Translate this page into:
Total Anomalous Pulmonary Venous Connection with Right Pulmonary Artery Stenosis
*Corresponding author: V. Bharath, Department of Cardiothoracic and Vascular Surgery, All India Institute of Medical Sciences, New Delhi, India. drbharathaiims@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bharath V, Hote MP. Total Anomalous Pulmonary Venous Connection with Right Pulmonary Artery Stenosis. J Card Crit Care TSS. 2025;9:71-4. doi: 10.25259/JCCC_39_2024
Abstract
Total anomalous pulmonary venous connection (TAPVC) is a cyanotic congenital anomaly where all 4 pulmonary veins open into the right atrium directly or indirectly, instead of opening into the left atrium. Patients with this condition present in neonatal and infancy period with symptoms of breathing difficulty, rapid breathing, and bluish coloration. The association of TAPVC with branch pulmonary artery stenosis is a rare condition and is not described in literature.
Keywords
Branch pulmonary artery stenosis
Right pulmonary artery stenosis
Total anomalous pulmonary venous connection
INTRODUCTION
Total anomalous pulmonary venous connection (TAPVC) accompanied by right pulmonary artery (RPA) Stenosis is an uncommon congenital heart anomaly marked by an abnormality in pulmonary venous return. In this condition, the pulmonary veins do not connect appropriately to the left atrium; instead, they drain into the systemic venous system, resulting in a mixture of oxygen-poor and oxygen-rich blood. The presence of RPA stenosis, which refers to the narrowing of the right pulmonary artery, exacerbates the situation by limiting blood flow from the right lung and elevating pressure within the pulmonary circulation. This combination can lead to severe cyanosis, pulmonary hypertension, and heart failure. Surgical intervention to correct both TAPVC and RPA stenosis is generally required, often during infancy. Timely diagnosis and treatment are essential for enhancing patient outcomes.
SURGICAL TECHNIQUE
We present a 2-year-old male child weighing 10 kg who presented to our pediatric emergency with deep cyanosis. On evaluation, the child was diagnosed with TAPVC with suspected narrowing of the RPA on echocardiography which also showed enlarged right atrium (RA) and ventricle. The RA and right ventricle were enlarged and the RPA was stenosed and not widened. Computed tomography angiography done confirmed the echocardiography findings.
After taking informed consent from the parents, the child was taken up for surgery. The child was intubated and invasive monitoring lines were placed. After sternotomy, the pericardium was opened and external anatomy of the heart was visualized. RPA was dissected and was found small in caliber compared to the left pulmonary artery [Figure 1].
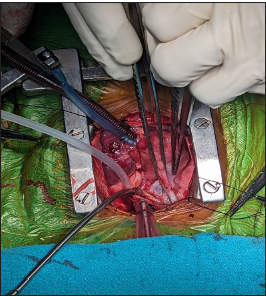
- External anatomy of the heart showing small right pulmonary artery.
After heparinization, cardiopulmonary bypass (CPB) was initiated with aortic and bicaval cannulation. Superior vena cava (SVC) was dissected and common chamber (formed by the confluence of all 4 pulmonary veins [PVs]) was identified posterior to the left atrium (LA) [Figures 2-4].
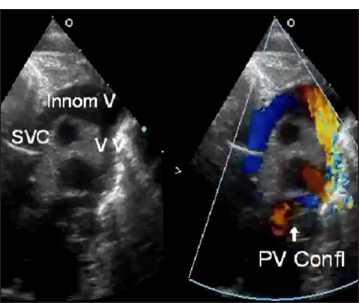
- Transthoracic echocardiography of the supracardiac total anomalous pulmonary venous connection showing the superior vena cava and innominate vein with confluent pulmonary valve. PV: Pulmonary vein, SVC: Superior vena cava
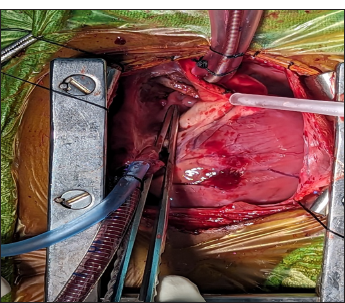
- Common chamber formed by the confluence of all four pulmonary veins was seen posterior to the left atrium.
