Translate this page into:
Partial Anomalous Pulmonary Venous Connection with Ventricular Septal Defect and Intact Atrial Septum
*Corresponding author: Chava Harshanth Sairam, Department of Cardiothoracic and Vascular Surgery, All India Institute of Medical Sciences, New Delhi, Delhi, India. harshanth405@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadav M, Sairam CH. Partial Anomalous Pulmonary Venous Connection with Ventricular Septal Defect and Intact Atrial Septum. J Card Crit Care TSS. 2024;8:109-12. doi: 10.25259/JCCC_62_2023
Abstract
Partial anomalous pulmonary venous connection (PAPVC) is a rare congenital cardiac abnormality in which the pulmonary veins drain into the right atrium directly or the superior vena cava 90% of PAPVC are accompanied by atrial septal defect. However, PAPVC with ventricular septal defect is a rare entity.
Keywords
Anomalous pulmonary venous connection
Ventricular septal defect
Intact atrial septum
INTRODUCTION
The condition in which few pulmonary veins (PVs) drain directly into the right atrium (RA) or superior vena cava (SVC) is called a partial anomalous pulmonary venous connection (PAPVC).[1] PAPVC is a rare congenital cardiac anomaly. An associated atrial septal defect (ASD) is seen in 90% of cases of PAPVC.[2] PAPVC with isolated ventricular septal defect (VSD) is a rare congenital cardiac malformation.[3]
CASE REPORT
A six-month-old male infant was brought to our center in view of poor weight gain, rapid breathing during feeding, and recurrent episodes of lower respiratory tract infection. On examination, the baby was alert, had a heart rate of 120/min, and had a hyperdynamic precordium with a pan systolic murmur. Chest X-ray showed features of increased pulmonary blood flow, electrocardiography suggestive of normal sinus rhythm, normal P wave axis, and QRS right axis deviation. On echocardiography, the baby had upper muscular VSD (5.5 mm), and pulmonary arterial hypertension was out of proportion to the size of VSD; in echocardiography, there is increased flow in the SVC. Computed tomography (CT) angiography was performed, and the left superior pulmonary vein (LSPV) opened into the left brachiocephalic vein; however, the authors could not find any ASD or patent foramen ovale [Figures 1 and 2]. The baby was taken up for VSD closure and PAPVC repair. Transesophageal echocardiography showed anomalous drainage of left upper pulmonary vein into innominate vein [Figure 3]. Intraoperative findings were – upper muscular VSD was present, VSD closure was done with a Dacron patch, LSPV (1 cm in diameter) was seen draining into the left brachiocephalic vein, and LSPV was extra pericardial and extra-pleural in location [Figure 4]. LSPV was mobilized through a defect made in the pericardium and anastomosed to the left atrial appendage, and the foramen ovale is left open [Figure 5].
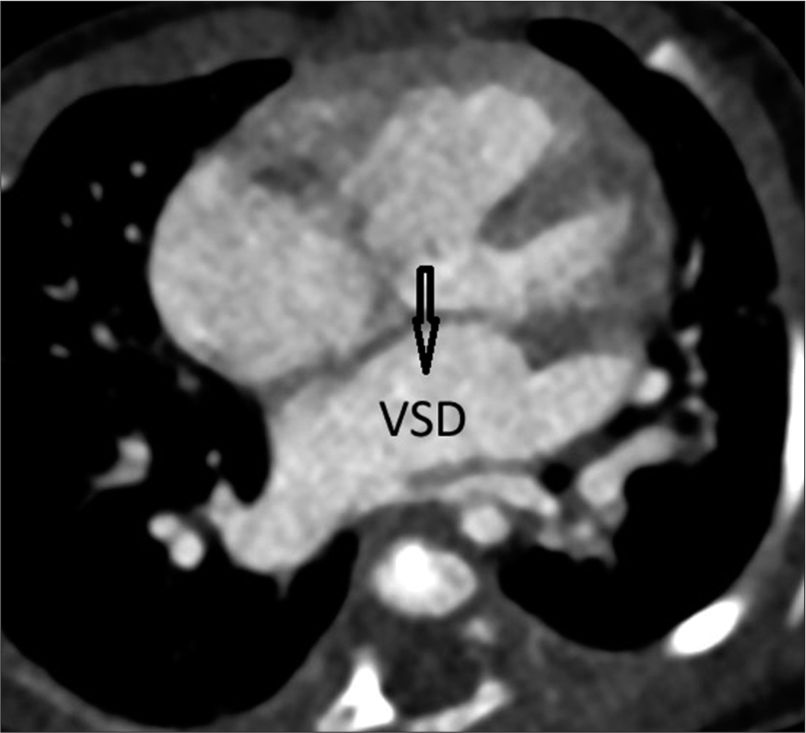
- Axial view of contrast-enhanced computed tomography scan showing ventricular septal defect (VSD). Arrow shows the position of VSD.
