Translate this page into:
To Assess the Impact of Glucose, Insulin, and Potassium Chloride Infusions in Patients after Cardiothoracic Surgery on Arrhythmias and Outcome
*Corresponding author: Lakshminarayana Tharra, Department of Critical Care, Apollo Hospital, Hyderabad, Telangana, India. laxman377@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tharra L, Parveen N, Dikshit V, Subba Reddy K, Sirga S, Venturumilli R. To Assess the Impact of Glucose, Insulin, and Potassium Chloride Infusions in Patients after Cardiothoracic Surgery on Arrhythmias and Outcome. J Card Crit Care TSS. 2025;9:29-34. doi: 10.25259/JCCC_38_2024
Abstract
Objectives:
The role of glucose, insulin, and potassium chloride (GIK) infusions on arrhythmias after cardiothoracic surgery was widely studied. Optimization of myocardial glucose uptake, ischemia damage, and arrhythmias is reduced by GIK infusion. Most of the research was conducted when GIK infusion was utilized intraoperatively. Studies done to know the impact of GIK infusions on rhythm issues after cardiothoracic surgery were contradictory, some studies showed positive results whereas other studies indicated that GIK solution usage after cardiothoracic surgery has no role in preventing arrhythmias. Therefore, the use of GIK infusion to prevent arrhythmias in patients recovering from cardiac surgery is still debatable, necessitating the completion of additional research before a conclusion can be drawn. (1) Primary objective: To determine whether GIK infusions can prevent arrhythmias after cardiac surgery. (2) Secondary objective: To know outcome parameters such as inotropic requirement, ventilatory hours, stay in Intensive Care Unit (ICU).
Material and Methods:
This is a randomized control trail including patients of both sexes aged 20–60 years, who were shifted to post-operative cardiothoracic ICU unit of Apollo Multi-specialty Hospital (Jubilee hills, Hyderabad), after undergoing cardiothoracic surgery (Coronary artery bypass graft and valve replacement or repair). The study was done from June 2023 to February 2024. Following the fulfillment of the relevant inclusion criteria, a total of 100 patients were assigned to two groups equally: The study GIK and control (non-GIK) groups through computer-based randomization. Once the patient is shifted to post-operative cardiothoracic unit after cardiac surgery, GIK infusion (40 IU/L of human actrapid and 40 meq/L potassium chloride was added to 10% dextrose solution) is given to the GIK group, with flow rate of 30 mL/h. The infusion continued for 48 h following surgery. In non-GIK group, normal saline or other intravenous fluid was started as per requirement.
Results:
The demographic characteristics of the study group (GIK group) and control group (non-GIK group) are similar. The control group was observed to have more arrhythmias compared to the study GIK group with a significant P < 0.001. The odds ratio is 0.1976 and confidence interval 95% between the two groups is 0.084–0.465. The incidence of atrial fibrillation was high among all arrhythmias in non GIK group, while the GIK group had a higher incidence of premature ventricular contractions. The non-GIK group experienced longer ionotropic support than the study group (GIK group) with significant P < 0.001. The non-GIK group had higher rates of ventilatory support requirements and increased duration of ICU stay (P = 0.002 and <0.001). Significant side effects were not observed with GIK infusion.
Conclusion:
GIK infusion after cardiac surgery helps to minimize post-operative arrhythmias and is linked to better post-operative outcomes, such as lower requirement of ionotropic support and early extubation leading to decreased length of stay in the ICU. There are no noteworthy non-cardiac problems linked to the use of GIK infusion. Therefore, we advise using GIK infusion to prevent and lessen arrhythmias in suitable patients after cardiac surgery in the ICU, thereby reducing the duration of ICU stay.
