Translate this page into:
The Anesthesiologist as Extracorporeal Membrane Oxygenation Intensivist: Heralding a New Era?
*Corresponding author: Marlice Alida Van Dyk, Intensive Care Unit, Netcare Unitas Hospital, Centurion, South Africa. dr.marlice@icudoctor.co.za
-
Received: ,
Accepted: ,
How to cite this article: Van Dyk MA. Anesthesiologist as Extracorporeal Membrane Oxygenation Intensivist: Heralding a New Era? J Card Crit Care TSS. 2024;8:119-21. doi: 10.25259/JCCC_29_2024
An anesthesiologist’s role is to preserve patient safety and autonomy. In today’s world, with increasingly more complex surgeries being performed, each post-operative patient should be looked after by an anesthesiologist in conjunction with the surgeon and or cardiologist.
Anesthesiologists are perioperative physicians with an intricate knowledge of the disease process, physiology as well as the surgery performed. The public, unfortunately is unaware of what anesthesiologists do in theater and their potential role in the perioperative period.
The American Society of Anesthesiologists branded us as physician anesthesiologists to make it clear to the public what our role should be. Despite this, anesthesiologists are still seen as not essential to the functioning of a busy hospital, and capital spending on anesthetic equipment is minimal.
In this ever-evolving world, anesthesiologists are perfectly qualified to move into leadership roles such as critical care intensivists, extracorporeal membrane oxygenation (ECMO) specialists, pain physicians, and echocardiographers. These specialist branches are just as critical as the role of the perioperative anesthesiologist but do not depend on the surgical disciplines.