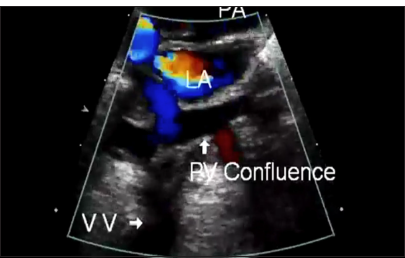
- Trans-thoracic echocardiography of intracardiac total anomalous pulmonary venous connection: Pulmonary venous confluence, seen posterior to the left atrium. PV: Pulmonary vein, LA: Left atrium, PA: Pulmonary artery
Systemic cooling started, the aorta cross-clamped, and cold blood cardioplegia was administered in the aortic root. Heart arrested in diastole.
RA opened and small atrial septal defect (ASD) was visualized. Common chamber anastomosed with the LA. ASD closed with dacron patch. RA closed, rewarming started, heart desired, and aortic cross-clamp released. Cardiac activity resumed. Enlargement of the LA was not performed.
Autologous pericardium harvested. RPA opened longitudinally and augmented with autologous pericardium. CPB gradually weaned off. RPA was now found to be adequately filling.
The sternum closed and the child was shifted to intensive care unit with mechanical ventilation and inotropes. Weaning from ventilator started on post-operative day (POD) 1. On POD 2, the child developed a patch in the right lung. Repeated attempts at weaning were unsuccessful. Hence, tracheostomy was done on POD 10. The child developed sepsis and expired on POD 20.
DISCUSSION
TAPVC is cyanotic congenital cardiac anomaly where all 4 PV will open into RA instead of LA, directly or indirectly.[1] Its surgical correction involves anastomosing common chamber to LA and closing the ASD.[2,3] TAPVC with branch pulmonary artery (PA) stenosis is not described in literature.
Yan et al., in a case report concluded that severe pulmonary artery hypertension (PAH) develops in infancy in the majority of patients with TAPVC. Only surgical intervention can save patients’ lives, and whether they have pulmonary venous return, obstruction has a significant impact on their prognosis. The timing and prognosis of surgery depend on the level of pulmonary hypertension, so it is crucial to assess patients’ PAH.[4]
Supracardiac TAPVC, surgical intervention typically consists of lifting the heart to the right and constructing a side-to-side anastomosis between the pulmonary venous confluence and the LA. Hasan et al. in a study stated that a second procedure was executed to minimize stress on the anastomosis as there was an obstruction in the confluence. This involved performing end-to-side anastomosis of the vertical vein to the left atrial appendage.[5]
Yen Hu concluded that a small PV confluence width is associated with the development of post-operative PVS and recurrent stenosis after surgical relief of PVS. Their results suggest that adequate bilateral PV lateralization during TAPVC surgery is crucial.[6]
In our case, we corrected TAPVC with surgical repair and addressed RPA stenosis by augmenting it with autologous pericardium. Augmenting pulmonary stenosis with pericardium is a standard technique routinely done in tetralogy of fallot repair,[7] but not in TAPVC RPA stenosis, which is a rarity.
Post-operative complications in the form of PV stenosis can occur after surgical repair of TAPVC. PV stenosis is a complication that can occur in up to 21% of patients who undergo repair of TAPVC.