Keywords
Arrhythmias
Cardiothoracic surgery (Coronary artery bypass grafting and valve surgery)
Glucose insulin potassium
Ionotropic support
Infusion
INTRODUCTION
For many years, cardiac protection has been accomplished through the usage of glucose, insulin, and potassium (GIK) solution during cardiac surgery. Few studies showed that when GIK infusion was started early in patients who were presented with acute myocardial infarction it resulted in reduced morbidity and mortality.[1,2] Improved ventricular performance and a smaller infarct size are associated with GIK infusion. Few studies evaluated the use of GIK solution in cardiac surgery patients and demonstrated its effectiveness in lowering mortality and improving post-operative morbidity, but some studies concluded that perioperative GIK usage does not significantly lower death and arrhythmias in patients undergoing cardiac surgeries.[3-5]
Following cardiac surgery, GIK administration was linked to better post-operative contractile function and a lower risk of atrial arrhythmias according to a study done by Ranucci et al.6 Therefore, the use of GIK solution to prevent arrhythmias in patients who are undergoing cardiac surgery is still debatable, necessitating the completion of more research before a conclusion can be drawn. Most of the research was conducted in settings where GIK infusions were initiated during surgery. Considering this, I intended to carry out a prospective randomized controlled study to determine how post-operative infusions of GIK affect the course of rhythm issues and outcome after cardiothoracic surgery.
Aims and objectives
Primary objective: To determine whether GIK infusions can prevent arrhythmias after cardiac surgery.
Secondary objective: To know outcome in terms of ionotropic support, ventilatory hours and stay in intensive care unit (ICU).
MATERIAL AND METHODS
This prospective randomized clinical trial which lasted for 9 months. Total number of patients included was 100 in number who were randomly allocated to two groups equally. Randomization was done by computerized method. The study was not blinded.
Study group (GIK group); once the patient is shifted to post-operative cardiothoracic unit after cardiac surgery, GIK infusion (40 IU/L of human actrapid and 40 meq/L potassium chloride was added to 10% dextrose solution) given to the GIK group, with flow rate of 30 mL/hr. The infusion continued for 48 h following surgery.
Control group (non-GIK group); in non-GIK group, normal saline or other intravenous fluid was started as per requirement. Patients aged 20–60 years who underwent cardiac surgery and met the inclusion criteria were included in the study.
Study design
This is a prospective randomized controlled study.
Study population
Patients who underwent cardiac surgery and admitted to ICU, Apollo Hospitals, Jubilee Hills, Hyderabad.
Study period
From June 2023 to February 2024.
Sample size
As per previous studies done to know the role of GIK in preventing arrhythmias in cardiac surgery, the adequate sample size needed for appropriate power of the study was calculated using online calculator (study population was N = 120 in 12 months as per previous studies) by benchmark 6 sigma calculators. The sample size was estimated to be 98, which was rounded up to 100.
Atrial fibrillation (AF) with a recent onset or other arrhythmias, namely, premature ventricular contractions (PVCs), ventricular tachycardia, ventricular fibrillation, and atrial flutter that need medical attention were classified as postoperative arrhythmias. Incidence of arrhythmias, duration of ionotropic support, ventilatory support, and ICU stay were noted. Ionotropic scores in the both groups not taken into consideration.
Inclusion criteria
Patients undergoing elective cardiac surgery (both coronary artery bypass grafting and valve surgery) in the age group of 20–60 years (both males and females) and admitted to postoperative ICU were included in the study. Patients with the left ventricular ejection fraction (EF) of >45% with normal right ventricle function is taken into consideration. Most of the patients included in both the study and control groups are on beta-blockers preoperatively.
Exclusion criteria
Known diabetic patients
Patients with preoperative renal dysfunction
Patients undergoing emergency surgery will be excluded
History of arrhythmias.
RESULTS
The demographic characteristics of the study group (GIK group) and control group (non-GIK group) are similar [Table 1]. A significant difference was observed between the GIK and non-GIK group with respect to incidence of arrhythmias (P < 0.001), a greater number of arrhythmias are seen in control group Figure 1, Table 2. The odds ratio is 0.1976 and confidence interval 95% between the two groups is 0.084–0.465. The incidence of AF was high among all arrhythmias in non GIK (control) group, while the GIK (study) group had a higher incidence of ectopics PVCs Figure 2, Table 3. The non-GIK group experienced longer ionotropic support than the study group (GIK group) with significant P < 0.002 Figure 3, Table 4. The non-GIK group had higher rates of mechanical ventilation hours and increased duration of ICU stay (P = 0.002 and < 0.001) Figures 4 and 5, Tables 5 and 6.
