Translate this page into:
Ten Recommendations for Managing Bleeding in Pediatric Cyanotic Cardiac Surgery
*Corresponding author: Klaus Görlinger, Department of Anaesthesiology and Intensive Care Medicine, University Hospital Essen, Essen, Germany. kgoerlinger@werfen.com
-
Received: ,
Accepted: ,
How to cite this article: Kammerer T, Görlinger K, Kapoor PM. Ten Recommendations for Managing Bleeding in Pediatric Cyanotic Cardiac Surgery. J Card Crit Care TSS. 2025;9:78-83. doi: 10.25259/JCCC_56_2024
Abstract
The recommended treatment options for coagulation management during cardiac surgery include fibrinogen concentrate, packed red blood cells, fresh frozen plasma, platelet concentrate (pooled donors or single donor), cryoprecipitate, recombinant factor VIIa, tranexamic acid, epsilon aminocaproic acid, prothrombin complex concentrate, as well as antidotes such as protamine and desmopressin. At present, only the top institutes in the world have TEG and ROTEM testing facilities available for bleeding patients or selected patient populations undergoing major cardiovascular surgery or liver transplantation. TEG and ROTEM should be made available more widely (for all bleeding patients and patients at high risk of bleeding in tertiary hospitals) across India. Inconvenience caused by planning and requesting of blood components and multiple institute-specific hindrances delaying the availability of blood components can be resolved by having factor concentrates available and stored in the operation theater. This approach may reduce transfusion requirements, morbidity, mortality, and healthcare costs.
Keywords
Algorithms
Bleeding management
Cyanotic heart disease
Pediatric cardiac surgery
Thromboelastometry
Transfusion
INTRODUCTION
The recommended treatment options for coagulation management during cardiac surgery include fibrinogen concentrate, packed red blood cells, fresh frozen plasma (FFP), platelet concentrates (pooled donors or single donor), cryoprecipitate, recombinant factor VIIa, tranexamic acid, epsilon aminocaproic acid (EACA), prothrombin complex concentrate (PCC), as well as antidotes such as protamine and desmopressin. The recommended tests for predicting/assessing bleeding during cardiac surgery are extrinsically activated thromboelastometric test (EXTEM), fibrin-based thromboelastometry test (FIBTEM), intrinsic thromboelastometry test (INTEM) and heparinase assay based thromboelastometry test (HEPTEM), Kaolin-thromboelastography (TEG), Heparinase-TEG, Rapid-TEG, and TEG-FF as well as platelet function testing such as Multiplate, rotational thromboelastometry (ROTEM) platelet, VerifyNow, TEG platelet mapping, as well as activated clot time (ACT) and blood gas analysis.
A pre-operative multidisciplinary bundle to discuss aspects such as invasive monitoring, cannulation sites, management of cardiopulmonary bypass (CPB), post-bypass inotropic support, chest closure, ventilatory support, and blood conservation management planning is encouraged for best alignment. Pre-operatively patients at high risk of bleeding can be identified by checking for iron-deficiency anemia, non-iron-deficiency anemia, fibrinogen level, and platelet function testing in patients taking P2Y12 inhibitors or dual antiplatelet therapy.