Other complications that can occur after TAPVC repair include: Post-operative PV obstruction: This complication can occur in up to 14.8% of patients who undergo TAPVC repair. Hemodynamically significant left to right shunting: This can occur if the vertical vein is left unligated. Risk factors for death after TAPVC repair include earlier age at surgery, hypoplastic or stenotic PVs, associated complex cardiac lesions, and postoperative pulmonary hypertension. Effective management of PV stenosis requires an interdisciplinary team and multimodal therapy. This can include medical and transcatheter therapies, as well as surgical repair.[8]
Partial anomalous pulmonary venous connection (PAPVC) is associated with ASD in most of the cases. However, in the case of ventricular septal defect (VSD) with the right ventricular volume overload and turbulent flow in SVC, associated PAPVC should be considered and treated accordingly. Proper diagnosis in the initial setting can allow to prevent redo procedures in these pediatric patients. In cases of VSD, the echocardiologist might not look for PAPVC. PAPVC on the right side is more common, but we report a case of LSPV draining into the left brachiocephalic with an upper muscular VSD.[9]
The potential benefits of this modification of the trapdoor technique are excellent operative exposure, use of autogenous, viable tissue capable of further growth, achievement of the anastomosis with correct angling and length, avoidance of injury to the aortic and pulmonary valvular apparatus, and avoidance of obstruction within the right ventricular outflow tract. In addition, the resulting absence of tension, torsion, or traction and the use of viable, endothelialized, autogenous arterial flaps help to avoid thrombosis.[10]
Pre-operative identification of TAPVR with double drainage has important surgical implications. Failure to address both the drainage of TAPVR may result in residual left-to-right shunting that requires further intervention and increases morbidity and mortality.[11]
CONCLUSION
TAPVC with RPA stenosis is a rare clinical entity. Its treatment is quite straightforward involving surgical correction of TAPVC along with RPA augmentation with autologous pericardium.
Ethical approval:
Institutional review board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- Total Anomalous Pulmonary Venous Connection: Morphology and Outcome from an International Population-based Study. Circulation. 2010;122:2718-26.
- [CrossRef] [PubMed] [Google Scholar]
- Total Anomalous Pulmonary Venous Connection: The Current Management Strategies in a Pediatric Cohort of 768 Patients. Circulation. 2017;135:48-58.
- [CrossRef] [PubMed] [Google Scholar]
- A Single Center, Retrospective Analysis of Total Anomalous Pulmonary Venous Connection Repair Early Outcome at a Tertiary Care Center in India. Ann Card Anaesth. 2021;24:333-8.
- [CrossRef] [PubMed] [Google Scholar]
- Case Report: Thoughts on Two Cases of Total Anomalous Pulmonary Venous Connection Complicated with Pulmonary Artery Hypertension. Front Cardiovasc Med. 2023;10:1075168.
- [CrossRef] [PubMed] [Google Scholar]
- Successful Surgical Repair of Isolated Supra-cardiac Total Anomalous Pulmonary Venous Connection (TAPVC) with Venous Confluence Stenosis Using Dual Anastomosis: A Case Report from Syria. J Surg Case Rep. 2024;2024:rjae621.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the Pulmonary Venous Entry Site Morphology on Postoperative Pulmonary Vein Stenosis in Total Anomalous Pulmonary Venous Connection Patients. J Formosan Med Assoc 2024
- [CrossRef] [Google Scholar]
- Current Outcomes and Treatment of Tetralogy of Fallot. F1000Research. 2019;8:F1000. Faculty Rev-1530.
- [CrossRef] [PubMed] [Google Scholar]
- Case Report: Thoughts on Two Cases of Total Anomalous Pulmonary Venous Connection Complicated with Pulmonary Artery Hypertension. Front Cardiovasc Med. 2023;10:1075168.
- [CrossRef] [PubMed] [Google Scholar]
- Partial Anomalous Pulmonary Venous Connection with Ventricular Septal Defect and Intact Atrial Septum. J Card Crit Care TSS. 2024;8:109-12.
- [CrossRef] [Google Scholar]
- Technical Details of a Novel Surgical Procedure of Anomalous Left Coronary Artery from the Pulmonary Trunk in a Child Using Autogenous Aortic and Pulmonary Arterial Flaps (UKC's Modification): A Video Presentation. J Card Crit Care TSS. 2024;8:53-6.
- [CrossRef] [Google Scholar]
- Dual Drainage of TAPVR-An Exquisite Connection. J Card Crit Care TSS. 2021;5:174-5.
- [CrossRef] [Google Scholar]







