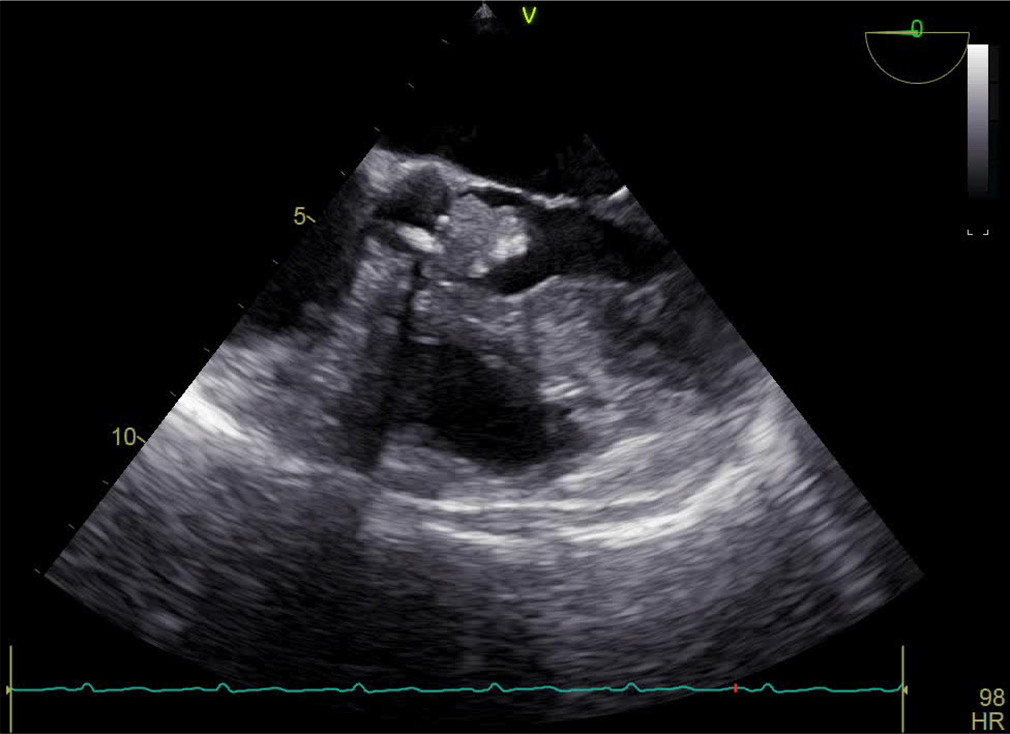
- Mid esophageal five-chamber view, demonstrating vegetation arising from aortic valve.
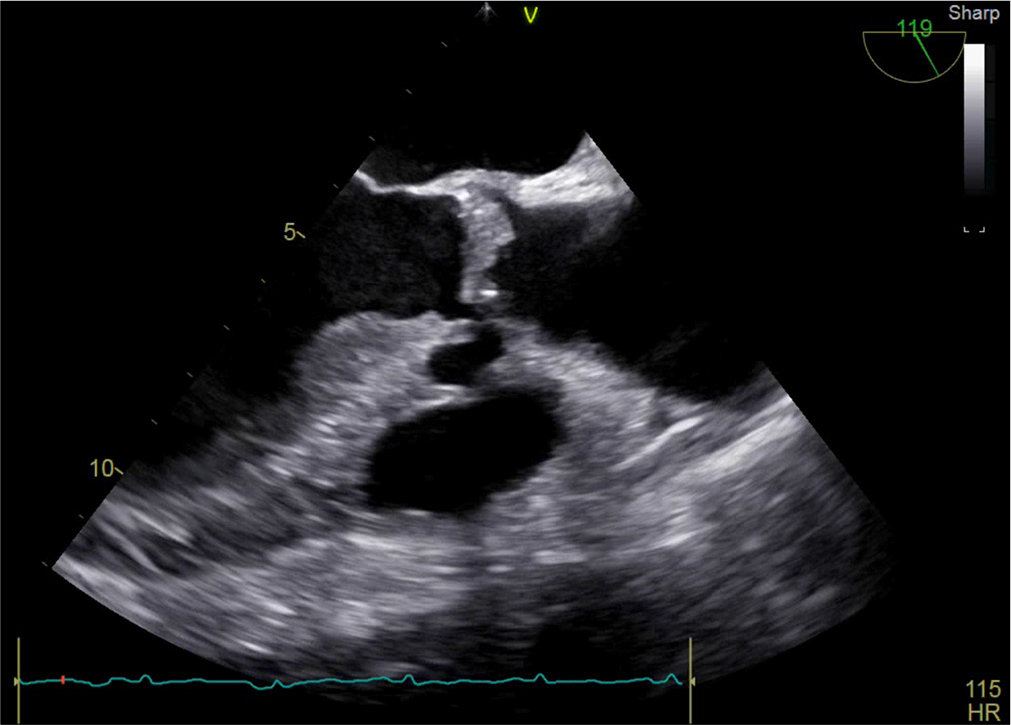
- Mid esophageal aortic valve (AoV) long axis view delineating vegetation, abscess cavity, and degenerative changes of AoV.
