Translate this page into:
Tubercular Tenosynovitis of the Wrist and Cardiac Correlation
*Corresponding author: Pranav Kapoor, Junior Resident, Department of Orthopaedics, Sharda University, Noida, Uttar Pradesh, India. kapoor.pranav193@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kapoor P, Singh A, Sood A. Tubercular Tenosynovitis of the Wrist and Cardiac Correlation. J Card Crit Care TSS 2023;7:165-8.
Abstract
Tubercular tenosynovitis has also been known as compound palmar ganglion which is a misnomer. Cardiovascular complications of tuberculosis (TB) are one of the most common extrapulmonary involvements of the disease. These cardiac complications arising due to tubercular inflammation are many and varies. These range from pericarditis (high prevalence) to acute myocardial infarction, aortitis, myocarditis, and mycotic aneurysms and many others. Cardiovascular complications of TB have a high rate of morbidity and mortality rate. There should be a high index of suspicion and interdisciplinary involvement of the various required specialties in the management of such a swelling with cardiac pathophysiology as well. This case report highlights one such example of tuberculosis with acute myocardial infarction (AMI) which got unmasked post TTS surgery.
Keywords
Tubercular tenosynovitis
Wrist
Cardiac correlation
INTRODUCTION
Tubercular tenosynovitis (TTS) has also been known as compound palmar ganglion in the past. Its differential diagnosis includes a vast number of inflammatory and infective pathologies of the hand, making diagnosis difficult. Large painless progressive swelling in the wrist or hand, with a restricted range of movement and weak grip in tuberculosis (TB) endemic areas must raise the suspicion of being of tubercular etiology. Laboratory tests and other investigative tools are useful diagnostic aids but are non-specific. The ultimate diagnosis is by histopathology examination (HPE) or detection of Mycobacterium tuberculosis in microbiological tests.[1,2] Suspicious cases must undergo excision biopsy, debridement with tenosynovectomy, with antitubercular therapy (ATT) to provide favorable outcomes.
TB is caused by the micro-organism M. tuberculosis, an airborne infectious agent that can rapidly spread from person to person during its active phase.[3] As the disease progresses, it can spread to involve multiple organ systems, such as the lymphatic system, central nervous system, gastrointestinal (peritoneum commonly), and cardiovascular system (CVS), among others.[4] As far back as the early 1900s, many authors in the literature had noted the effects of TB on the CVS even now, in the modern era, mortality rates of those with CVS involvement approach 60%.[5,6] Globally, cardiovascular diseases are the leading cause of death; thus, intersections of TB and CVS, especially with such high mortality rates, should be closely examined.[7] Cardiovascular complications of TB are one of the most common extrapulmonary involvements of the disease. These CVS complications arising from TB are numerous, with pericarditis showing a high prevalence. Others are acute myocardial infarction (AMI), aortitis, myocarditis, and mycotic aneurysms.[8,9] We present here, one such patient who incidentally had tubercular and cardiac manifestations.
CASE REPORT
A 48-year-old female presented with painless progressive swelling on the left wrist for 7 months. Examination revealed two swellings approximately 7 cm × 5 cm, respectively, on the ulna-volar aspect of the wrist on either side of the carpal ligament [Figure 1].

- (a-c) Two palmar swellings approximately 7 cm × 5 cm on either side of the carpal ligament seen in different cross section.
Magnetic resonance imaging (MRI) revealed a lobulated lesion extending from the distal forearm into the palmar hypothenar aspect of the hand engulfing the flexor tendons in a dumbbell fashion [Figure 2]. The patient complained of intermittent chest pain radiating to the back, on exertion. Echocardiography revealed a 99% stenotic and blocked right coronary artery (RCA) with ischemic changes in the electrocardiogram inferolateral leads with an ejection fraction of 55%. She was, thus, posted for 2 elective procedures 1 week apart [Figure 3]. In the first, surgical excision of the two swellings on the left wrist and the second procedure after 1 week was an angioplasty with a high-risk percutaneous coronary intervention (PCI) done, in the RCA with a drug eluting stent. Both the procedures were uneventful. She was then put on antitubercular and antiplatelet drugs postoperatively.