| Variable | GIK Group, n=50 | Non GIK group, n=50 | P-value |
|---|---|---|---|
| Age | 41.4±12 | 41.3±12.2 | 0.76 |
| Sex | Male40 | Male42 | 0.95 |
| Female10 | Female8 | ||
| Diabetes mellitus | Yes15 | Yes17 | 0.668 |
| No35 | No33 | ||
| Hypertension | Yes29 | Yes22 | 0.161 |
| No21 | No28 | ||
| Hypothyroidism | Yes2 | Yes3 | 0.646 |
| No48 | No47 | ||
| Ejection Fraction | |||
| Moderate (30–50%) | 32 | 28 | 0.45 |
| Good (> 50%) | 18 | 22 | 0.4 |
GIK:Glucose-Insulin- Potassium, Non-GIK:Non-Glucose-Insulin- Potassium.
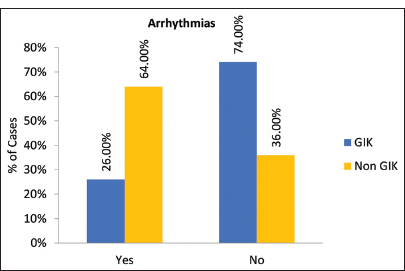
- Incidence of arrhythmias among GIK and Non GIK groups. GIK: Glucose-Insulin- Potassium, Non GIK: Non- Glucose-Insulin- Potassium.
| Arrhythmias | Group | Total | |
|---|---|---|---|
| GIK | Non GIK | ||
| Yes | 13 | 32 | 45 |
| No | 37 | 18 | 55 |
| Total | 50 | 50 | 100 |
| P-value | <0.001 | ||
| (Chisquare test) | |||
| Odds Ratio | 0.1976 | ||
| CI 95% | 0.0840–0.4652 | ||
GIK: Glucose-Insulin- Potassium, Non-GIK: Glucose-Insulin- Potassium,CI: Confidence interval
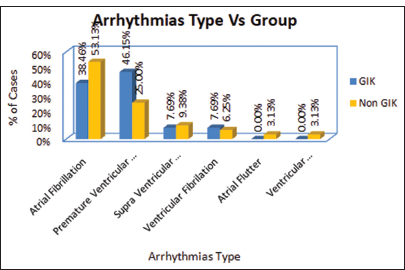
- Shows comparison of incidence of various Arrhythmias between GIK and Non GIK group. GIK: Glucose-Insulin-Potassium.
| Arrhythmias type | Group | Total | |
|---|---|---|---|
| GIK | Non GIK | ||
| Atrial Fibrillation | 5 | 17 | 22 |
| Premature Ventricular Contractions | 6 | 8 | 14 |
| Supra Ventricular Tachycardia | 1 | 3 | 4 |
| Ventricular Fibrillation | 1 | 2 | 3 |
| Atrial Flutter | 0 | 1 | 1 |
| Ventricular Fibrillation+Tachycardia | 0 | 1 | 1 |
| Total | 13 | 32 | 45 |
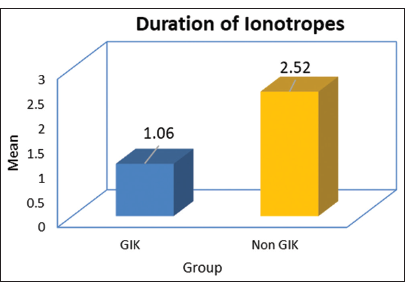
- Comparison of the duration of ionotropic requirement between GIK and Non GIK groups. GIK:Glucose-Insulin-Potassium, Non GIK: Non- Glucose-Insulin- Potassium.
