Translate this page into:
Quadruple Valve Replacement for Congenital and Rheumatic Valvular Heart Disease
*Corresponding author: Ajmer Singh, Department of Cardiac Anaesthesia, Institute of Critical Care and Anesthesiology, Medanta The Medicity, Gurugram, Haryana, India. ajmersingh@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Singh A, Nanda C, Mukati R, Mehta Y. Quadruple Valve Replacement for Congenital and Rheumatic Valvular Heart Disease. J Card Crit Care TSS. doi: 10.25259/JCCC_50_2024
Abstract
A 38-year-old female presented to our institution for recurrent symptoms of heart failure. There was a history of a palliative procedure followed by corrective surgery for tetralogy of Fallot in childhood. Transthoracic echocardiography demonstrated severe mitral stenosis, moderate mitral regurgitation, severe aortic regurgitation, severe tricuspid regurgitation, and free pulmonary regurgitation. She underwent the replacement of all four valves with mechanical prostheses in a single operation uneventfully. Follow-up visits at 3 months and 6 months revealed normal functioning of all four valves.
Keywords
Mechanical valves
Quadruple valve replacement
Rheumatic heart disease
Tetralogy of Fallot
INTRODUCTION
Rheumatic heart disease, resulting from rheumatic fever, is the predominant etiology of valvular heart disease (VHD) in India. It generally affects more than one valve. Rheumatic VHD usually influences the mitral, aortic, and sometimes tricuspid valve (TV); but rarely affects the pulmonary valve.[1] The pulmonary valve is generally affected by congenital heart diseases, most often after surgical correction of tetralogy of Fallot. Carcinoid heart disease, on the contrary, usually affects the tricuspid and pulmonary valves and typically spares the left-sided heart valves.[2] Extensive infective endocarditis can also lead to degeneration of all valves. For patients with VHD, medical therapy can only reduce the symptoms caused by heart failure. Surgery or endovascular intervention is generally required if symptoms persist despite optimum medical treatment. The involvement of all four valves that require surgery is not very common. Quadruple valve replacement (QVR) can potentially lead to an increased risk of morbidity and mortality. The early morbidity is related to long cardiopulmonary bypass (CPB) time and myocardial ischemia. Any underlying myocardial dysfunction caused by multivalvular disease can potentially worsen the outcome of the surgery.
We describe here a patient who required QVR for congenital and rheumatic VHD that affected all four valves.
CASE REPORT
A 38-year-old female, weighing 42 kg, was admitted to our institution for worsening of her heart failure symptoms (New York Heart Association class III-IV). There was a history of a palliative surgery followed by total correction of tetralogy of Fallot in childhood. At 20 years of age, she suffered from rheumatic fever. For the last 2 years, she had progressive dyspnea, palpitations, swelling of feet, and loss of weight, requiring hospital admission twice for heart failure. On physical examination, she looked undernourished and had grade 2 (moderate) ascites and bilateral pedal edema. Her heart rate was 60 beats/min, rhythm was atrial fibrillation with controlled ventricular rate, and blood pressure was 106/50 mmHg. Pre-operative laboratory investigations showed normal complete blood count, thyroid function, renal function, and serum electrolytes results. Serum albumin was low (2.4 g/dL) and the N-terminal pro-B natriuretic peptide level was 3470 pg/mL. Cardiomegaly and bilateral pleural effusions were seen on the chest X-ray. Transthoracic echocardiography demonstrated an intact patch at the ventricular septal defect position with no residual lesion, well-opened right ventricular outflow tract, free (severe) pulmonary regurgitation, pulmonary artery systolic pressure of 54 mmHg, severe tricuspid regurgitation, and right ventricular dysfunction with tricuspid annular plane systolic excursion of 1.4 cm. In addition, the leaflets of mitral and aortic valves were thickened and fibrosed, resulting in severe mitral stenosis (mitral valve area 0.8 cm2 by planimetry, mean pressure gradient 12 mmHg), moderate mitral regurgitation, and severe aortic regurgitation. The left ventricular enddiastolic dimension was 53 mm, with global hypokinesia and an ejection fraction of 45%. Pre-operative medications aimed to treat heart failure, control heart rate, promote diuresis, and maintain electrolyte balance, included oral diltiazem 30 mg thrice a day, spironolactone 25 mg once a day, and torsemide plus (torsemide 20 mg + spironolactone 50 mg) once a day. In view of her diagnosis, symptoms, and echocardiographic findings, she was advised for an early surgery. The calculated European system for cardiac operative risk evaluation II (EuroSCORE) was 10.02%. The patient was explained about the pros and cons of QVR, the need for life-long anticoagulation, and regular follow-up; and informed consent was obtained.