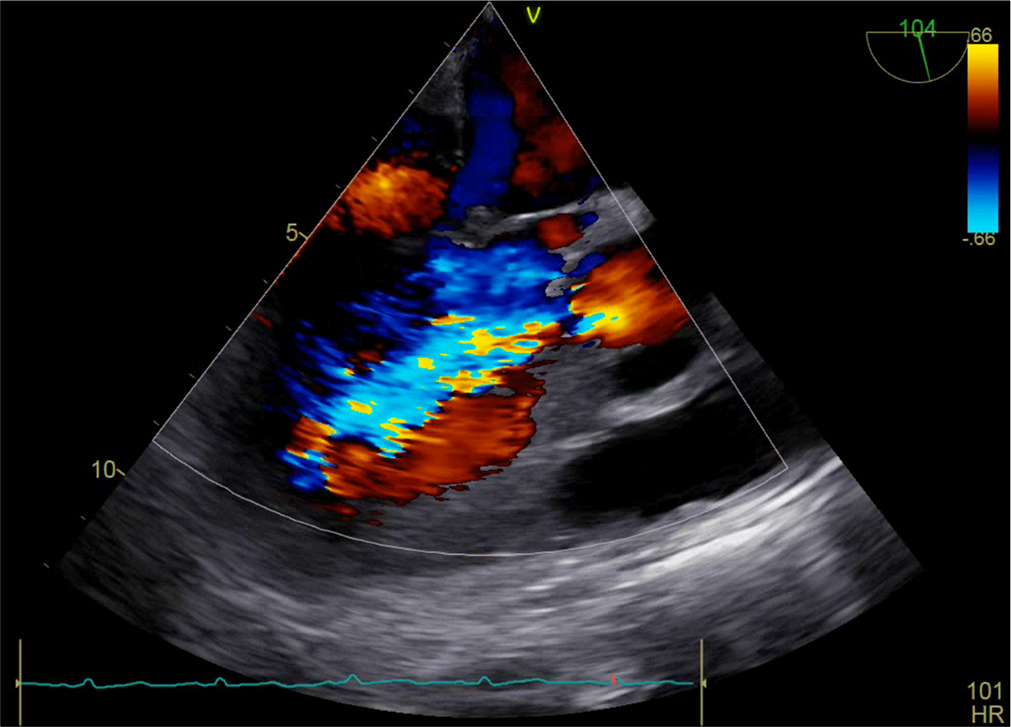
- Mid esophageal, aortic valve (AoV), long axis view with color Doppler interrogation revealing flow turbulence across the AoV along with regurgitant jet.