KEY POINTS TO BE OBSERVED IN BLEEDING PATIENTS
When excessive bleeding occurs perioperatively, the following key points must be considered in such bleeding management algorithms [Figure 1]:
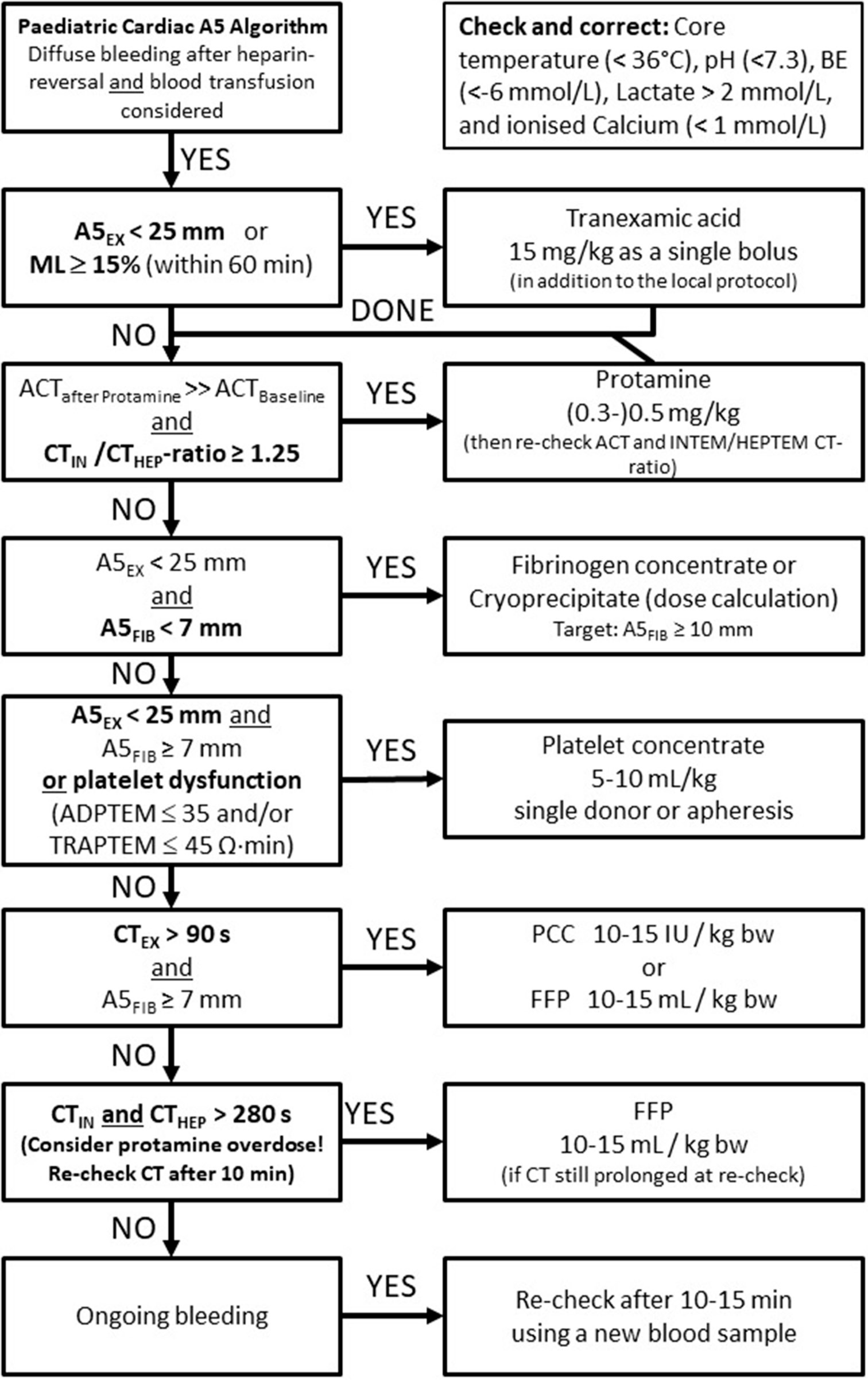
- Evidence-based thromboelastometry (ROTEM)-guided bleeding management algorithm for pediatric cardiac surgery (Courtesy of Klaus Görlinger, Essen, Germany). ML: Maximum lysis, FFP: Fresh frozen plasma, PCC: Prothrombin complex concentrate, ACT: Activated clot time, TRAPTEM: ROTEM platelet assay with thrombin receptor-activating peptide, HEPTEM: Heparinase-based thromboelastometric assay. ADPTEM: Adenosine di-phosphate based thromboelastometric test, ROTEM: Rotational thromboelastometry.