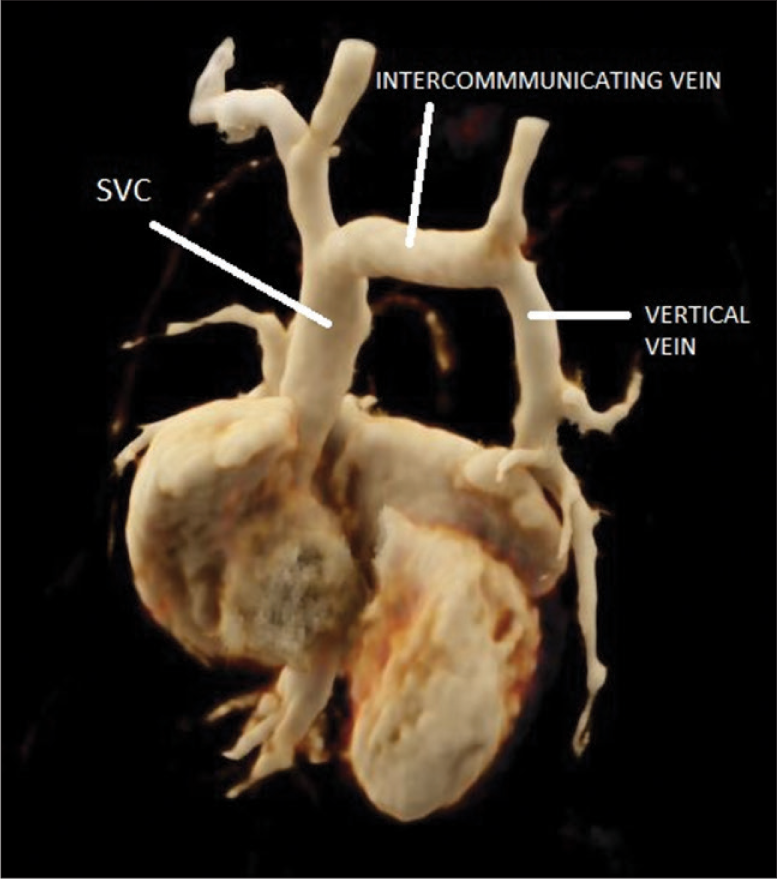
- 3D reconstruction image showing superior vena cava (SVC), intercommunicating vein and vertical vein, left superior pulmonary vein drains into vertical vein, intercommunicating vein, and SVC. Arrows depict SVC, Innominate vein and Vertical vein.
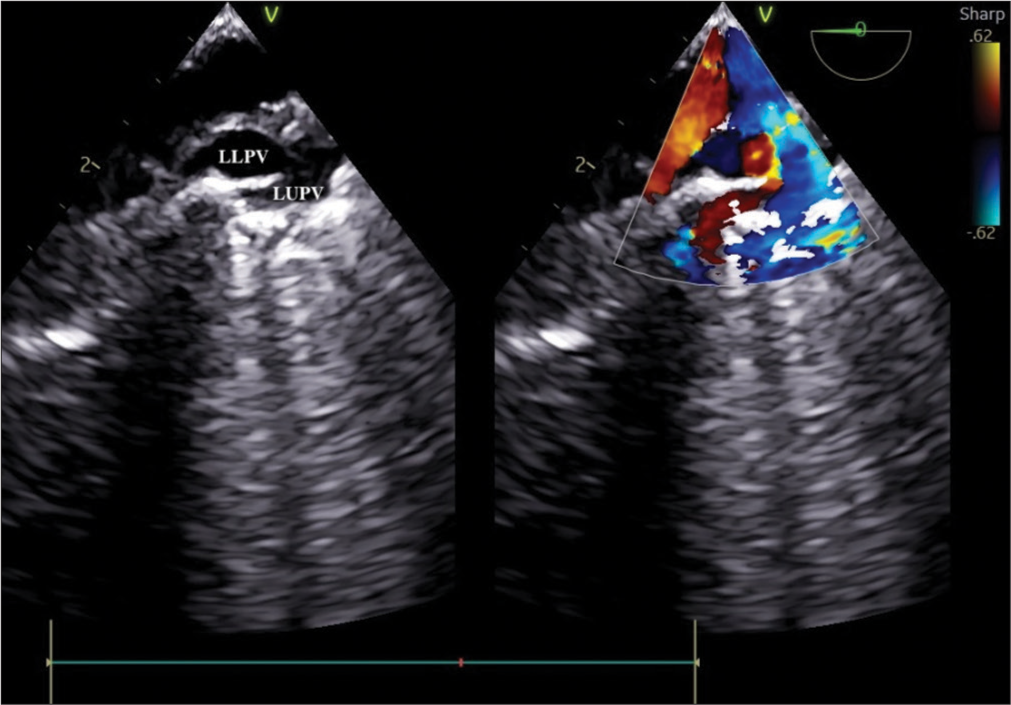
- Modified mid esophageal view focusing on pulmonary veins (PVs) demonstrated anomalous drainage of the left upper PV to innominate vein.