Video 1:
Video 1:Mid esophageal 5-chamber view, demonstrating vegetation arising from aortic valve.Video 2:
Video 2:Mid esophageal, aortic valve, and short axis view along with orthogonal comparison illustrating vegetation and a cavitary lesion in the junction of left and right coronary cusp.After adequate heparinization, CPB was started. Injection tranexamic acid was given thrice, that is, before commencement of CPB, on institution of CPB and after weaning from CPB to prevent exaggeration of extracorporeal inflammation. The vegetation, as well as the degenerative AoV was resected and replaced with 21# size bileaflet mechanical prosthetic AoV. The aortic cross-clamp and CPB time were 110 and 150 minutes, respectively. The patient was weaned with the support of dobutamine 5 mcg/kg/min and nitroglycerin 0.5 mcg/kg/min. Post-CPB, TEE revealed normal movement of leaflets, without paravalvular leak and a mean gradient of 19 mm of Hg. After protamine neutralization, adequate hemostasis, and video laryngoscope-guided inspection of oral mucosa, the patient was shifted to intensive care unit (ICU) for further post-operative management. Broad spectrum antibiotics started and blood culture was sent for further management. Gentle oral suction was allowed in the ICU and to inform if any oral bleeding. The patient was extubated after 8 h of mechanical ventilation and early mobilization was started. Oral anticoagulant “Nicoumalone” was given to maintain INR 1.5–2. The patient was discharged from the hospital after 6 days, and he underwent tumor resection after 3 months.
DISCUSSION
Epidemiology of malignancies with concurrent heart disease
The incidence of malignancy with concurrent heart disease ranges from 3.4% to 7%, whereas 1.9% and 4.2% cancer patients require cardiac surgery.[5,9] Breast, colon, prostate, and bladder carcinoma constitute almost 70–83% of all malignancies requiring cardiac intervention, out of which 68–83% are active solid organ tumor and 7–17% hematological tumor.[6]
Chemoradiotherapy and cardiovascular complications
Chemoradiotherapy tailored multiple cardiovascular and pulmonary complications such as myocardial fibrosis with special predilection to the aortic or mitral valve, aortic calcification, intimal proliferation of great vessel, supra-aortic arch vasculopathy involving carotid and subclavian arteries, pleural and pericardial effusion, coronary vasospasm, radiation-induced fibrosis of internal mammary artery, diffuse interstitial fibrosis, and pneumonia which influence the perioperative course [Tables 1 and 2][10]
| Chemotherapy agents | Cardiotoxic effect | |
|---|---|---|
| Anthracycline | ||
| 1. | Doxorubicin | LV dysfunction/CHF/Arrhythmias/Cardiomyopathies |
| 2. | Daunorubicin | LV dysfunction/CHF/Arrhythmias |
| 3. | Epirubicin | LV dysfunction/CHF/Arrhythmias |
| Alkylating agents | ||
| 1. | Cyclophosphamide | Cardiac Tamponade/Arrhythmias/CHF |
| 2. | Bleomycin | Myocardial Ischemia |
| 3. | Melphalan | Acute cardiomyopathy |
| Platinum based agents | ||
| 1. | Cisplatin | HTN/CAD/Thromboembolic Events/Angina/CHF/Arrhythmias |
| Antimicrotubular agent | ||
| 1. | Paclitaxel | Arrhythmia/Heart block, CHF |
| 2. | Vinblastine | Angina/Myocardial Ischemia |
| Antimetabolites | ||
| 1. | 5-fluorouracil | Angina/MI/Arrhythmias/Cardiomyopathy/CHF |
CHF: Congestive heart failure, CAD: Coronary artery disease, HTN: Hypertension, LV: Left ventricle, MI: Myocardial infarction
| Type 1 | Irreversible myocardial damage, dose dependent cardiotoxicity (e.g. anthracyclines) |
| Type 2 | Reversible myocardial damage, dose independent myocardial injury (e.g. trastuzumab) |
| Type 3 | Coronary artery disease due to radiation exposure or vasospasm (e.g. radiation therapy and 5-fluorouracil) |
| Type 4 | Miscellaneous such as myocarditis or Takotsubo’s cardiomyopathy (e.g. 5-fluorouracil and tyrosine kinase inhibitors) |
| Type 5 | Indirect secondary to conduction abnormalities, arrhythmias, and hypertension (e.g. ibrutinib, 5-fluorouracil, and platinum-based therapy) |
Onco therapy and coagulation disorders
Malignancy per se has a prothrombotic or prohemorrhagic effect, which is further enhanced with various chemotherapeutic agents. These effects are more pronounced in cardiac surgery, where anticoagulants and extracorporeal circuits are used. However, thrombosis is more common, especially in myeloproliferative cancers, than hemorrhagic phenomenon. Procoagulant tissue factor is the major culprit but other procoagulants can directly activate factor X, inducing local and systemic thrombosis. Hence, proper care such as early mobilization, intermittent compression device, and low-molecular-weight heparin prophylaxis addressed for avoiding deep vein thrombosis, pulmonary embolism, and major arterial thrombosis.