The pathophysiology of cyanotic congenital heart disease (CCHD) and non-CCHD with its impact on hematocrit and fibrinogen availability. Here, FIBTEM clot firmness (A5, A10, maximum clot firmness [MCF]) better reflects fibrinogen availability in whole blood rather than Clauss fibrinogen plasma concentration since the plasma volume is significantly reduced in CCHD.[1,2]
Pre-conditions of hemostasis must be considered in perioperative bleeding management. Here, hypothermia (core temperature <36°C), acidosis (pH <7.3; base excess [BE] <−6 mmol/L; Lactate >2 mmol/L), and hypocalcemia (ionized Ca++ <1 mmol/L) should be avoided and must be corrected before hemostatic interventions aiming at increased thrombin generation.[3,4]
Time is life in severe bleeding! Therefore, viscoelastic testing results must be available 10–15 min after blood sampling to detect and specify coagulopathic bleeding in real time. Here, early clot firmness amplitudes (A5 and A10) are key for success.[5] Furthermore, interdisciplinary communication, collaboration, and consensus are crucial to provide the therapeutic interventions (allogeneic blood products, coagulation factor concentrates, and hemostatic drugs) in a timely manner. This is most important for blood products with a long turn-around time, such as cryoprecipitate and platelets. Here, thromboelastometry measurements during CPB under full heparinization can facilitate, on the one hand early diagnosis of coagulopathy and avoid a delay in therapy, and, on the other hand, can avoid unnecessary ordering of blood products and factor concentrates if coagulopathy can be ruled out.[6] Thromboelastometry measurement under full heparinization on CPB can be done since all thromboelastometric assays except INTEM include a heparin inhibitor, eliminating the effect of 5–7 U/mL unfractionated heparin (UFH). Extrinsically activated assays (EXTEM, FIBTEM, and APTEM) use polybrene for fast elimination of up to 5 U/mL UFH, and HEPTEM uses heparinase for the elimination of up to 7 U/mL UFH.
Antifibrinolytic drugs (TXA or EACA) can be given prophylactically in patients undergoing cardiac surgery with CPB and can be topped up in case of detection of hyperfibrinolysis by thromboelastometry.[7,8]
Heparin-reversal by protamine should be done in a careful way (protamine dose of 60–80% of the primary heparin dose) since protamine overdose is associated with significant factor V inhibition and platelet dysfunction.[9] Furthermore, prolonged ACT is not specific for a residual heparin effect. Protamine overdose can prolong ACT significantly, too, but can be differentiated from residual heparin effect by INTEM clotting time (CT) to HEPTEM CT ratio. Notably, the most often reason for prolonged ACT in pediatric cardiac surgery is low fibrinogen since hemodilution happens early in pediatric cardiac surgery due to the small blood volume.[10] Accordingly, the detection of hypofibrinogenemia is crucial in pediatric patients undergoing cardiac surgery.
-
Accordingly, detection of and differentiation between hypofibrinogenemia and thrombocytopenia is essential in bleeding patients undergoing cardiac surgery. Here, several studies demonstrated that thromboelastometry rapidly and precisely predicts hypofibrinogenemia and thrombocytopenia during CPB in neonates, infants and children undergoing cardiac surgery.[11,12] A fibrinogen cut-off value below 150 mg/dL corresponding with a FIBTEM A5 below 7 mm is the best predictor for bleeding in pediatric cardiac surgery.[13-15] Furthermore, the targeted increase in FIBTEM A5 allows for a dose calculation for fibrinogen concentrate or cryoprecipitate [Table 1].[15,16] Here, fibrinogen dose calculation is much more precise for fibrinogen concentrate with a standardized fibrinogen concentration of 20 g/L (0.9–1.3 g fibrinogen in a 1 g vial) compared with cryoprecipitate. Fibrinogen concentration in cryoprecipitate depends on the donor and varies widely between 8 and 16 g/L.[16-18]
Table 1: Fibrinogen dose calculation for fibrinogen concentrate and cryoprecipitate based on the targeted increase in FIBTEM clot firmness (A5 or A10).Targeted increase in A5FIB (mm) Fibrinogen dose (mg/kg bw) Fibrinogen concentrate (mL/kg bw) Cryoprecipitate (mL/kg bw) 2 mm 12.5 mg/kg bw 0.6 mL/kg bw 1 mL/kg bw 4 mm 25.0 mg/kg bw 1.2 mL/kg bw 2 mL/kg bw 6 mm 37.5 mg/kg bw 1.9 mL/kg bw 3 mL/kg bw 8 mm 50.0 mg/kg bw 2.5 mL/kg bw 4 mL/kg bw 10 mm 62.5 mg/kg bw 3.1 mL/kg bw 5 mL/kg bw 12 mm 75.0 mg/kg bw 3.8 mL/kg bw 6 mL/kg bw Fibrinogen dose (g) = targeted increase in A5 FIB (mm) × body weight (kg)/160. Correction factor (140–160 mm kg/g) depends on the actual plasma volume. A5 FIB levels of 12–16 mm may compensate for low platelet count or function. A5 FIBTEM: Clot firmness amplitude 5 min after CT in mm; bw: Body weight