Under standard cardiac monitoring, including intraoperative transesophageal echocardiography, midline sternotomy was performed. Transesophageal echocardiography findings for valvular pathologies were consistent with transthoracic echocardiography [Figure 1-4]. CPB was instituted by aortobicaval cannulation and myocardial protection was achieved with del Nido cardioplegia and systemic hypothermia (28°C temperature). After the replacement of the mitral valve (25 mm St Jude Medical, Inc.™, MN, USA), the aortic valve (23 mm St Jude Medical), and the pulmonary valve (27/29 mm ON-X Life Technologies, Inc.™, TX, USA) were replaced. The TV was replaced (27 mm St Jude Medical) after the release of the aortic cross-clamp. The aortic cross-clamp time was 153 min and the duration of CPB was 180 min. During CPB, 2.5 L of ultrafiltrate was removed, followed by 800 mL of modified ultrafiltration. The return to rhythm was spontaneous, requiring temporary pacing, and the weaning from CPB was smooth with mild inotropic support of milrinone and epinephrine. Extracorporeal membrane oxygenation (ECMO) support was on standby for the inability to wean from CPB or refractory cardiogenic shock. Post-operative echocardiography showed normal functioning of all four valves with no paravalvular leak. The mean/peak gradients across the valves were: Mitral 4/10 mmHg, aortic 15/27 mmHg, pulmonary 3/6 mmHg, and TV 2/5 mmHg. Post-operative chest radiographs showed all four mechanical prosthetic valves [Figure 5]. Postoperative anticoagulation was achieved with intravenous unfractionated heparin for the first 2 days, followed by oral warfarin therapy with a target international normalized ratio of 3.0 (range 2.5–3.5). The subsequent stay of the patient in the hospital, till her discharge on the 12th post-operative day, was unremarkable. The patient gradually gained weight and had New York Heart Association functional class I symptoms at 3-month and 6-month follow-up visits, and all four valves were functioning normally.

- Intraoperative transesophageal echocardiography Mid-esophageal (ME) long-axis view shows (a) doming of the anterior mitral leaflet and non-coaptation of aortic valve leaflets, (b) color flow Doppler shows severe aortic regurgitation.
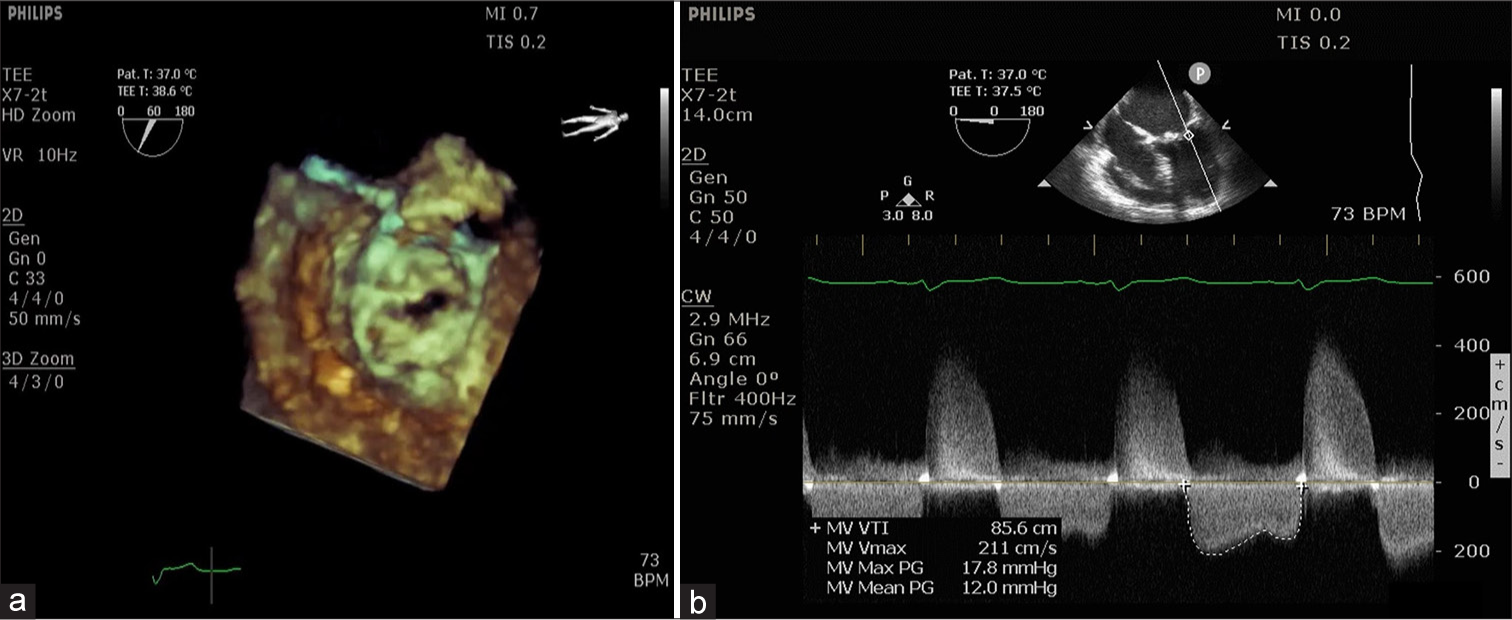
- (a) Three-dimensional en-face view of the mitral valve shows restricted opening and (b) continuous-wave Doppler at mitral valve shows severe mitral stenosis.
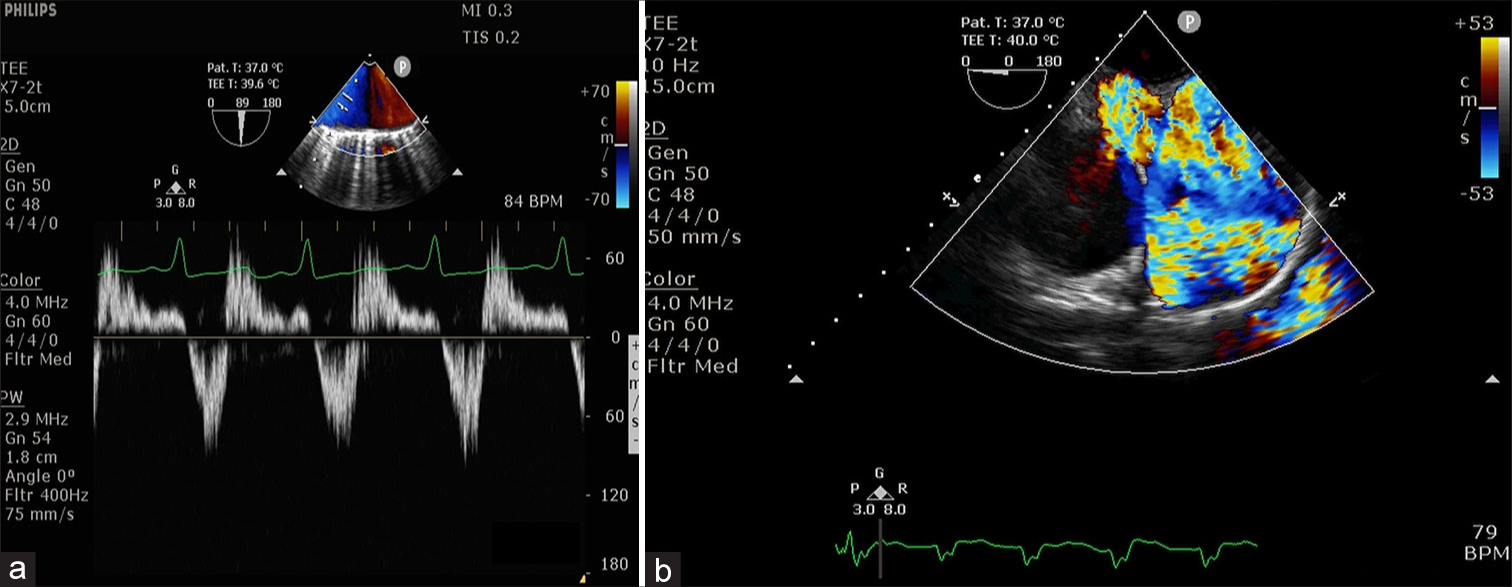
- (a) Pulse-wave Doppler at aortic arch shows diastolic flow reversal and (b) upper-esophageal ascending aorta short-axis view shows free pulmonary regurgitation.