| Group | Duration of Ionotropes (days) | P-value (t-test) | |
|---|---|---|---|
| Mean | Standard deviation | ||
| GIK | 1.06 | 0.978 | <0.001 |
| Non GIK | 2.52 | 0.789 | |
GIK: Glucose, insulin and potassium
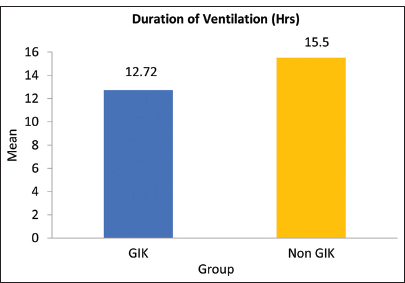
- Graph depicting that duration of mechanical ventilation is more in Non-GIK group when compared to GIK group.GIK: Glucose-Insulin- Potassium, Non GIK: Non- Glucose-Insulin-Potassium.
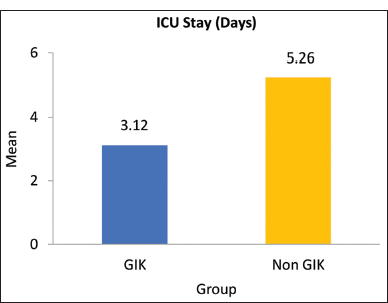
- Comparison of ICU length of stay between GIK and Non GIK group. GIK: Glucose-Insulin- Potassium, Non-GIK: Non-Glucose-Insulin- Potassium.
| Group | Duration of Ventilation (h) | P-value (t-test) | |
|---|---|---|---|
| Mean | Standard deviation | ||
| GIK | 12.72 | 1.679 | 0.002 |
| Non GIK | 15.50 | 5.870 | |
GIK: Glucose, insulin and potassium
| Group | ICU stay (Days) | P-value (t-test) | |
|---|---|---|---|
| Mean | Standard deviation | ||
| GIK | 3.12 | 0.773 | <0.001 |
| Non GIK | 5.26 | 0.664 | |
GIK: Glucose, insulin and potassium, ICU: intensive care unit
DISCUSSION
Fatty acids are the main source of energy for non-ischemic cardiac tissue, providing 60–70% of the overall energy requirements of the heart. These fatty acids are harmful during ischemia because they raise oxygen demand, decrease glucose consumption, and increase the risk of O2 free radical production in the heart, which can lead to arrhythmias.[6,7] Therefore, myocardium may benefit from the supply of exogenous glucose substrate during ischemia. GIK infusion can cause metabolic changes during ischemia and reperfusion, such as decreased oxidation of free fatty acids, enhanced oxidation of glucose, increased glycolysis, and increased absorption of oxygen for the synthesis of adenosine triphosphate (ATP) and its use for enhanced cardiac contractility.[8] In addition, GIK contributes to the activation of K-ATP channels that are signaled by insulin. These channels are crucial ischemic pre-conditioning mediators that provide strong defense against myocardial ischemia (ischemia reperfusion damage). By raising the open state probability and lowering the ATP sensitivity of K-ATP channels, insulin plays a crucial part in controlling these channels.
In addition, GIK infusion has been shown to possess inotropic and vasodilator qualities. In 2004, Bothe et al. carried out an analysis to assess the function of GIK infusion in cardiothoracic surgery. The results suggest that GIK may significantly lessen atrial arrhythmias incidence during cardiothoracic surgery and increase recovery of contractile function postoperatively. To properly evaluate the effectiveness of GIK following heart surgery, large-scale randomized multicenter trials are necessary, as a number of factors restrict the power of this analysis.[9]
To determine the impact of GIK infusion on arrhythmias and mortality after cardiac surgery, Rabi et al. conducted a systematic meta-analysis in 2010. They concluded patients who have undergone cardiothoracic surgery, perioperative use of GIK infusion does decrease mortality or arrhythmias.[10] The usage of GIK infusion in patients undergoing cardiothoracic surgery should be avoided until future trials results supporting GIK infusions are published, as the safety of these infusions has not been well investigated.[11]
In 2015, Ahmad et al. studied how GIK chloride infusion during adult cardiothoracic surgery protected the myocardium. Patients were randomly allocated equal groups equally: Study group or control group. A dextrose solution containing human actrapid and potassium chloride was given to the GIK group.[12] After the anesthesia was induced but before cardiopulmonary bypass began, flow rate of the infusion was 30 mL/h. When the clamp was removed from aorta, the infusion was resumed and maintained for 6 h. According to study findings, GIK infusion improves post-operative outcomes and plays a positive role in myocardial protection without raising the risk of non-cardiac complications.[13,14]
In 2016, Zhao et al. conducted research to determine if patients undergoing cardiopulmonary bypass surgery benefit from modified GIK regimens in terms of improved tissue perfusion and cardio-protection. They concluded that patients undergoing cardiopulmonary bypass surgery have a lesser significant adverse cardiac event in the hospital when they are offered a modified GIK regimen perioperatively.[15,16] These advantages most likely come from improved myocardial metabolism and increased systemic tissue perfusion brought on by GIK[17,18] activating insulin signaling.