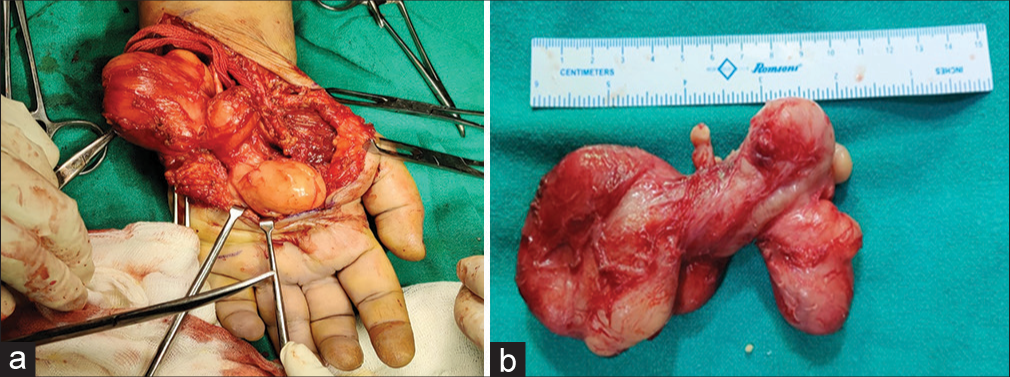
- Surgical excision of the compound palmar ganglion. (a) With gross section and (b) it is the excised encapsulated mass.
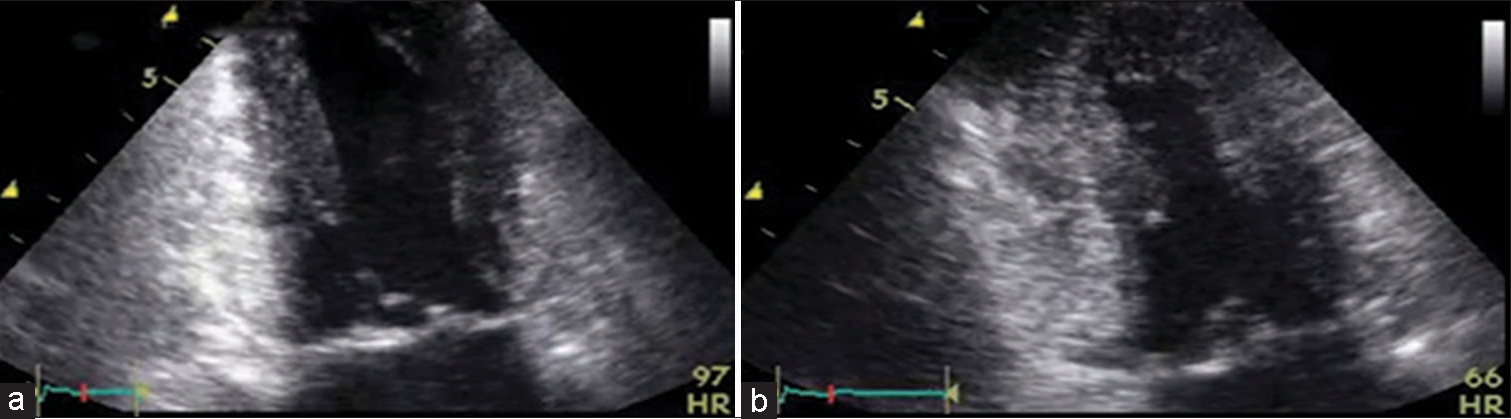
- (a and b) A transthoracic echocardiogram showing decreased wall motion in midseptum and inferior lateral wall dyskinesia following acute myocardial infarction with tuberculosis.
Intraoperative, a large encapsulated mass arising from the ulnar bursa proximal to the carpal ligament and intraoperatively extending distally to encompass the tendon sheaths of the ring, and little fingers were excised. On histopathological examination (HPE), a grossly cut section revealed an irregularly thickened wall of the cyst cavity filled with yellowish material indicative of rice bodies and microscopically suggestive of a large ganglion cyst. GeneXpert M. tuberculosis/resistance to rifampin assay on tissue samples was positive for M. tuberculosis. The patient was started on ATT (4 drug regime), hand splinted with posterior slab, and supervised physiotherapy started once the patient was pain-free. At 3-month follow-up, the patient had full functional recovery with good grip strength and range of motion with repeat echocardiography showing good ventricle function with the left ventricular ejection fraction of 55%. High risk PCI was done one week later, which too was uneventful.
