Translate this page into:
Extracorporeal Membrane Oxygenation Nursing Care
*Corresponding author: Varsha Sharma, Department of Nursing Care, All India Institute of Medical Sciences, New Delhi, India. varshasharma0591@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma V, Joshi M. Extracorporeal Membrane Oxygenation Nursing Care. J Card Crit Care TSS. 2024;8:129-33. doi: 10.25259/JCCC_18_2024
Abstract
Extracorporeal membrane oxygenation (ECMO) is increasingly being used with adult patients in respiratory failure or cardiac failure. ECMO is a complex treatment that requires diligent nursing care with the knowledge and ability to identify complications of ECMO can potentially reduce morbidity and mortality in these high-risk patients. Nurses are integral to the multidisciplinary team caring for patients in the intensive care unit and are fundamental to successful outcomes. The increased complexity of caring for the patient supported by ECMO adds to the challenge for the nursing team. The bedside intensive care nurse is supported by ECMO specialist nurses in the delivery of care and monitoring of the ECMO patient. This cardiopulmonary support system uses an artificial membrane lung to move blood forward and replace carbon dioxide with oxygen in venous blood.
Keywords
Cardiac failure
Cardiogenic shock
Extracorporeal membrane oxygenation
Respiratory failure
Nursing care for patients with extracorporeal membrane oxygenation
INTRODUCTION
Extracorporeal membrane oxygenation (ECMO) is being used with patients with cardiopulmonary failure or while the heart and lungs are in the recovery phase postoperatively or any complications related to the cardiopulmonary system or they are not able to function normally even with the assistance of all emergency medicines and ventilator. ECMO is a boon to modern critical cardiopulmonary care and to deal with complications, for example, during corona pandemic. While patient is on ECMO support needs vigilant care with a multidisciplinary approach, which includes (critical care physicians, surgeons, anesthetists, nurses, perfusionists, physiotherapists, and rehabilitation therapists). The approach of a multidisciplinary team is to provide good holistic ECMO care to the patient and early recovery of the patient. Early identification of complications with the help of expert team members and work in collaboration can reduce mortality and mortality in these high-risk patients. ECMO is not the treatment to cure the disease or complications related to the cardiopulmonary system; it’s a taking over the job of the heart and lungs during the recovery phase. Critical care nurses play a very important role while taking care of patients with ECMO. ECMO involves draining blood from the venous circulation to outside the body and passing it through the artificial lung membrane (oxygenator), which removes carbon dioxide and adds oxygen to the blood, which can be returned back to the body in venous or arterial circulation after re-warming.
INDICATIONS
Respiratory conditions in which ECMO support is indicated: Pneumonia, lung failure, pneumonia, acute respiratory distress syndrome, pulmonary embolism, as a treatment therapy during the corona virus pandemic, post-lung transplant
Conditions in which both cardiopulmonary support is needed: Cardiogenic shock, acute myocardial infarction, cardiomyopathies, myocarditis, cardiogenic shock, operation complications, for example, heart transplant
While cardiopulmonary resuscitation is carried out in that condition ECMO support is required.
ECMO COMPONENTS
The basic components of the ECMO circuit are as follows:
Venous and arterial cannulas
Blood pump
Oxygenator
Tubings
Monitors, alarms
Heat exchangers.
NURSING CONSIDERATIONS
Assessment and monitoring of the patient on ECMO patient
A competent healthcare team should identify the patient’s condition for the purpose of ECMO support and the disease process.
Continuous monitoring of the hemodynamic parameters of the patient’s health condition by various means, which includes heart rate and rhythm, blood pressure, pulmonary artery catheter monitoring, temperature, oxygen saturation, and oscillation of arterial waveform.
Prevention of hypothermia
Patients on ECMO support are more prone to hypothermia because blood is removed from the body. Heaters, fluid warmer, warm blankets (Bair–Hugger), and avoiding unnecessary exposure of the patient can be used for the maintenance of normothermia.
Providing routine care to the patient
Providing routine care to the patient is challenging as cannulas are in situ, and there is a risk of their dislodgement and bleeding because the patient is on anticoagulant therapy.[1]
Carefully changing the position of the patient while changing the sheets and providing routine care to the patient.
Use comfort devices and measures while providing a comfortable position to the patient, for example, a pillow.
Take help from the other healthcare team members.
Prevention of potential problems
Close observation of the surgical site and ECMO circuit for chances of bleeding, infection, any alarms from the monitor, for the dislodgement of cannulas, and kinking of the tubings. The health team should be ready for the management of all these potential problems by keeping all surgical and ECMO supplies for emergency purposes.