Impaired thrombin generation due to coagulation factor deficiency happens late in cardiac surgery since factor VIII is released as a fast acute phase protein from the endothelial cells.[19] Enzymatic coagulation factors that decrease early after CPB are the coagulation factors II, VII, and X and belong to the vitamin K-dependent coagulation factors produced by the liver. Since they belong to the extrinsic pathway, a deficiency can only be detected by viscoelastic assays, which are tissue factor-activated, factor VII-dependent, and heparin-insensitive.[20] This applies for EXTEM CT, only. Kaolin R-time or INTEM CT are looking at the wrong pathway and therefore cannot be used to detect a factor deficiency of the extrinsic pathway. The same applies for patients treated with vitamin K-antagonists or neonates and children with a vitamin K deficiency. Patients with a deficiency of vitamin K-dependent coagulation factors or treated with vitamin K-antagonists (e.g., warfarin) can be treated with 4-factor PCC or FFP. However, the latter bears a high risk of pulmonary complications due to transfusion-associated circulatory overload, transfusion-related acute lung injury, transfusion-related immunomodulation with nosocomial infections, and thrombosis.[21-24]
Prolonged clotting times due to coagulation factor deficiency in the intrinsic pathway are rare - except for patients with hemophilia - and can be treated with specific factor concentrates for hemophilia A (factor VIII) and B (factor IX) or with plasma for other coagulation factor deficiencies such as factor V or factor XI. Anyway, protamine overdose should be considered as a reason for prolonged INTEM and HEPTEM CT.[9,16] Notably, prolonged INTEM and HEPTEM CT due to protamine overdose disappear spontaneously after 15–20 min when additional protamine is bound by heparinoids of the endothelial glycocalyx.
Hypercoagulability (EXTEM MCF >69 mm [EXTEM A5 >49 mm] and/or FIBTEM MCF >22 mm [FIBTEM A5 >19 mm]) are associated with an increased risk of thrombotic complications and should be avoided.[25] Hypercoagulability can also occur due to postoperative acute phase reaction and may require additional anticoagulation.
The results of observational and interventional studies in pediatric cardiac surgery have been summarized in thromboelastometry-guided bleeding management algorithms for this patient population [Figure 1].[26] They should be adapted to the patient population, available diagnostics and therapeutic interventions, and logistics of each hospital. When excessive bleeding occurs in paediatric patients viscoelastic testing by TEG, Sonoclot or ROTEM provides leads to further transfusion.[27-29]
The implementation of thromboelastometry-guided bleeding management algorithms following these recommendations in pediatric cardiac surgery was associated with a significant reduction in post-CPB bleeding, transfusion requirements, post-operative mechanical ventilation time, intensive care unit (ICU) and hospital length of stay, and mortality in cohort studies as well as randomized controlled trials.[30-33]
CONCLUSION
Centers of excellence should be established under the egis of key apex centers to facilitate the establishment of standardized coagulation management protocols. Measures should be taken to enhance awareness about newly available factor concentrates among anesthesiologists and cardiac surgeons in India, as this was not a well-clarified topic in medical graduation curriculum leading to knowledge gaps. At present, only the top institutes in the world have TEG and ROTEM testing facilities for bleeding patients or selected patient populations undergoing major cardiovascular surgery or liver transplantation. TEG and ROTEM should be made available more widely (for all bleeding patients or at high risk of bleeding in all tertiary institutes) across India. Inconvenience caused due to planning and requesting of blood components, and multiple institute-specific hindrances delaying availability of blood components can be resolved by having factor concentrates available and stored in the operation theatre. If cost is an issue, cost reallocation can be considered by reducing costs spent on other products and rather spending/reallocating on factor concentrate, based on cost-effectiveness, convenience, efficacy, and improved patient safety offered by this goal-directed bleeding management. Most important, the implementation of thromboelastometry-guided bleeding management algorithms in pediatric cardiac surgery was associated with a significant reduction in bleeding, transfusion requirements, postoperative mechanical ventilation time, ICU and hospital length of stay, and mortality.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
Dr. Klaus Görlinger and Dr. Poonam Malhotra Kapoor are on the editorial board of the Journal. Dr. Klaus Görlinger works as the Medical Director of TEM Innovations/Werfen PBM, Munich, Germany.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Effect of Haematocrit on Fibrin-based Clot Firmness in the FIBTEM Test. Blood Transfus. 2013;11:412-8.
