Translate this page into:
Optimizing Internal Mammary Artery Harvest and Preparation
*Corresponding author: Rahul Bhushan, Department of Cardiothoracic and Vascular Surgery, Atal Bihari Vajpayee Institiute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi, Delhi, India. rahulbhushan98@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhushan R, Grover V. Optimizing Internal Mammary Artery Harvest and Preparation: A Comprehensive Review of the Cornerstone in Coronary Revascularization. J Card Crit Care TSS. 2024;8:80-4. doi: 10.25259/JCCC_75_2023
Abstract
The left internal mammary artery (LIMA) graft plays a pivotal role in coronary artery bypass surgery, offering unparalleled efficacy in revascularization. This review paper delves into the multifaceted considerations surrounding LIMA utilization, aiming to provide a comprehensive understanding of optimal approaches. The study encompasses the alleviation of spasm, selection of graft harvesting techniques, identification of ideal vasodilators, and exploration of optimal delivery methods. Through an analysis of extensive research spanning the past three decades, this review elucidates critical insights for cardiac surgeons and researchers alike. The review emphasizes the ubiquity of severe spasms in harvested LIMA and examines interventions to mitigate this challenge. Studies highlighting the efficacy of papaverine administration through various routes underscore the need for tailored approaches based on clinical context. The debate between skeletonized and pedicled LIMA harvests is explored, revealing the advantages and complexities associated with each technique. Findings suggest that while skeletonized grafts offer enhanced flow, the decision remains multifaceted due to potential complications. Addressing the quest for the ideal vasodilator, the review juxtaposes papaverine and sodium nitroprusside, presenting both as viable options. Despite ongoing discussions, the cost-effectiveness and accessibility of papaverine have positioned it as the favored choice among clinicians. Optimal delivery methods emerge as a crucial factor in graft success, with perivascular injection showing promise in promoting sustained and improved flow rates. The clinical implications of these findings are substantial. By integrating the evidence presented, cardiac surgeons can make informed decisions, maximizing graft patency and patient outcomes. Further, research avenues are identified, encompassing refined delivery techniques, comprehensive comparisons of vasodilators, and long-term clinical outcome evaluations. In conclusion, this review underscores the intricate considerations essential for successful LIMA utilization. By addressing spasms, selecting graft techniques, choosing vasodilators, and refining delivery methods, practitioners can tailor their strategies to the individual patient, enhancing the efficacy of coronary revascularization.
Keywords
Left internal mammary artery
Coronary artery bypass surgery
Graft selection
Vasodilators
Spasm
Skeletonized harvest
Pedicled harvest
Papaverine
Sodium nitroprusside
Delivery methods
Coronary revascularization
Optimal approach
INTRODUCTION
The left internal mammary artery (LIMA) graft to the left anterior descending artery is undoubtedly a cornerstone of coronary artery bypass surgery and, to a significant extent, a pillar for cardiac surgeons, given its unparalleled efficacy compared to other grafts or catheter-based interventions.[1] However, a clear guideline and operative approach for optimizing LIMA performance are lacking. Given the vital nature of this topic, we believe that it is prudent to analyze research pertaining to LIMA and uncover an optimal approach to harvesting and preparing the LIMA before anastomosis. It is a well-known fact that the LIMA undergoes severe spasms immediately after harvesting, with or without the pedicle. The literature describes multiple topical dilators for treating spasms, including methods such as spraying, perivascular injection, or intraluminal injection of dilators into the LIMA to relieve spasms and enhance blood flow. Revisiting the literature to identify the most prudent harvesting and treatment protocol for the internal mammary artery (IMA) can aid readers and surgeons in adopting a more standardized and optimal approach during coronary revascularization procedures.