Muscle weakness is common in patients receiving ECMO support. When the patient is deemed ready for mobilization from a medical standpoint, physical therapy may begin.
Prevention of infection
Cannula in situ is a potential source of infection. The age of the patient and post-transplant (heart and lung transplant) are on immunosuppressive therapy, which are also contributing to increased chances of infection.
Close observation of the surgical site for the signs and symptoms of infection to the patient, for example, redness, inflammation, and bleeding that can be seen by doing transparent dressing at the cannula insertion site
Always maintain sterile technique and personal protective equipment while providing care to the patient and handling the invasive lines; it will reduce the chances of infection.
Hemodynamic parameters monitoring for identification of infection, for example, C-reactive protein.
Pain management
Pain management by various means by giving sedation will also reduce the oxygen consumption of the patient.[2] It will also reduce the patient’s movement and chances of cannula dislodgment. Other diversion techniques can also be used, for example, music and massage therapy, to the patient for better outcomes and to improve the intensive care unit experience of the patient.
Nutritional needs
Patients who are on ECMO therapy are at risk of malnutrition. Nutritional needs can be fulfilled by both enteral nutrition (EN) and parenteral nutrition (PN) routes.[3]
Some studies support that EN is safe and well-tolerated and can significantly reduce the in-hospital mortality of patients receiving ECMO. Abdominal distention and elevated gastric residual volume were the common reasons for EN intolerance, but occur less frequently in the early EN group.
For patients receiving ECMO, EN started with hypocaloric doses within 48 h of ECMO initiation is recommended.[4,5]
Fluid and electrolyte management
By monitoring renal function test, which is an important parameter in identifying fluid balance and the prognosis of the patient
Dialysis is indicated for the prevention and management of fluid overload. Dialysis can be done by various means, for example, hemodialysis and ECMO circuits [Figures 1 and 2].
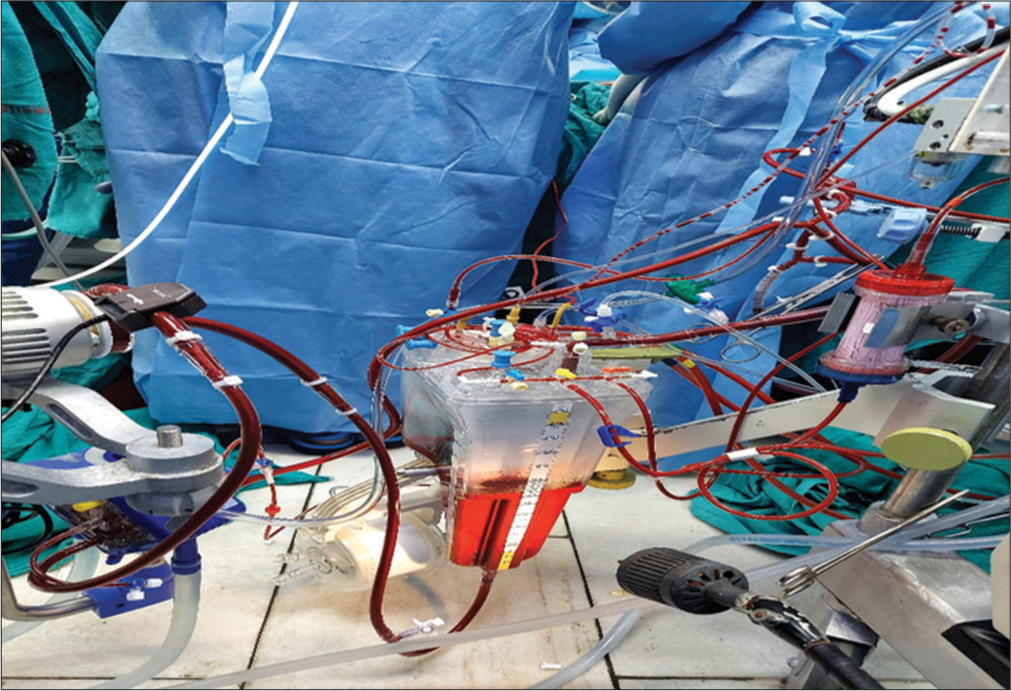
- Integrated extracorporeal membrane oxygenation.