In our study, we discovered that the GIK (study) group had a lesser incidence of arrhythmias than the control (non-GIK) group (P < 0.002 and confidence interval 95% 0.074–0.565). The GIK group also had shorter ventilatory and ionotropic support durations, which reduced morbidity and ICU stay after surgery. Non-GIK group showed longer duration of mechanical ventilation due to increase in incidence of arrhythmias and hemodynamic instability. The type of surgeries between GIK and Non GIK groups are also comparable [Figure 6, Table 7].
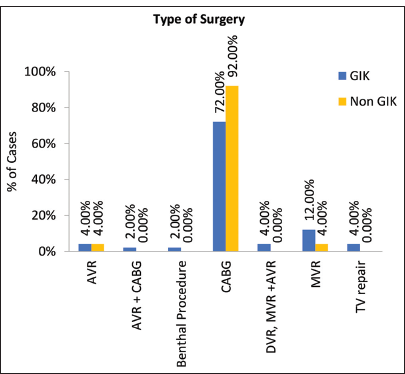
- Graph projecting the comparison of type of surgery between GIK and Non-GIK group. GIK:Glucose-Insulin- Potassium, Non GIK: Non- Glucose-Insulin- Potassium, AVR: Aortic valve repalcement, CABG: Coronary Artery Bypass Graft, DVR: Double valve repalcement, MVR: Mitral valve replacement, TV repair: Tricuspid valve repair..
| Surgery | Group | Total | |
|---|---|---|---|
| GIK | Non GIK | ||
| AVR | 2 | 2 | 4 |
| AVR+CABG | 1 | 0 | 1 |
| Benthal procedure | 1 | 0 | 1 |
| CABG | 36 | 46 | 82 |
| DVR, MVR+AVR | 2 | 0 | 2 |
| MVR | 6 | 2 | 8 |
| TV repair | 2 | 0 | 2 |
| Total | 50 | 50 | 100 |
| P-value | 0.162 | ||
| (Chisquare test) | |||
AVR: Aortic valve replacement, CABG: Coronary artery bypass grafting, DVR: Double valve replacement, MVR: Mitral valve replacement, GIK: Glucose, insulin, and potassium and TV repair: Tricuspid valve repair.
The supplementary table depicts the data collected in both GIK and Non GIK groups with respect to various parameters. Side effects observed with GIK infusion are hyperkalemia and hyperglycemia which was manageable.
Limitations
Study is not blinded
Single-centered study done in Apollo hospital, Jubilee hills Hyderabad
Patients with normal left ventricular EF were taken into consideration and also ionotropic scores not done.
CONCLUSION
GIK chloride infusion after cardiothoracic surgery helps to minimize post-operative arrhythmias and is linked to better post-operative outcomes, such as lower requirement of ionotropic support and early extubation, leading to reduced stay in the intensive care unit after surgery. There are no noteworthy non-cardiac problems linked to the use of GIK infusion.
Therefore, we advise using GIK infusion to prevent and lessen arrhythmias in suitable patients after cardiac surgery in the ICU, thereby reducing the duration of ICU stay.
Ethical approval:
The research/study approved by the Institutional Review Board at Apollo Hospital, number AHJ-C-S-002/01-23, dated 06th May 2023.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Financial support and sponsorship:
Nil.