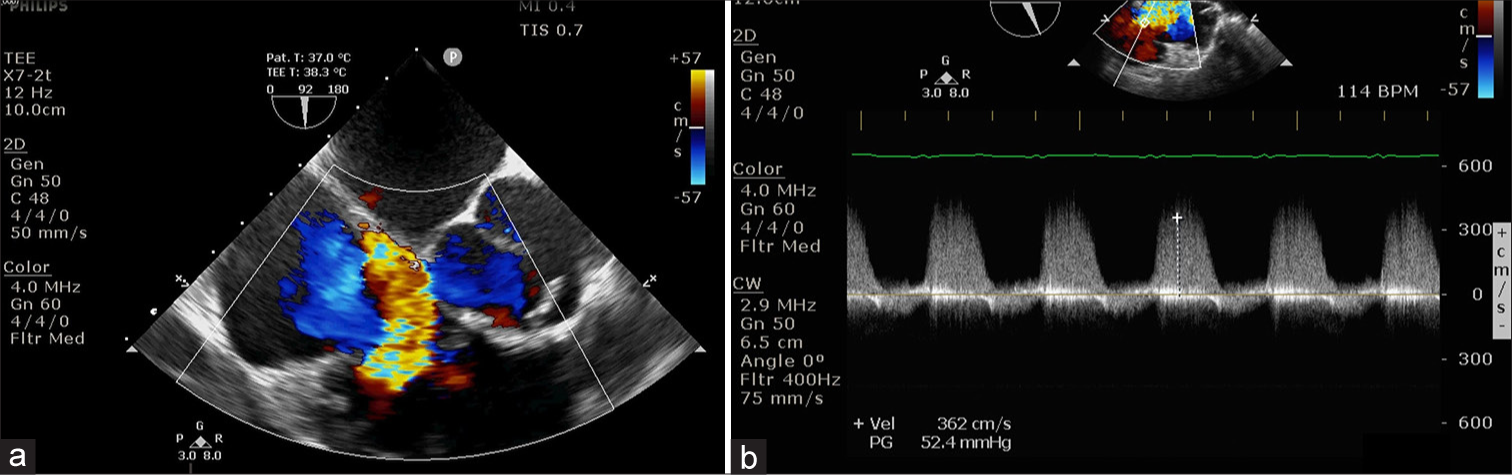
- (a) Color flow Doppler at tricuspid valve shows severe regurgitation, (b) modified bicaval view shows tricuspid regurgitation jet.