DISCUSSION
TTS represents only 2–5% of osteoarticular TB. TTS progresses through three histopathological stages which are: (i) hygromatous, (ii) serofibrinous, and (iii) fungoid stage. The progression of the disease is slow and local inflammatory signs are usually discreet or absent. MRI is more sensitive and specific than ultrasound for detecting and visualization of tubercular synovial tendon sheaths. The ultimate diagnosis is by HPE and microbiological tests.[10] HPE findings usually reveal granulomatous lesions showing central caseation and surrounded by multiple giant cells and epithelioid cells confirming TB.[11] Rice bodies found in TTS consist of fibrinous masses (tubercles) and are formed due to microinfarction following inflammation and ischemia of the synovial sheath and are present in 50% of cases. When the diagnosis is uncertain and tissue cultures are pending or delayed, crucial time is lost which may delay diagnosis and treatment. Hence with a provisional diagnosis of TB, ATT can be started empirically. TB and coronary heart disease (CHD) have a common pathophysiology of inflammation. The pathogenesis of atherosclerosis of tubercular and CHD etiology thus is a systemic inflammation that plays a significant role in the development of CHD. Furthermore, TB and CHD have been said to have epidemiologic similarities. From a pathological perspective, systemic inflammation plays a significant role in the development of CHD in TB, and this inflammation propels immunological activation, which drives the development of CHD. Furthermore, the coinfection of HIV with TB, commonly seen in low and middle-income countries, further contributes to this immunological response leading to worse outcomes in patients.[12,13] Huaman et al. conducted a randomized controlled case study investigating the relationship between latent TB and AMI. This study in which 105 patients with AMI and 110 non-AMI controls were enrolled showed a higher frequency of latent TB in AMI patients compared to non-AMI controls.
Correlating coronary heart disease (CHD) and TB in our patient
Our patient having simultaneous coronary artery disease with TTS is not a coincidence. The epicenter of the pathophysiology of both acute myocardial infarction and tubercular tenosynovitis both preoperatively and postoperatively remains inflammation. An orthopaedic surgery here unmasked the coronary symptom and she was well referred to the cardiologist. Right coronary artery (RCA) stenosis with AMI in women presents generally with atypical chest pain, back pain, and gastroenteritis. Our patient had the same symptoms. Hence, the second cath lab-based high-risk percutaneous coronary implantation (PCI) was done with a drug-eluting stent in the RCA territory. It was done under sedation and the procedure remained uneventful. As a corollary to this case study, echocardiography should be done in all tubercular patients.
What’s new in 2023?
Today in 2023, an MRI of the cyst with gangliography may be performed to delineate the boundary, type, position, and homogenous nature of the compound palmar ganglion and differentiate it from a plain giant cyst, lipoma, neuroma, or a sarcoma cyst. Echocardiography backup is noninvasive and should be done when a typical chest pain symptom persists.
CONCLUSION
Cardiovascular complications of TB have a high rate of morbidity and mortality. There should be a high index of suspicion and interdisciplinary involvement of the various required specialties in the management of such a swelling with a cardiac pathophysiology backup as well.[14] Patients who are successfully treated for active TB should continue to be monitored for long-term cardiovascular complications with frequent echocardiography performed at regular intervals. Furthermore, more studies should be conducted on the various cardiovascular complications in TB to improve management guidelines for affected patients and further reduce mortality.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Financial support and sponsorship
Nil.
References
- Compound Palmar Ganglion: A Case Report and Literature Review. Ann Saudi Med. 1986;6:55-9.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis Tenosynovitis with Multiple Rice Bodies of the Flexor Tendons in the Wrist: A Case Report. Int J Surg Case Rep. 2016;27:129-32.
- [CrossRef] [PubMed] [Google Scholar]
- Extrapulmonary Tuberculosis: Pathophysiology and Imaging Findings. Radiographics. 2019;39:2023-37.
- [CrossRef] [PubMed] [Google Scholar]
- Extra-Pulmonary Tuberculosis: A Retrospective Study of Patients in Accra, Ghana. PLoS One. 2019;14:e0209650.
- [CrossRef] [PubMed] [Google Scholar]
- Trend Analysis of Cardiovascular Disease Mortality, Incidence, and Mortality-to-Incidence Ratio: Results from Global Burden of Disease Study 2017. BMC Public Health. 2021;21:401.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis and Risk of Acute Myocardial Infarction: A Propensity Score-Matched Analysis. Epidemiol Infect. 2017;145:1363-7.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculous Tenosynovitis of the Flexor Tendons of the Wrist: A Case Report. BMC Res Notes. 2018;11:238.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis of the Skeletal System: Bone, Joints, Spine, and Bursal Sheaths (3rd ed). New Delhi: Jaypee Brothers Medical Publishers; 2004.
- [Google Scholar]
- Heart Disease and Stroke Statistics--2011 Update: A Report from the American Heart Association. Circulation. 2011;123:e18-209.
- [Google Scholar]
- The Relationship between Latent Tuberculosis Infection and Acute Myocardial Infarction. Clin Infect Dis. 2018;66:886-92.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis and Cardiovascular Complications: An Overview. Cureus. 2022;14:e28268.
- [CrossRef] [Google Scholar]