Being a part of an ECMO team in South Africa, establishing the ECMO Society of South Africa, being the representative of SWAAC ELSO in South Africa, and doing simulation training on a regular basis, I learned that ECMO is an essential stethoscope in every tertiary intensive care unit (ICU) and all anesthesiologists have a major role to play in managing these patients.
ANESTHESIOLOGISTS ARE GREAT ECHOCARDIOGRAPHERS AND ECMO INTENSIVISTS
Anesthesiologists, in lieu of their training in cardiothoracic anesthesia and bypass surgery, are perfectly positioned to be ECMO intensivists. They have excellent skills in echocardiography (ECHO) and extracorporeal therapies (ECMO). A lifesaving procedure such as ECMO needs good imaging for success and better patient outcomes.[1] The placement of cannulas and the right patient selection for ECMO all require ECHO.[2] [Figure 1] An in-depth knowledge of ECHO on ECMO can only be provided by an anesthesiologist or intensivist trained in both modalities. ECHO plays a fundamental role in the management of patients supported with ECMO.[3] [Figure 2] It is particularly useful for the detection of cardiac complications that may arise during ECMO. ECHO aids in the smooth ECMO run [Flowchart 1].[4]
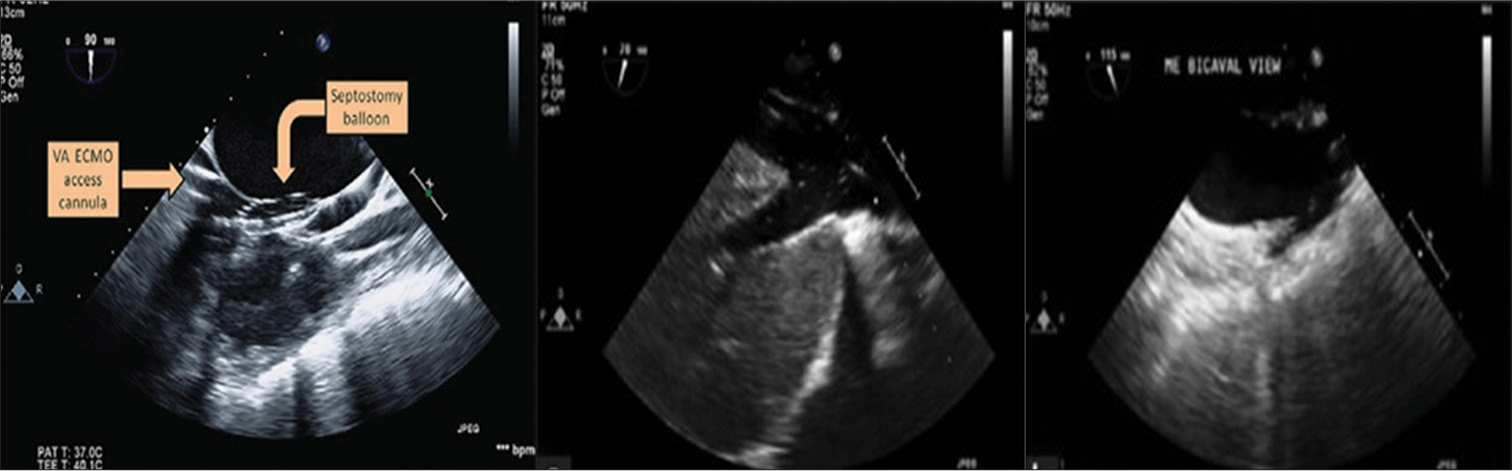
- Transesophageal echocardiography is an effective tool in guiding the balloon atrial septostomy catheter and balloon inflation.
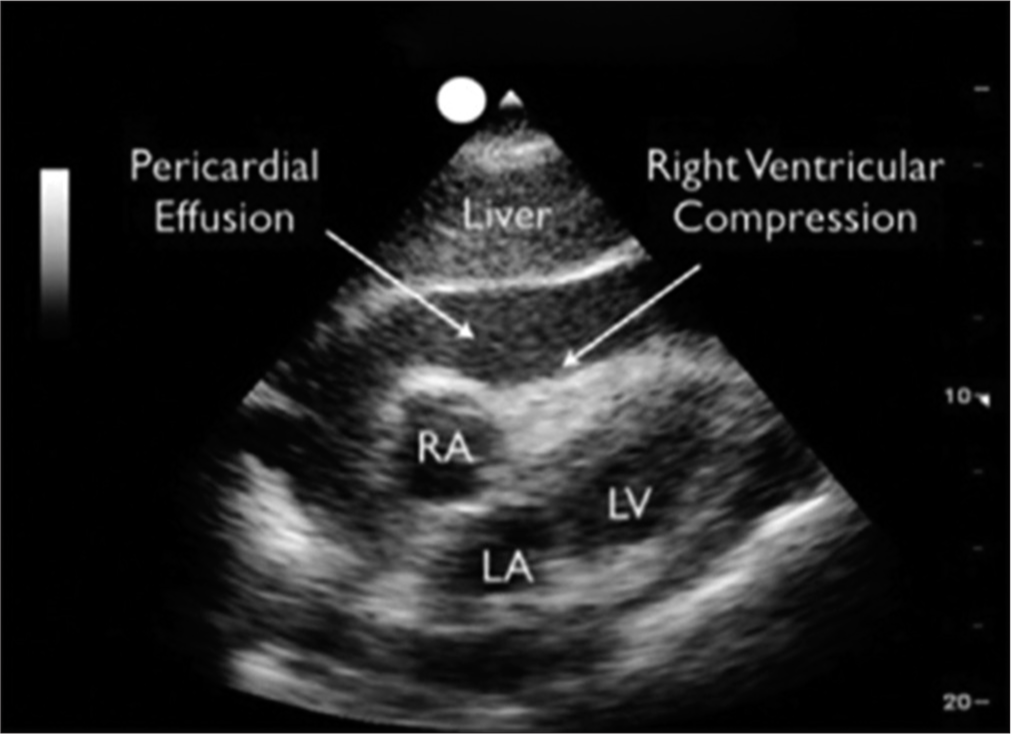
- Pericardial tamponade detected by echocardiography when on extracorporeal membrane oxygenation (ECMO), RA: Right Atrium, LA: Left Atrium, LV: Left Ventricle.