Malignancy and extracorporeal circulation
Extracorporeal circulation induces whole-body inflammatory reaction by activation of proinflammatory cytokines, and complement system. Therefore, the major concern in approaching cancer patients for cardiac surgery under CPB is the exaggeration of inflammatory reactions. Both in vitro and in vivo studies have illustrated that surgical stress as well as extracorporeal exposure, further suppress of the immune system. Furthermore, elevated levels of IL-10 and transforming growth factor-b inhibiting T-cell, macrophage, and natural killer cell activity have also been reported. However, the correlation between extracorporeal circulation and tumor progression has not been clearly demonstrated yet. Schoenmakers et al. proclaimed no significant alteration in early and late outcomes between on-pump and off-pump coronary artery bypass grafting and lung resection.[11] Similarly, Suzuki et al. concluded that there were no adverse effects of CPB on cancer progression during a period of 5 years follow-up.[8]
Perioperative management strategy
Technological advancement and multimodal, multidisciplinary management enable the survival of cancer patients undergoing cardiac surgery. However, certain factors should be considered during the perioperative course [Table 3].[12]
| S. No | Anesthetic Consideration | Anesthetic management |
|---|---|---|
| 1. | Multiorgan involvement | • Multidisciplinary involvement is required. • Maintain Perioperative Hemodynamic stability. |
| 2. | Cardiotoxicity effect of Chemotherapeutic Agents | • Updated Knowledge of various Chemotherapeutic Agents and their Cardiotoxicity effect. • Detailed evaluation of patient. • Incorporation of global longitudinal strain, 4D ejection fraction, cardiac biomarkers. |
| 3. | Abnormal Coagulation pathway | • Evaluation of prothrombotic or pro-haemorrhagic state. • Coagulation management should be optimised. |
| 4. | No appropriate risk stratification model | • Further research is needed for concurrent malignancy and cardiac diseases. • New risk stratification model for incorporation of malignancy should be developed. |
| 5. | Inconclusive evidence on impact of extracorporeal circulation | • Further research is required to detailed evaluation of extracorporeal circulation and malignancy. |
| 6. | Exaggerated inflammatory response | • Measures to decrease inflammation on CPB should be incorporated. |
CPB: Cardiopulmonary bypass
Detailed history pertinent to malignancy, organ involvements, tumor progression, active or relapse tumor, chemoradiotherapy, hematologic or pulmonary involvement, along with its impact on cardiovascular system, surgical planning, anticipated post-operative complications, and long-term outcome should be thoroughly assessed.
Before cardiac surgery prothrombotic or prohemorrhagic state should be evaluated and prophylaxis should be started preoperatively.
The extent of cardiovascular involvement, biventricular function, and risk stratification though Euro Score and society of thoracic surgery (STS) score does not include cancer, and subsequent risk-benefit analysis should be done to optimize the patient before surgery. The patient should be screened all before planning for surgery with the electrocardiogram, cardiac biomarker, especially troponin level, and biventricular function assessment with an echocardiogram including global longitudinal strain, and, 4D ejection fraction.
Although conclusive evidence on the impact of extracorporeal circulation is not available, anticipated complications, organ dysfunction, exaggerated inflammation, and longer ventilator requirements are critical.