- [Google Scholar]
- The Association between Cyanosis and Thromboelastometry (ROTEM) in Children with Congenital Heart Defects: A Retrospective Cohort Study. Anesth Analg. 2017;124:23-9.
- [CrossRef] [PubMed] [Google Scholar]
- Hemostatic Defects in Massive Transfusion: An Update and Treatment Recommendations. Expert Rev Hematol. 2021;14:219-39.
- [CrossRef] [PubMed] [Google Scholar]
- Trauma-Induced Disturbances in Ionized Calcium Levels Correlate Parabolically with Coagulopathy, Transfusion, and Mortality: A Multicentre Cohort Analysis from the Trauma Register DGU(®) Crit Care. 2023;27:267.
- [CrossRef] [PubMed] [Google Scholar]
- Early Thromboelastometry Variables Predict Maximum Clot Firmness in Children Undergoing Cardiac and Non-cardiac Surgery. Br J Anaesth. 2015;115:896-902.
- [CrossRef] [PubMed] [Google Scholar]
- Validity of Thromboelastometry for Rapid Assessment of Fibrinogen Levels in Heparinized Samples During Cardiac Surgery: A Retrospective, Single-center, Observational Study. J Cardiothorac Vasc Anesth. 2016;30:90-5.
- [CrossRef] [PubMed] [Google Scholar]
- Tranexamic Acid in Patients Undergoing Coronary-Artery Surgery. N Engl J Med. 2017;376:136-48.
- [CrossRef] [PubMed] [Google Scholar]
- Tranexamic Acid Versus Ɛ-aminocaproic Acid: Efficacy and Safety in Paediatric Cardiac Surgery. Eur J Cardiothorac Surg. 2011;39:892-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anticoagulant and Side-effects of Protamine in Cardiac Surgery: A Narrative Review. Br J Anaesth. 2018;120:914-27.
- [CrossRef] [PubMed] [Google Scholar]
- Prolonged Activated Clotting Time after Protamine Administration Does Not Indicate Residual Heparinization after Cardiopulmonary Bypass in Pediatric Open Heart Surgery. Thorac Cardiovasc Surg. 2015;63:397-403.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive Value of Rotational Thromboelastometry During Cardiopulmonary Bypass for Thrombocytopenia and Hypofibrinogenemia after Weaning of Cardiopulmonary Bypass. Korean J Anesthesiol. 2015;68:241-8.
- [CrossRef] [PubMed] [Google Scholar]
- Rotational Thromboelastometry Rapidly Predicts Thrombocytopenia and Hypofibrinogenemia during Neonatal Cardiopulmonary Bypass. World J Pediatr Congenit Heart Surg. 2018;9:424-33.
- [CrossRef] [PubMed] [Google Scholar]
- Fibrinogen Levels and Postoperative Chest Drain Blood Loss in Low-weight (<10 kg) Children Undergoing Cardiac Surgery. Perfusion. 2019;34:629-36.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation Between ROTEM FIBTEM Maximum Clot Firmness and Fibrinogen Levels in Pediatric Cardiac Surgery Patients. Clin Appl Thromb Hemost. 2019;25:1076029618816382.