|
TYPES OF EXTRACORPOREAL MEMBRANE OXYGENATION
ECMO is a supportive therapy used to provide cardiac and/or respiratory support for critically ill patients in whom maximal conventional medical management has failed. There are two types of ECMO – veno-venous ECMO (VVECMO) and veno-arterial ECMO (VA-ECMO). VV ECMO provides oxygenation and carbon dioxide removal in isolated refractory respiratory failure. VA-ECMO is preferred when support is needed for cardiac and/or respiratory failure.
Complications such as thrombosis or displacement of cannulae of the ECMO circuit can be seen on ECHO with two-dimensional or three-dimensional ECHO. ECHO is mandatory during initiation of ECMO, cannula insertion, hemodynamic monitoring, and detecting of complications during weaning and is an essential monitoring tool during a successful ECMO run.
Post-operative analgesia is an extremely important part of the post-operative care of these patients and aids in early mobilization, shorter ICU length of stay, and attenuation of stress response. Various regional analgesia techniques can be used, such as thoracic epidural and interpleural anesthesia,[5] subarachnoid analgesia,[6] and paravertebral block, and, nowadays, local anesthetic infusion into the wound. Cardiac anesthetists can manage all these better than other critical care specialists or cardiac surgeons. Cardiac anesthesiologists are best equipped to be in charge of a cardiac ICU, but they also need to be trained in critical care management.
Having an anesthesiologist intensivist as part of a mobile ECMO team adds a great skill set through an understanding of cardiac and respiratory compromise and the nuances of mechanical circulatory support devices that allow them to be able to manage the device and hemodynamics during transport. In addition, the cardiac critical care anesthesiology intensivist serving as a shock consultant would play a key role in this process and would lead the effort to identify which patients may benefit from mobile ECMO initiation.
The INTERMACS categorization system should be understood by all ECMO intensivists dealing with patients with heart failure.[7] Fluency in pathways for patients who fail to wean from ECMO must be achieved. Initiation and management of ECMO and other ECLS devices used for advanced respiratory and cardiac failure, including extracorporeal cardiopulmonary resuscitation, is necessary.[8] For all this, an anesthesiologist as a perioperative physician is an ideal clinician, this time not behind the curtains during patient surgery but far ahead of others as a “Skilled perioperative and post-operative physician intensivist.”
References
- Echocardiography in Extracorporeal Membrane Oxygenation. Ann Card Anaesth. 2017;20(Supplement):S1-3.
- [CrossRef] [Google Scholar]
- Anticoagulation during ECMO: Will the Tight Rope be Tighter in 2018? J Card Crit Care TSS. 2017;1:55-6.
- [CrossRef] [Google Scholar]
- The Role of Echocardiography in the Management of Patients Supported by Extracorporeal Membrane Oxygenation. J Am Soc Echocardiogr. 2012;25:131-41.
- [CrossRef] [PubMed] [Google Scholar]
- A Comparative Evaluation of Intrapleural and Thoracic Epidural Analgesia for Postoperative Pain Relief after Minimally Invasive Direct Coronary Artery Bypass Surgery. J Cardiothorac Vasc Anesth. 1998;12:162-5.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal (Subarachnoid) Morphine for Off-Pump Coronary Artery Bypass Surgery. Heart Surg Forum. 2004;7:E205-10.
- [CrossRef] [PubMed] [Google Scholar]
- Describing Advanced Practice Provider Roles Within Critical Care Teams with Tele-ICUs: Exemplars from Seven US Health Systems. Nurs Outlook. 2020;68:5-13.
- [CrossRef] [PubMed] [Google Scholar]
- Developing Cardiothoracic Surgical Critical Care Intensivists: A Case for Distinct Training. Medicina (Kaunas). 2022;58:1865.
- [CrossRef] [PubMed] [Google Scholar]