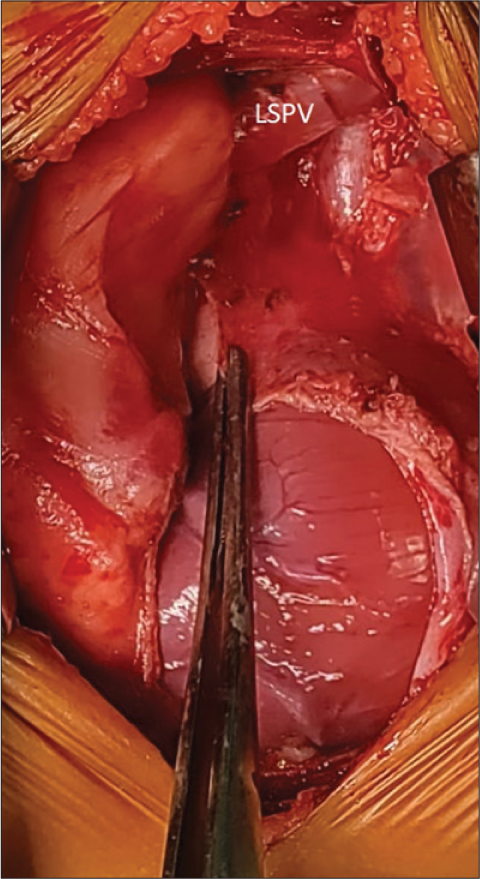
- Left superior pulmonary vein (LSPV) seen draining into innominate vein. LSPV is seen at extrapleural and extrapericardial locations.
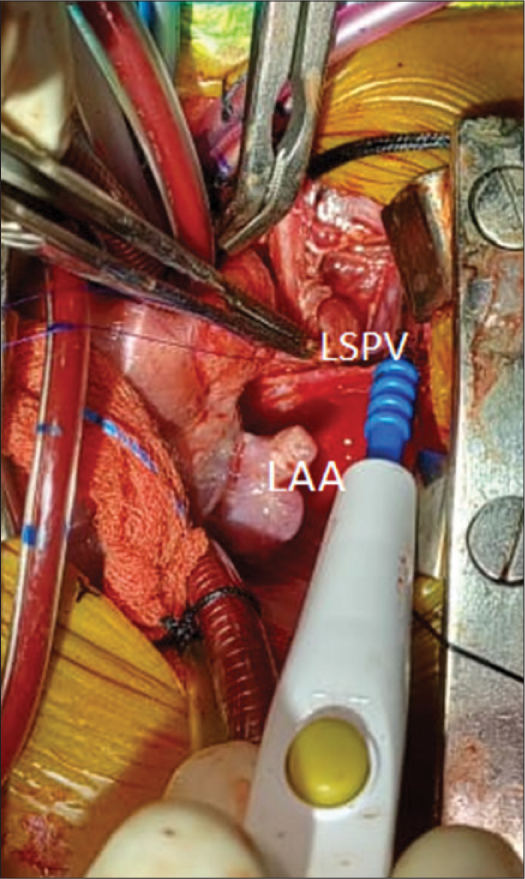
- Left superior pulmonary vein (LSPV) and left atrial appendage (LAA) are exposed and LSPV is anastomosed to LAA. LSPV at innominate vein side is ligated.