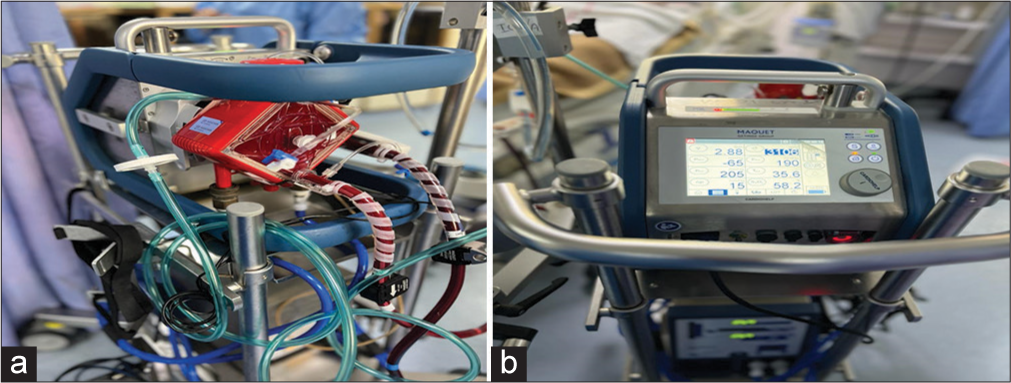
- (a and b) Cardiac extracorporeal membrane oxygenation.
Transportation
Reduced transportation is the priority for the patient as it will reduce the chances of cannula dislodgement and bleeding [Figure 3].
If it is needed, then all team members (critical care physician, nurse, perfusionist, and transport team members) should go along with the patient.
The team should be ready and well-equipped for the management of accidental cannula dislodgement if it occurs.
Routine diagnostic tests should be done at the bedside to reduce patient movement, for example, X-ray, ultrasound, and echocardiography. If computed tomography is indicated, proper transport measures should be taken while transporting the patient. Magnetic resonance imaging is contraindicated in patients on ECMO support due to the presence of metal content in cannulas.

- Transportation of patient on extracorporeal membrane oxygenation.
Psychological support to the patient and family
Nurses play a major role in providing care to the patient on ECMO support and communicating with the family members of the patient.[5] Clarifying the doubts of the patient and family members. Allowing the family members to express their anxiety and verbalize their feelings regarding the patient and disease process.
If attempts of weaning are unsuccessful then providing palliative care to the patient in collaboration with the ethical and legal department of the hospital for discontinuing ECMO support to the patient.
Complications: Muscle weakness, bleeding, coagulopathy, hemolysis, neurologic complications, limb ischemia, infection, and unsuccessful weaning.
ROLE OF NURSES IN DETECTING AND PREVENTION OF COMPLICATIONS RELATED TO ECMO
Specialized nurses have knowledge and understanding of potential complications related to ECMO therapy and can assist with early detection through critical thinking, performing frequent assessments, and reporting them through an open dialog with the team of providers involved.
Renal and other intra-abdominal complications
The incidence of acute kidney injury (AKI) has been reported as high as 80% of ECMO patients and is associated with a quadrupled mortality risk.[7] Severe fluid overload is one of the major reasons that renal replacement therapy (RRT) is initiated in this population and is often performed through the ECMO circuit but can also be performed after the pump, which could lower the risk of air embolism not trapped by the oxygenator.[8] Fluid overload is independently associated with increased mortality, prolonged loss of sensation, prolonged ventilator time, and prolonged ECMO time. This consideration can lead providers to assume earlier RRT for therapeutic fluid removal would reduce these comorbidities. The bedside nurse can assist in the early identification of AKI by monitoring urine output, measuring strict fluid intake and output, assessing serial serum chemistry values, particularly serum creatinine and trends of electrolyte dyscrasias, and identifying physical examination findings related to fluid overload.
Abdominal compartment syndrome (ACS)
This is one of the complications of the ECMO due to fluid overload. Keeping the ECMO flows appropriate prevents this complication. Positive fluid balance is associated with generalized edema, pleural effusions, and ascites, all of which are known to be causes of ACS. ACS can also compress femoral cannulas, thus diminishing the effectiveness of ECMO therapy.[9] Clinical assessments significant for the monitoring of ACS include physical monitoring of the abdomen for tension, distention (diameter), discoloration, and, if the technology is readily available, measurement of intra-abdominal pressure.
Hematological complications
Bleeding is the most frequent complication associated with ECMO. With the significant risk for bleeding and the subsequent need for anticoagulation, nurses can expect regular and repeated blood draws, transfusions, and anticoagulant titration to be a part of their daily practice in the care of the ECMO patient.