References
- Glycemic Control and Outcome Related to Cardiopulmonary Bypass. Best Pract Res Clin Anaesthesiol. 2015;29:177-87.
- [CrossRef] [PubMed] [Google Scholar]
- Cardioprotective Effects of Insulin: How Intensive Insulin Therapy May Benefit Cardiac Surgery Patients. Circulation. 2012;125:721-8.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Coronary Syndromes: Early Metabolic Modulation-a Solution for MI? Nat Rev Cardiol. 2012;9:377-8.
- [CrossRef] [PubMed] [Google Scholar]
- Forty Years of Glucose-insulin-potassium (GIK) in Cardiac Surgery: A Review of Randomized, Controlled Trials. Eur J Cardiothorac Surg. 2006;29:479-85.
- [CrossRef] [PubMed] [Google Scholar]
- Mitochondrial ATP-sensitive Potassium Channels Inhibit Apoptosis Induced by Oxidative Stress in Cardiac Cells. Circ Res. 2001;88:1267-75.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperlactatemia during Cardiopulmonary Bypass: Determinants and Impact on Postoperative Outcome. Crit Care. 2006;10:R167.
- [CrossRef] [PubMed] [Google Scholar]
- Nitric Oxide Mediates the Antiapoptotic Effect of Insulin in Myocardial Ischemia Reperfusion: The Roles of PI3-kinase, Akt, and Endothelial Nitric Oxide Synthase Phosphorylation. Circulation. 2002;105:1497-502.
- [CrossRef] [PubMed] [Google Scholar]
- Glucose-insulin-potassium Therapy in Adult Patients Undergoing Cardiac Surgery: A Meta-analysis. Eur J Cardiothorac Surg. 2011;40:192-9.
- [CrossRef] [PubMed] [Google Scholar]
- Glucose-Insulin-Potassium in Cardiac Surgery: A Meta-analysis. Thorac Surg. 2004;78:1650-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Perioperative Glucose-insulin-Potassium Infusions on Mortality and Atrial Fibrillation after Coronary Artery Bypass Grafting: A Systematic Review and Meta-analysis. J Cardiol. 2010;26:e20-4.
- [CrossRef] [PubMed] [Google Scholar]
- Nitric Oxide Decreases Acute Kidney Injury and Stage 3 Chronic Kidney Disease after Cardiac Surgery. Am J Respir Crit Care Med. 2018;198:1279-87.
- [CrossRef] [PubMed] [Google Scholar]
- Myocardial Protection with Glucose-insulin-potassium Infusion during Adult Cardiac Surgery. Pak J Med Sci. 2017;33:325-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Meta-analysis of Glucose-insulin-potassium Therapy for Treatment of Acute Myocardial Infarction. Exp Clin Cardiol. 2010;15:e20-4.
- [Google Scholar]
- Anti-inflammatory Effect of High-dose Insulin Treatment after Urgent Coronary Revascularization Surgery. Acta Anaesthesiol Scand. 2006;50:962-9.
- [CrossRef] [PubMed] [Google Scholar]
- Modified Glucose-insulin-potassium Regimen Provides Cardioprotection with Improved Tissue Perfusion in Patients Undergoing Cardiopulmonary Bypass Surgery. J Am Heart Assoc. 2020;9:e012376.
- [CrossRef] [PubMed] [Google Scholar]
- Improved Myocardial Protection during Coronary Artery Surgery with Glucose-insulin-potassium: A Randomized Controlled Trial. J Thorac Cardiovasc Surg. 2006;131:34-42.
- [CrossRef] [PubMed] [Google Scholar]
- Preconditioning with Glucose-insulin-potassium Solution and Restoration of Myocardial Function During Coronary Surgery. Gen Physiol Biophys. 2009;28:262-70.
- [Google Scholar]
- Glucose-insulin-potassium (GIK) Solution Used with Diabetic Patients Provides Better Recovery after Coronary Bypass Operations. Med Arch. 2013;67:84-7.
- [CrossRef] [PubMed] [Google Scholar]