Particular attention with regard to anticipated coagulation disorders on CPB, its monitoring, and management is required.
Special care to be given when hematological malignancy and pulmonary involvement is present; therefore, decision-making and patient selection are crucial.
Pain management, nutritional supplements, palliative care, and especially psychosocial support are the most important determinants for patient satisfaction and better outcomes.
Multidisciplinary team involving medical, radiation and surgical oncology, cardiac anesthesiology, and cardiothoracic vascular surgery is required for better patient management.
Early and late outcomes
In a study by Chan et al. where the authors demonstrated a higher rate of blood transfusion (80% vs. 49%), occurrence of atrial fibrillation postoperatively (42.2% vs. 33.8%), cerebrovascular accidents (2.4% vs. 0%), pulmonary complications (14.5% vs. 6%), requirement of reintubation (8.4% vs. 0.9%), and a higher sepsis rate (8.4% vs. 1.9%) in patients having malignancy as compared to patients without malignancy undergoing cardiac surgery.[9] Moreover, patients with hematological malignancies confer a higher almost 14.3% to 18.7% hospital mortality rates. Symptomatic patients with aortic stenosis scheduled for intermediate or high risk non cardiac surgery should undergo surgical AVR or transcatheter aortic valve implantation (according to the 2021 European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines for the management of Valvular heart disease [VHD]) (class I, level C). Multiple studies concluded that no surgery for oral cancer has poor outcome and 5 year survival is around 15–45% if the patient undergone surgery.
Carrascal et al. demonstrated that post-operative survival is predominantly depended on pre-operative left ventricular function and presence of chronic pulmonary pathology, and the time span between cancer detection and planning of surgery.[5]
CONCLUSION
Concurrent active malignancy and cardiac surgery under CPB require proper planning by a multidisciplinary approach as each step possesses potential challenges to the caregivers. Early diagnosis and management is the key dictum as with the progression of the left ventricle dysfunction, morbidity and mortality increase. There are a lot of grey areas in the management of cancer patients undergoing cardiac surgery; therefore, multiple study and clinical trials are required to enlighten with knowledge.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cardiovascular Toxic Effects of Targeted Cancer Therapies. N Engl J Med. 2016;375:1457-67.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term Survival of Patients with Radiation Heart Disease Undergoing Cardiac Surgery: A Cohort Study. Circulation. 2013;127:1476-84.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular Complications of Radiation Therapy for Thoracic Malignancies: The Role for Non-invasive Imaging for Detection of Cardiovascular Disease. Eur Heart J. 2014;35:612-23.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Prior Malignancy on Survival after Cardiac Surgery. Ann Thorac Surg. 2004;77:1593-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Surgery with Extracorporeal Circulation in Cancer Patients: Influence on Surgical Morbidity and Mortality and on Survival. Rev Esp Cardiol. 2008;61:369-75.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Surgery with Extracorporeal Circulation and Concomitant Malignancy: Early and Long-term Results. J Cardiovasc Med (Hagerstown). 2016;17:152-9.
- [CrossRef] [PubMed] [Google Scholar]
- In vitro Evaluation of the Effect of Cardiac Surgery on Cancer Cell Proliferation. Ann Thorac Cardiovasc Surg. 2011;17:260-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Cardiopulmonary Bypass on Cancer Prognosis. Asian Cardiovasc Thorac Ann. 2010;18:536-40.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Surgery in Patients with a History of Malignancy: Increased Complication Rate but Similar Mortality. Heart Lung Circ. 2012;21:255-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer Therapy-related Cardiac Dysfunction: An Overview for the Clinician. Clin Med Insights Cardiol. 2019;13:1179546819866445.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of On-pump or Off-pump Coronary Artery Revascularization with Lung Resection. Ann Thorac Surg. 2007;84:504-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Surgery in Adult Patients with Remitted or Active Malignancies: A Review of Preoperative Screening, Surgical Management and Short-and Long-term Postoperative Results. Eur J Cardiothorac Surg. 2018;54:10-8.
- [CrossRef] [PubMed] [Google Scholar]