MATERIAL AND METHODS
This literature review was conducted using a search engine database of PubMed spanning the last 30 years. The search utilized MeSH keywords to ensure comprehensive coverage. Specifically, the following search terms were employed: “left internal mammary artery,” “internal thoracic artery,” “papaverine,” “topical dilators,” and “intravascular versus local injection.” Inclusion criteria for articles encompassed those that provided full-text availability [Figure 1]. Articles lacking full-text access were excluded from this study. The methodology adhered to the guidelines outlined by the Preferred Reporting Items of Systematic Reviews and Meta-Analyses, ensuring a systematic and structured approach to this review.
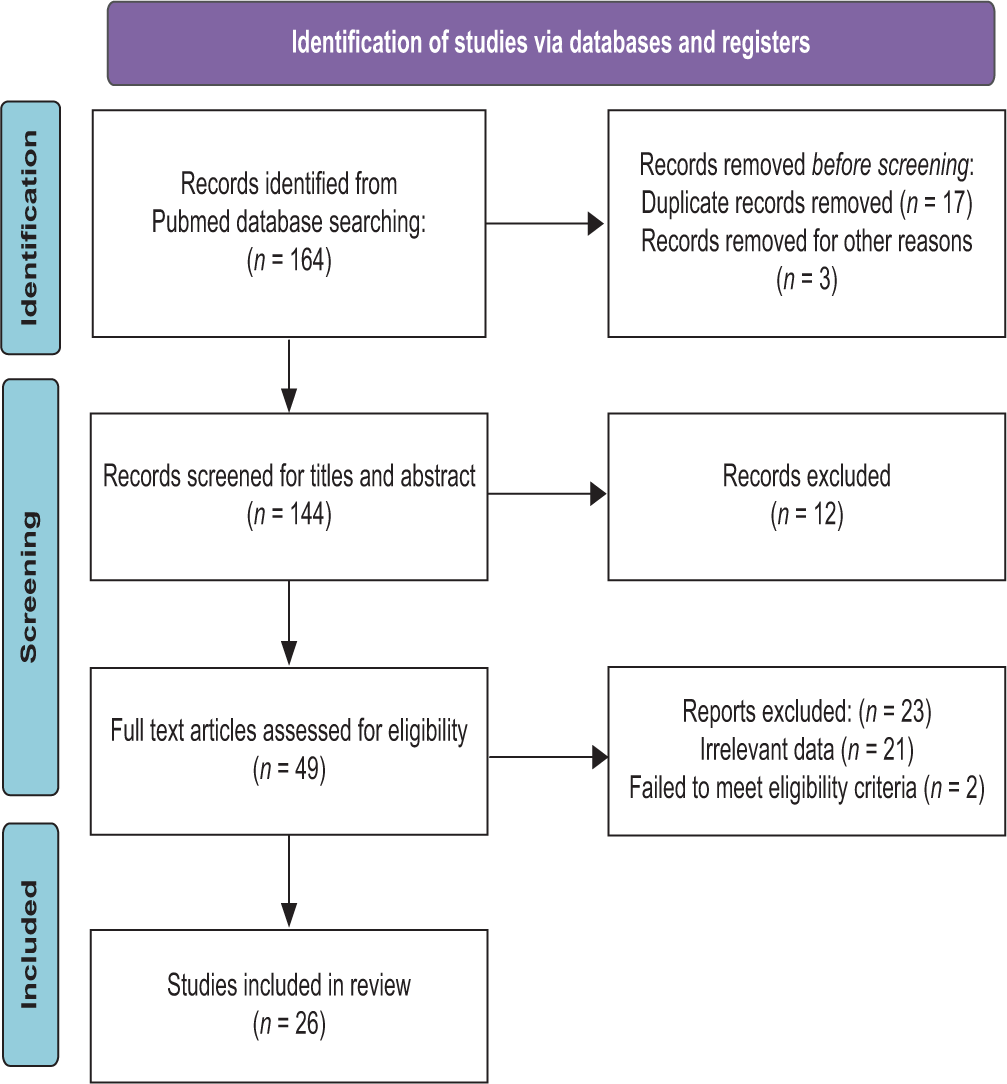
- Inclusion criteria for literature review.