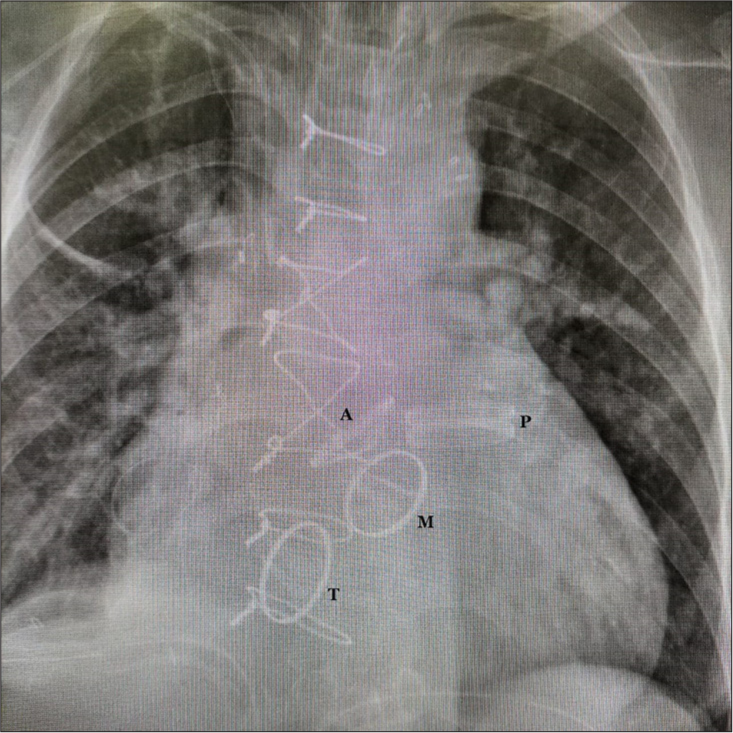
- Post-operative chest radiograph shows all four valves, P: Pulmonary, A: Aortic, M: Mitral, T: Tricuspid.
DISCUSSION
Rheumatic heart disease, carcinoid heart disease, and infective endocarditis can affect all valves requiring QVR. Hossack et al. in 1987 reported the first QVR for rheumatic VHD.[3] For carcinoid heart disease, Arghami et al. reported QVR in seven patients.[4] They opined that QVR can cause functional improvement in symptomatic patients with VHD. The perioperative outcomes after QVR have shown dramatic improvements due to better myocardial protection, improved surgical techniques, and the advances made in mechanical valve designs. Compared to the patients undergoing single or double valve replacement, QVR patients are exposed to substantially longer CPB and myocardial ischemia times, which can worsen the pre-existing ventricular dysfunction. In addition, the replacement of multiple valves exposes the patient to added long-term morbidities related to prosthetic valves, such as thromboembolism, anticoagulation-related hemorrhage, endocarditis, and paravalvular leakage.
Recently, there has been major interest in imaging myocardial fibrosis with cardiac magnetic resonance imaging (MRI). Imaging of myocardial fibrosis using Cardiac MRI has been studied in a variety of cardiovascular conditions for both diagnostic and prognostic purposes. The clinical applications of fibrosis imaging have been described in ischemic cardiomyopathy, dilated cardiomyopathy, hypertensive cardiomyopathy, myocarditis, and infiltrative diseases.[5] Among VHD, aortic stenosis is the only lesion in which Cardiac MRI can detect myocardial disease at an early, reversible stage. The patient described here did not have aortic stenosis or cardiomyopathy, hence Cardiac MRI was not performed. Cardiac MRI has emerged as the gold standard in assessing ventricular mass, volume, and systolic function, however, the data derived from it have not been validated and compared with clinical outcomes in patients with VHD.