On transesophageal echocardiography (TEE) before the procedure, there was no ASD, upper muscular VSD of size 5 mm (left to right shunt) gradient (45/23 mm Hg), right-sided PVs drains into the left atrium (LA) and left-sided lower PV drains into LA, but the flow is turbulent at the site of insertion to LA. Pre-procedure systolic pressure is 65/30 mm Hg, pulmonary artery pressure is 50/25 mm hg, post-procedure systolic blood pressure is 69/30 mm Hg, and pulmonary artery pressure is 28/13 mm Hg. Post-procedure TEE showed no intracardiac shunt post procedure TEE also showed left upper pulmonary vein draining into left atrial appendage [Figure 6].
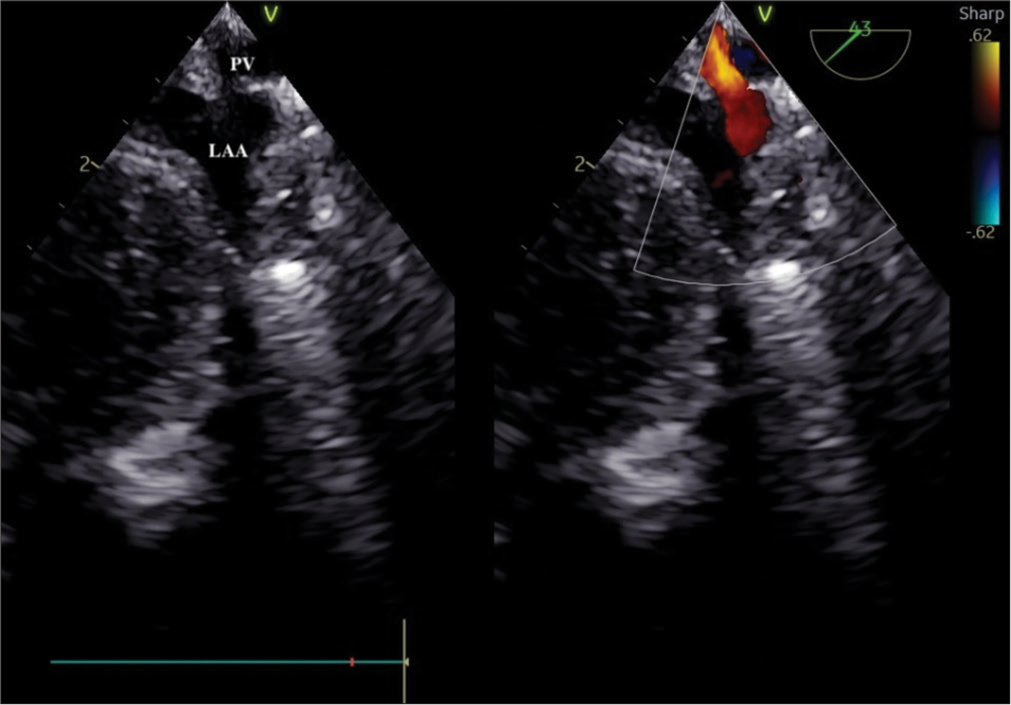
- Mid esophageal left atrial appendage (LAA) view illustrating drainage of pulmonary vein to LAA.
The baby was shifted to the intensive care unit post-procedure on dobutamine ten microgram/kg/min and nitro-glycerine one microgram/kg/min infusion. The baby was extubated on the second postoperative day. The baby had an uneventful post-operative period.
DISCUSSION
In a heart with normal anatomy, four PVs drain into LA.[4] In the case of PAPVC, few PVs drain abnormally into RA or into SVC. In the case of PAPVC, it is unusual to see more than one vein draining into RA. It needs expertise to diagnose the condition on echocardiography, improper diagnosis is made in 25% of cases.[5] Further studies are needed to evaluate the patterns of drainage in cases of PAPVC.