RESULTS
LIMA and spasm
First, accepting the fact that every harvested LIMA undergoes severe spasm shall be a universal admission. A study by Yavuz et al. calculated that the mean blood flow in the LIMA was 60.7 ± 6.0 mL/min before papaverine application.[2] Post papaverine application in various subgroups, the mean blood flow in those receiving intraluminal papaverine rose to 129.3 mL/min, it was 87.7 mL/min in the subgroup of topical spray while 130.6 mL/min in those receiving periarterial papaverine on transit time flow measurement analysis. Francesco et al. evaluated LIMA topical free flow and intraluminal free flow measurements in a study of over 180 patients and found that standard untreated LIMA flow was roughly 31.6 ± 19.9 mL/min overall study subgroups which increased to 45.4 ± 38.9 mL/min in those treated with papaverine while it was 38.6 ± 25.2 among those treated by glycerylnitrate-verapamil offering statistically significant (P = 0.1) difference.[3]
Skeletonized versus pedicled IMA harvest
While obvious drawn advantages exist in favor of skeletonized LIMA harvest ranging from longer, lengthy, better skeletal supply to sternum, it is associated with increased time consumption and much more technical expertise in the harvest. In terms of flow measurement, a randomized trial by Puslecki et al. found no statistically significant difference between both subgroups of pedicled versus skeletonized IMA under evaluation in microscopic as well as inflammatory marker changes in both subgroups of IMA.[4]
However, another prospective study of 357 patients conducted by Deja et al, compared no skeletonized IMA with skeletonized ones and found that free left internal thoracic artery blood flow was 66.3 ± 7.42 mL/min in no skeletonized vessel versus 100.3 ± 14.84 mL/min in skeletonized (P = 0.04).[5] Furthermore, in a review analysis conducted by Erden et al., analyzing 17 papers providing the best clinical evidence summarized that graft patency was comparable in both the pedicled as well nonpedicled group, offering no statistically significant difference.[6] Thus, a skeletonized IMA shall be recommended but would not follow a strict dictum of protocol and shall be individualized based on patient and comorbidities as well as a surgeon.
The ideal vasodilator
In a comparative study by Cooper et al., the authors compared normal saline, papaverine, nifedipine, glyceryl trinitrate, and sodium nitroprusside (SNP) agents as treatment for IMA.[7] Free flow in each subgroup was measured. While saline produced a small increase in flow gain by 10 mL/min (from a median of 23 mL/min to 38 mL/min) (not significant), a significant increase was observed with papaverine, with a flow gain of 18 mL/min (from 25 mL/min to 43 mL/min). Nifedipine and glyceryl trinitrate raised free flow by 48 mL/min (from 23 mL/min to 71 mL/min) and 39 mL/min (from 23 to 62 mL/min), respectively. SNP, on the other hand, increased inflow by 82 mL/min (from 26 to 108 mL/min). Thus, they recommended the use of SNP as an ideal dilator. SNP, being a potent vasodilator, releases Nitric oxide, and induces hypotension in high dosage. With a half-life of only 2 min, it is commonly used to treat hypertensive crises with typical infusion rates ranging from 0.5 to 4 mcg/kg/min, which is then titrated to the desired effect. Typical infusion concentrations for adults are 200 mcg/mL or 400 mcg/mL. Thus, for local administration in IMA harvest, it is considered safe in regulated doses under the anesthetic’s guidance. In a randomized trial conducted by Francesco et al., 100 patients were randomly divided into three subgroups of glyceryl-trinitrate/verapamil (GV) solution group, papaverine group, and normal saline group where dilators were administered intraluminal and flow rates were studied.[3] While the papaverine subgroup had maximal flow, it did not reach statistical significance when compared to the GV subgroup. However, intraluminal free flow in group GV and papaverine subgroup was higher than the normal saline group (P = 0.004 and 0.001, respectively).