Infectious complications
Care provided by specialized nurses remains inherently important in the prevention of infection, particularly when caring for lines and their cannulation sites with thorough hand, cannulation site, and patient hygiene and the application of impermeable site dressings. For preventing infection preventive measures such as hand hygiene, meticulous oral care with chlorhexidine gluconate solution, endotracheal tube cuff pressure control, and control of sedation.[10] Further management of routine line and cannulation site management with sterile techniques.
Cardiopulmonary complications
The bedside nurse can assist with early detection of these complications by close assessment of vasopressor and inotrope requirements, endotracheal secretions, monitoring the ventilator for pressures, and ensuring daily chest radiographs and frequent echocardiograms which are ordered to monitor the progression of cardiopulmonary disease.[11-14]
Neurological complications
The bedside nurse becomes integral to monitoring subtle neurologic indicators such as pupillary response and bi-spectral index, which can read zero in the event of catastrophic neurologic injury.
Contraindications of ECMO
ECMO is contraindicated in the following clinical conditions:
Significant aortic regurgitation
Severe peripheral artery disease
Bleeding diathesis
Recent stroke or head trauma
Uncontrolled sepsis
Unwitnessed cardiac arrest
Malignancy.
CONCLUSION
Continuing assessment of nurses’ knowledge and practice, continuous training courses should be conducted for nurses to improve their knowledge and practice and to increase their performance regarding the care of patients with ECMO. High-fidelity medical simulation can play an important role in staff training, improvement in previously gained proficiency, and development of optimal SOP for nursing care and management during ECMO in patients with COVID-19. Optimal SOPs may further guide multidisciplinary teams, including intensive care units and interventional departments. Other healthcare professionals recognize continuous training, having experience, teamwork, and increased staffing as measures that can promote the nurses’ role in extracorporeal membrane oxygenation. Extracorporeal membrane oxygenation (ECMO) is increasingly being used with adult patients with respiratory failure or cardiac failure. ECMO is a complex treatment that requires diligent nursing care. Critical care nurses with the knowledge and ability to identify complications of ECMO can potentially reduce morbidity and mortality in these high-acuity patients.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Patient Care during ECMO In: Sangalli F, Patroniti N, Pesenti A, eds. ECMOExtracorporeal Life Support in Adults. New York: Springer Science and Business; 2014. p. :345-59.
- [CrossRef] [Google Scholar]
- Increased Sedation Requirements in Patients Receiving Extracorporeal Membrane Oxygenation for Respiratory and Cardiorespiratory Failure. Anaesth Intensive Care. 2012;40:648-55.
- [CrossRef] [PubMed] [Google Scholar]
- Adequacy of Nutrition Support During Extracorporeal Membrane Oxygenation. Clin Nutr. 2019;38:324-31.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) J Parenter Enter Nutr. 2016;40:159-211.
- [CrossRef] [PubMed] [Google Scholar]
- ESPEN practical and partially revised guideline: Clinical nutrition in the intensive care unit. Clinical Nutrition. 2023;42:1671-89.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care Professional Development for Critical Care Nurses: A Multicenter Program. Am J Crit Care. 2017;26:361-71.
- [CrossRef] [PubMed] [Google Scholar]
- Review of Extracorporeal Membrane Oxygenation and Dialysis-based Liver Support Devices for the Use of Nephrologists. Am J Nephrol. 2017;46:139-49.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal Membrane Oxygenation and the Kidney. Cardiorenal Med. 2016;6:50-60.
- [CrossRef] [PubMed] [Google Scholar]
- A Care Bundle Approach for Prevention of Ventilator-associated Pneumonia. Clin Microbiol Infect. 2012;19:363-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nurses' knowledge and practice regarding care of patients connected with extracorporeal membrane oxygenation. Eur Chem Bull. 2023;12:6374-86.
- [Google Scholar]
- Managing patients on extracorporeal membrane oxygenation support during the COVID-19 pandemic-a proposal for a nursing standard operating procedure. BMC Nurs. 2021;20:214.
- [CrossRef] [PubMed] [Google Scholar]
- Perception of other healthcare professionals about the nurses' role and competencies in veno-venous extracorporeal membrane oxygenation care: A qualitative study. Nurs Open. 2022;9:996-1004.
- [CrossRef] [PubMed] [Google Scholar]
- Extracorporeal membrane oxygenation: The nurse's role in patient care. Nursing Critical Care. 2020;15:6-14.
- [CrossRef] [Google Scholar]