- [CrossRef] [PubMed] [Google Scholar]
- Individualized, Intraoperative Dosing of Fibrinogen Concentrate for the Prevention of Bleeding in Neonatal and Infant Cardiac Surgery Using Cardio-pulmonary Bypass (FIBCON): A Phase 1b/2a Randomized Controlled Trial. Circ Cardiovasc Interv. 2020;13:e009465.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of Evidence-based Algorithms for Rotational Thromboelastometry-guided Bleeding Management. Korean J Anesthesiol. 2019;72:297-322.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in Coagulation-relevant Parameters: Comparing Cryoprecipitate and a Human Fibrinogen Concentrate. PLoS One. 2023;18:e0290571.
- [CrossRef] [PubMed] [Google Scholar]
- Theoretical Modelling of Fibrinogen Supplementation with Therapeutic Plasma, Cryoprecipitate, or Fibrinogen Concentrate. Br J Anaesth. 2014;113:585-95.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma Activity of Individual Coagulation Factors, Hemodilution and Blood Loss After Cardiac Surgery: A Prospective Observational Study. Thromb Res. 2010;126:e128-33.
- [CrossRef] [PubMed] [Google Scholar]
- A European Consensus Statement on the Use of Four-factor Prothrombin Complex Concentrate for Cardiac and Non-cardiac Surgical Patients. Anaesthesia. 2021;76:381-92.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric Non-red Cell Blood Product Transfusion Practices: What's the Evidence to Guide Transfusion of the 'Yellow' Blood Products? Curr Opin Anaesthesiol. 2020;33:259-67.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence, Risk Factors, and Outcome of Transfusion-related Acute Lung Injury in Critically Ill Children: A Retrospective Study. J Crit Care. 2015;30:55-9.
- [CrossRef] [PubMed] [Google Scholar]
- Transfusion-Related Acute Lung Injury In A Paediatric Intensive Care Unit Of Pakistan. J Ayub Med Coll Abbottabad. 2017;29:702-5.
- [Google Scholar]
- Perioperative Plasma in Addition to Red Blood Cell Transfusions Is Associated With Increased Venous Thromboembolism Risk Postoperatively. Anesth Analg. 2024;139:254-61.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship Between Transfusion of Blood Products and the Incidence of Thrombotic Complications in Neonates and Infants Undergoing Cardiac Surgery. J Cardiothorac Vasc Anesth. 2017;31:1943-8.
- [CrossRef] [PubMed] [Google Scholar]
- Value of Point-of-Care Algorithms in Pediatric Cardiac Surgery. J Cardiac Crit Care TSS. 2024;8:181-4.
- [CrossRef] [Google Scholar]
- Congenital Cyanotic Cardiac Surgery in Children: Is Algorithm-Based Point-of-Care Testing Essential to Prevent Bleeding? J Cardiac Crit Care TSS. 2018;2:84-90.
- [CrossRef] [Google Scholar]
- Is Rotational Thromboelastometry the Answer for Rapid Prediction of Coagulopathy on Extracorporeal Membrane Oxygenation? J Cardiac Crit Care TSS. 2017;1:108-10.
- [CrossRef] [Google Scholar]
- Reexploration Can Be Deterred by Point-of-Care Testing in Cardiac Surgery Patient. J Card Crit Care TSS. 2017;1:48-50.
- [CrossRef] [Google Scholar]
- A ROTEM-guided Algorithm Aimed to Reduce Blood Product Utilization during Neonatal and Infant Cardiac Surgery. J Extra Corpor Technol. 2023;55:60-9.
- [CrossRef] [PubMed] [Google Scholar]
- Thromboelastometry-guided Intraoperative Haemostatic Management Reduces Bleeding and Red Cell Transfusion after Paediatric Cardiac Surgery. Br J Anaesth. 2015;114:91-102.
- [CrossRef] [PubMed] [Google Scholar]
- A Prospective Randomized Clinical Trial of Efficacy of Algorithm-based Point-of-Care guided Hemostatic Therapy in Cyanotic Congentital Heart Disease Surgical Patients. J Card Crit Care TSS. 2020;3:8-16.
- [CrossRef] [Google Scholar]
- Prospective Interventional Cohort Study using AIIMS Simplified POC Algorithm for Restricted Blood Transfusion in Cyanotic Children. J Card Crit Care TSS. 2024;8:195-204.
- [CrossRef] [Google Scholar]