Veno-arterial ECMO (VA-ECMO) support may be required following multivalvular surgery if there is refractory cardiogenic shock or the patient cannot be weaned from CPB. The clinical criteria of post-cardiotomy cardiogenic shock include systolic arterial hypotension (<80 mmHg) and signs of end-organ failure, anaerobic metabolism, and metabolic acidosis (potential of hydrogen [pH] <7.3, lactate level >3.0 mmol/L, and urine output <0.5 mL/kg) despite optimized supportive measures, such as intra-aortic balloon pump, inotropes, nitric oxide, and phosphodiesterase inhibitors therapy. In a retrospective study of early and mid-term results of VA-ECMO after valvular surgery, successful weaning from ECMO was achieved in 51/87 patients (59%), and 43/87 patients (49%) were discharged from the hospital.[6]
Mechanical valves can last a lifetime (>30 years) and superior long-term outcomes have been documented with the bileaflet mechanical valves. For mitral and aortic valves, mechanical prostheses are the favored choice. Based on the individual patient’s risk of bleeding, life expectancy, and future intervention, the choice of valve should be customized.[7] Bioprosthetic valves, compared to mechanical valves are prone to early degeneration. However, they can be used in patients who have limited life expectancy, or those with contraindications to warfarin due to severe hepatic dysfunction. Our patient is young, and with the possibility of further intervention in the case of a biological valve replacement, mechanical valves were deemed appropriate to reduce the need for future reoperations. With mechanical valves in both the aortic and mitral position, along with a thromboembolic risk factor (atrial fibrillation), the American College of Cardiology/American Heart Association (ACC/AHA) 2017 has recommended a target International Normalized Ratio (INR) of 3.0 (range 2.5–3.5, Grade 1B recommendation), which was followed.[8] Few Japanese and Chinese institutions have used lower INR target values (below 2.5) to minimize hemorrhagic complications in their patients. In India, because of poor compliance with the medications and socioeconomic conditions, thrombotic complications are more commonly seen than bleeding complications, hence we are advised to keep an INR of 2.5–3.5. The anticoagulation regimen needs to be fine-tuned to balance the lowest risk of bleeding with the lowest risk of thromboembolic complications. Approximately 15–20% of patients undergoing TV replacement can develop atrioventricular block, and they may need implantation of a permanent pacemaker. The decision to repair or replace the TV is based on several factors, including the extent of the disease process, the amount of salvageable leaflet tissue, concomitant procedures on other heart valves, patient age and comorbidities, and surgical expertise. Considering the complexity of the surgical procedure, and to shorten the duration of CPB, we refrained from TV repair and preferred replacement. Moreover, although the midterm mortality is higher after replacement versus repair of TV, the long-term durability of valve repair is questionable with a high recurrence rate of Tricuspid Regurgitation (TR). Follow-up echocardiograms have revealed more residual TR (moderate to severe) in the repair group (38% vs. 5%, P < 0.001).[9] Residual TR is associated with a higher biventricular failure, reoperation, and high mortality (up to 40%). Singh et al. have also found no difference between the repair and replacement groups 15 years postoperatively with regard to thromboembolism, valve thrombosis, or bleeding rates.[9] Adult patients rarely require replacement of the pulmonary valve. It is mostly required in patients with congenital heart disease, such as those who have undergone repair of tetralogy of Fallot, as happened in this patient.
The previous reports of triple valve surgery have shown a high operative mortality rate (13–25%) and suboptimal long-term outcomes, with documented survival rates of 75% and 61% at 5 years and 10 years, respectively.[10,11] For QVR surgery, large-scale studies describing the risk of mortality are not available, only a few case reports or case series are published in the literature. Cao et al. and Budak et al. have published long-term survival (11 years and 20 years respectively) without complications after QVR with mechanical valves in patients with rheumatic VHD.[12,13] They attributed the successful outcome to improved myocardial protection, better acquaintance with complex surgeries, and enhanced post-operative care. Transcatheter valve implantation can be contemplated as a suitable alternative in extremely prohibitive-risk patients.[14] There are, however, no published reports of the use of the transcatheter technique for all four valves.