A randomized trial to explore ideal vasodilator was conducted by Battaloglu, et al. comparing four vasodilators, namely, nitro-glycerine, diltiazem, papaverine, and adenosine.[8] They found no significant differences among the five groups’ pre-treatment flow rates (P = 0.526) or post-treatment flow rates (P =.194). The mean ratio values were 1.74 ± 0.17 with nitro-glycerine, 1.77 ± 0.49 with diltiazem, 1.82 ± 0.59 with papaverine, and 1.57 ± 0.54 with adenosine. Thus, no ideal vasodilator exists. While few studies point to SNP as an ideal agent, most of the studies hail papaverine as the single most common drug to be used as a dilator based on cost, availability, and robust data support.
Intraluminal, topical spray, or injection to adjacent tissue-the ideal delivery
Gowda et al. studied papaverine delivery through topical spray and perivascular injection into LIMA pedicle in forty randomized undergoing coronary revascularizations.[9] In analyzing data, they found that LIMA flows were identical in both groups before the papaverine application. However, LIMA blood flow after papaverine application in the topically sprayed group was 87.20 ± 13.46 mL/min, while it was 104.7 ± 20.19 mL/min in those who received a perivascular injection of papaverine to LIMA pedicle. It was hypothesized that the perivascular injection of papaverine exposed IMA to prolonged duration to dilator in comparison to spraying. A study conducted by Yorgancioğlu et al. involving 86 patients was divided into two subgroups – one receiving SNP spray while the other subgroup was given perivascular injection of SNP.[10] Statistically significant differences were noted in flow measurement (P < 0.05) between the two groups, where SNP injection to the pedicle provided a better flow than simple spraying of the same agent. In a similar trial conducted by Dregelid, et al., involving 78 patients undergoing coronary revascularization, intraluminal papaverine solution injection provided a better blood flow rate and distal dilation than mere submersion in papaverine solution but at a considerable risk of mechanical wall injury which was reported in 8 of 52 internal mammary arteries treated with intraluminal papaverine.[11]
An interesting comparative study was conducted by Bahcivan et al. randomizing 75 patients into three subgroups, namely, group 1 had papaverine injected into the endo thoracic tissue around the internal thoracic artery before dissection, group 2 had papaverine injected into IMA pedicle, and group 3 had intraluminal papaverine injected.[12] Mean blood flow was 56.3, 21.1, and 20.9 mL/min in groups 1, 2, and 3, respectively. Thus, they proposed that papaverine injected into endo thoracic fascia not only facilitated rapid harvesting by creating a plane of dissection, but it also gave better flow to LIMA. However, the said practice was associated with more episodes of bleeding in multiple studies due to dilatation of IMA branch vessels as well and thus not routinely recommended. Considering the research, perivascular papaverine injection is recommended for optimal and prolonged topical action of vasodilators. While intraluminal injection occasionally yields better results, the associated risk discourages its regular use.[13-16]
In a recent RCT published by Rezk et al., the authors randomized 100 patients into intrapleural LIMA harvest versus extrapleural IMA harvest to follow up for variation in outcomes in two groups. The study mainly found lesser respiratory complications with better improvement in forced expiratory volume in the first and second sec (FEV1%), forced vital capacity (FVC%), and FEV1/FVC in the extrapleural approach.[17]
DISCUSSION
The LIMA graft holds a pivotal role in coronary artery bypass surgery, standing as a cornerstone of effective revascularization.[18,19] In this review, we delved into the intricate aspects of LIMA utilization, focusing on spasm alleviation, graft selection methods, ideal vasodilators, and optimal delivery techniques. The analysis of the accumulated data sheds light on several critical considerations for cardiac surgeons and researchers alike. Our exploration confirms the universal occurrence of severe spasms in harvested LIMA, which necessitates effective interventions.[20] Intraluminal, topical spray, and periarterial routes of papaverine administration exhibited varying degrees of success in alleviating spasms and enhancing blood flow. This underscores the importance of selecting the most effective method based on clinical context and individual patient factors. The debate surrounding skeletonized versus pedicled LIMA harvest persists. While skeletonized grafts offer advantages in terms of sternum supply and length, our review shows that the decision should not be taken lightly.[21] Striking a balance between enhanced flow and potential complications inherent to the technique remains an ongoing challenge. Our review highlights papaverine as a commonly recommended choice, demonstrated to yield significant flow improvements across studies. Papaverine is the hydrochloride of an alkaloid obtained from opium or prepared synthetically. It belongs to the benzylisoquinoline group of alkaloids. Papaverine relaxes the smooth musculature of the larger blood vessels, including the coronary, cerebral, peripheral, and pulmonary arteries. Considered to be a safe drug with minimal systemic impact, the documented complications include dizziness, vertigo, and priapism. Although consensus remains elusive, the practicality, cost-effectiveness, and availability of papaverine have positioned it as the preferred option for most clinicians.[22]
The route of vasodilator delivery plays a crucial role in optimizing graft flow. Our analysis reveals a compelling preference for perivascular injection over other methods. Studies suggest that perivascular injection of papaverine leads to prolonged exposure and subsequently improved flow rates in the LIMA.[23,24] This aligns with Yorgancioğlu et al.’s findings, demonstrating better outcomes with perivascular injection of SNP compared to topical spraying.[10] Despite the advantages, the potential for mechanical wall injury with intraluminal injection raises concerns, warranting careful consideration.
The insights derived from this review hold substantial clinical implications. Adopting a judicious approach to LIMA utilization, spasm management, and vasodilator selection could contribute to improved patient outcomes and graft patency. Further, the research could explore refined delivery techniques, a comprehensive comparison of vasodilators, and advancements in minimizing potential risks associated with different approaches. In addition, prospective studies evaluating long-term clinical outcomes would contribute to a more comprehensive understanding of the best practices in LIMA utilization.[25,26]
CONCLUSION
The LIMA graft stands as a cornerstone of coronary artery bypass surgery, with its optimal utilization requiring a nuanced understanding of various factors. This review underscores the importance of addressing LIMA spasms, selecting the appropriate graft harvest technique, and choosing the most effective vasodilator and delivery method. By amalgamating the evidence presented, cardiac surgeons can make informed decisions, tailoring their approach to the individual patient’s needs and achieving the best possible outcomes in coronary revascularization.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Internal Mammary Harvesting: Techniques and Evidence from the Literature. J Card Surg. 2020;35:860-7.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Papaverine Applications on Blood Flow of the Internal Mammary Artery. Ann Thorac Cardiovasc Surg. 2001;7:84-8.
- [Google Scholar]
- Effects of Papaverine and Glyceryl Nitrate-verapamil Solution as Topical and Intraluminal Vasodilators for Internal Thoracic Artery. Ann Thorac Surg. 2006;81:120-4.
- [CrossRef] [PubMed] [Google Scholar]
- An Innovative Panel to Assess Endothelial Integrity of Pedicled and Skeletonized Internal Thoracic Artery used as Aortocoronary Bypass Graft: A Randomized Comparative Histologic and Immunohistochemical Study. J Thorac Dis. 2018;10:4865-73.
- [CrossRef] [PubMed] [Google Scholar]
- Intraoperative and Laboratory Evaluation of Skeletonized Versus Pedicled Internal Thoracic Artery. Ann Thorac Surg. 1999;68:2164-8.
- [CrossRef] [PubMed] [Google Scholar]
- Does a Skeletonized or Pedicled Left Internal Thoracic Artery give the Best Graft Patency? Interact Cardiovasc Thorac Surg. 2010;10:97-104.
- [CrossRef] [PubMed] [Google Scholar]
- Overcoming Perioperative Spasm of the Internal Mammary Artery: Which is the Best Vasodilator? J Thorac Cardiovasc Surg. 1992;104:465-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of Pretreatment with Different Topical Vasodilators on Blood Flow in the Internal Mammary Artery: A Prospective Randomized Study. Heart Surg Forum. 2007;10:E136-40.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Papaverine on Left Internal Mammary Artery Flow: Topical Spraying Versus Perivascular Injection Method. Braz J Cardiovasc Surg. 2020;35:181-4.