Cardiac surgical procedures involving long CPB times can lead to multiorgan dysfunction in the post-operative period. The characteristic pathologies that may occur during the postoperative period include systemic inflammatory response syndrome (SIRS) after extracorporeal circulation, cardiogenic shock and low cardiac output syndrome, arrhythmia, renal injury, stroke, and respiratory distress.[15] For patients with mild symptoms, fluid supplementation, oxygen therapy, and symptomatic treatment are generally sufficient. Severe SIRS causes targeted organ damage or major organ dysfunction and should be actively treated once it occurs. Eliminating excessive inflammatory factors and inhibiting excessive inflammatory responses can block the progression of SIRS to multiple organ dysfunction syndrome. Continuous renal replacement therapy and plasma exchange can simulate the renal clearance pattern of water and solutes, and significantly remove a variety of solutes from the body. Moreover, they can remove excess inflammatory mediators and endotoxins from the body through filtration and adsorption, reduce the restimulation of inflammatory cells, and avoid the cascade reactions stimulated by inflammatory mediators. Patients with acute myocardial injury or heart failure should immediately receive high-flow oxygen therapy, intravenous diuretics, and short-term antibiotic therapy. For patients with acute lung injury, treatment should include mechanical ventilation, antibiotics, fluid restriction, and corticosteroids. At present, there are no specific treatment methods for liver failure; therefore, supportive measures such as adequate calorie supplementation, control of systemic infections, or application of a molecular adsorbent recirculation system for treating liver failure can only be administered to allow time for damaged liver cells to recover and regenerate. In patients with acute kidney injury, sufficient fluids, diuretics, and sodium bicarbonate should be administered to alkalize the urine, and symptomatic supportive treatment should be given. Hemodialysis is necessary if renal function continues to deteriorate and acute renal failure occurs.
CONCLUSION
Excellent short-term results can be achieved in patients with symptomatic quadruple VHD. These patients, however, require a regular follow-up for thromboembolism, anticoagulation-induced hemorrhage, endocarditis, and other complications.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
Dr. Yatin Mehta is on the Editorial Board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Quadruple Valve Replacement in a Patient with Severe Rheumatic Heart Disease. Echo Res Pract. 2018;5:K47-51.
- [CrossRef] [PubMed] [Google Scholar]
- Quadruple Bioprosthetic Valve Replacement in a Patient with Severe Carcinoid Heart Disease. JACC Case Rep. 2020;2:271-6.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term Follow-up of a Patient with Quadruple Valve Replacement. Tex Heart Inst J. 1987;14:315-317.
- [Google Scholar]
- Quadruple Valve Replacement in Patients with Carcinoid Heart Disease. J Thorac Cardiovasc Surg. 2010;140:1432-4.
- [CrossRef] [PubMed] [Google Scholar]
- Myocardial Fibrosis: Why Image, how to Image and Clinical Implications. Heart. 2019;105:1832-40.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of Veno-Arterial Extracorporeal Membrane Oxygenation for Patients Undergoing Valvular Surgery. PLoS One. 2013;8:e63924.
- [CrossRef] [PubMed] [Google Scholar]
- Quadruple Valve Replacement for Carcinoid Heart Disease. Braz J Cardiovasc Surg. 2018;33:398-403.
- [CrossRef] [Google Scholar]
- 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135:e1159-95.
- [CrossRef] [PubMed] [Google Scholar]
- Midterm Outcomes of Tricuspid Valve Repair Versus Replacement for Organic Tricuspid Disease. Ann Thorac Surg. 2006;82:1735-416.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple Valve Operation for Advanced Valvular Heart Disease: Results and Risk Factors in 513 Patients. J Am Coll Cardiol. 1992;19:725-32.
- [CrossRef] [PubMed] [Google Scholar]
- Short-and Long-Term Results of Triple Valve Surgery in the Modern Era. Ann Thorac Surg. 2006;81:2172-7. discussion 2177-8
- [CrossRef] [PubMed] [Google Scholar]
- Quadruple Valve Replacement with Mechanical Valves: An 11-Year Follow-Up Study. Heart Surg Forum. 2012;15:E145-9.
- [CrossRef] [PubMed] [Google Scholar]
- Quadruple Valve Replacement for Rheumatic Valvular Disease. Excellent Durability for 20 Years. Herz. 2015;40:731-3.
- [CrossRef] [PubMed] [Google Scholar]
- Transcatheter Pulmonic Valve Replacement in Carcinoid Heart Disease. Eur Heart J Cardiovasc Imaging. 2015;16:1046.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple Organ Dysfunction After Mitral Valve Replacement in a Patient with Systemic Lupus Erythematosus Complicated by Libman-Sacks Endocarditis: A Case Report and Literature Review. J Int Med Res. 2023;51:1-8.
- [CrossRef] [PubMed] [Google Scholar]