- [CrossRef] [PubMed] [Google Scholar]
- An Alternative Application of Sodium Nitroprusside to Overcome Perioperative Spasm of the Internal Thoracic Artery. Cardiovasc Surg. 2001;9:64-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dilation of the Internal Mammary Artery by External and Intraluminal Papaverine Application. J Thorac Cardiovasc Surg. 1995;110:697-703.
- [CrossRef] [PubMed] [Google Scholar]
- Endothoracic Papaverine Application for Internal Thoracic Artery Harvest. Asian Cardiovasc Thorac Ann. 2007;15:234-7.
- [CrossRef] [PubMed] [Google Scholar]
- All We Need to know about Internal Thoracic Artery Harvesting and Preparation for Myocardial Revascularization: A Systematic Review. J Cardiothorac Surg. 2021;16:354.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Normothermic Papaverine to Relieve Intraoperative Spasm of the Internal Thoracic Artery. Ann Thorac Surg. 1996;62:769-71.
- [CrossRef] [PubMed] [Google Scholar]
- Arterial Endothelial Denudation by Intraluminal Use of Papaverine-NaCl Solution in Coronary Bypass Surgery. Eur J Cardiothorac Surg. 2004;25:560-6.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative Estimation of LIMA Blood Flow between Extraluminal Papaverine vs Extraluminal Papaverine Plus Intraluminal Vasodilator Cocktail in CABG Patients. Ann Card Anaesth. 2020;23:414-8.
- [CrossRef] [PubMed] [Google Scholar]
- Open Versus Closed Pleura Internal Mammary Artery Harvesting and Early Pulmonary Function After Coronary Artery Bypass Grafting. Heart Lung Circ. 2020;29:1412-7.
- [CrossRef] [PubMed] [Google Scholar]
- In Patients Undergoing Coronary Artery Bypass Grafting is Semi-skeletonization Superior to Pedicled Harvesting of the Left Internal Mammary Artery? Interact Cardiovasc Thorac Surg. 2021;33:362-6.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletonized or Pedicled Harvesting of Left Internal Mammary Artery: A Systematic Review and Meta-analysis. Semin Thorac Cardiovasc Surg. 2021;33:10-8.
- [CrossRef] [PubMed] [Google Scholar]
- 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:197-215.
- [CrossRef] [PubMed] [Google Scholar]
- Intractable Left Internal Mammary Artery Spasm After Coronary Artery Bypass Grafting. Cureus. 2020;12:e7045.
- [CrossRef] [Google Scholar]
- Differential Pharmacologic Sensitivities of Phosphodiesterase-3 Inhibitors among Human Isolated Gastroepiploic, Internal Mammary, and Radial Arteries. Anaesth Analg. 2005;101:950-6.
- [CrossRef] [PubMed] [Google Scholar]
- A Comparative Evaluation of the Effects of Multiple Vasodilators on Human Internal Mammary Artery. Anaesthesiology. 1998;88:1654-9.
- [CrossRef] [PubMed] [Google Scholar]
- Harvesting Internal Mammary Artery: A Narrative Review. J Cardiovasc Surg (Torino). 2020;61:790-801.
- [CrossRef] [PubMed] [Google Scholar]
- In Situ Skeletonized Right Internal Mammary Artery Bypass Grafting to Left Anterior Descending Artery. Int Heart J. 2018;59:35-42.
- [CrossRef] [Google Scholar]
- Techniques and Standards in Intraoperative Graft Verification by Transit Time Flow Measurement After Coronary Artery Bypass Graft Surgery: A Critical Review. Eur J Cardiothorac Surg. 2017;51:26-33.
- [CrossRef] [PubMed] [Google Scholar]