It is seen that 0.4–0.7% of cases are diagnosed as PAPVC in an autopsy series.[2,6] The true incidence could still be lower as many of these cases were asymptomatic. In three-quarters of patients diagnosed with asplenia syndrome, one case of PAPVC is diagnosed.[7] Usually, the right-sided PVs drain into RA,[2] but, in this case, LSPV is seen draining into an innominate vein. It is ten times more common to observe a case of PAPVC with the right side PV draining abnormally. PAPVC is associated with ASD in 90% of cases.[2] It is very rare to see an abnormally draining left PV associated with an intact atrial septum.[8]
Incidentally detected cardiac murmur would bring the child to the cardiologist, or else a child with PAPVC is usually asymptomatic.[5] Right ventricle volume overload or pulmonary vascular obstructive disease would be the pathology leading to the onset of symptoms in adults. The appearance of symptoms in PAPVC depends on the degree of mixing and the presence or absence of left to right shunt.[9,10] Rhythm disturbance would be noted in routine clinical visits, failure to thrive or repeated lower respiratory tract infections could be presenting complaints,[11,12] tachypnea and subcoastal retractions could also be noted[6] in a patient with PAPVC. Stridor could be present on auscultation.[11] Severe pulmonary edema with hypoxemia and cyanosis would be signs when not treated in the initial stage.[7]
Imaging methods used to diagnose a case of PAPVC include chest radiograph, echo cardiogram, cardiac CT, and cardiac magnetic resonance imaging (MRI). Prominent RA and right ventricle with dilated PVs are observed on chest radiography in the case of PAPVC.[6,12] On echocardiography, color flow mapping shows PVs opening into RA or SVC, turbulence is noted in the blood flow in SVC, and there is associated tricuspid regurgitation in some cases of PAPVC.[5,12] The Role of structural MRI in cases of PAPVC has changed over the years, it has become the procedure of choice for diagnosis of PAPVC.[5,13] In a few cases, echocardiography cannot exactly diagnose the drainage of all four PVs. Cardiac catheterization might be needed to confirm the diagnosis in such cases. PAPVC could be associated with other congenital cardiac anomalies [Table 1].
| Author | Contribution |
|---|---|
| Iwasa et al. | A report was submitted of a case with VSD, ASD, and pulmonary venous stenosis |
| Kim et al. | Reported a rare case in which child had coarctation of Aorta along with PAPVC, ASD, and VSD |
| Oh et al. | Submitted case report of a rare case in which child has isolated PAPVC without either ASD or VSD |
PAPVC: Partial anomalous pulmonary venous connection, ASDL: Atrial septal defect, SVC: Superior vena cava, RSPV: Right superior pulmonary vein, VSD: Ventricular septal defect
The treatment of choice for PAPVC is surgical repair.[12,14] Pre-school age is the ideal time to perform surgery on a child with PAPVC.[12] The technique of repair depends on the number and size of anomalous veins. The Warden technique or modified Warden technique is most commonly used for PAPVC repair.[15] PAPVC is usually associated with ASD; in a few cases, PAPVC could be an isolated condition without any mixing of blood. PAPVC can also present with associated ASD, VSD and pulmonary stenosis.[16,17]
CONCLUSION
PAPVC is associated with ASD in most of the cases. However, in the case of VSD with the right ventricular volume overload and turbulent flow in SVC, associated PAPVC should be considered and treated accordingly. Proper diagnosis in the initial setting can allow to prevent redo procedures in these pediatric patients. In cases of VSD, the echocardiologist might not look for PAPVC. PAPVC on the right side is more common, but we report a case of LSPV draining into the left brachiocephalic with an upper muscular VSD.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Tetralogy of Fallot, Absent Pulmonary Valve, Partial Anomalous Pulmonary Venous Return and Coarctation of the Aorta. Int J Cardiol. 1995;52:203-6.
- [CrossRef] [PubMed] [Google Scholar]
- Partial Anomalous Pulmonary Venous Return. Mil Med. 2008;173:523-4.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical Management of Coarctation of the Aorta with a Ventricular Septal Defect and Coexisting Partial Anomalous Pulmonary Venous Connection: A Case Report. Korean J Thorac Cardiovasc Surg. 2006;39:479-81.
- [Google Scholar]
- Prenatal Diagnosis of Partial Anomalous Pulmonary Venous Connection by Detection of Dilatation of Superior Vena Cava in Hypoplastic Left Heart. A Case Report. Fetal Diagn Ther. 2002;17:298-301.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of Partial Anomalous Pulmonary Venous Connection by Magnetic Resonance Imaging. Pediatr Cardiol. 2005;26:490-1.
- [CrossRef] [PubMed] [Google Scholar]
- Persistent Lung Shadow in an Infant with Ventricular Septal Defect and Partial Anomalous Pulmonary Venous Connection Associated with Pulmonary Venous Obstruction. Pediatr Int. 2008;50:397-9.
- [CrossRef] [PubMed] [Google Scholar]
- Concentric Placement of Stents to Relieve an Obstructed Anomalous Pulmonary Venous Connection. Cathet Cardiovasc Diagn. 1997;42:201-4.
- [CrossRef] [Google Scholar]
- Left Partial Anomalous Pulmonary Venous Connection Found during a Lobectomy for Lung Cancer: Report of a Case. Surg Today. 1995;25:982-3.
- [CrossRef] [PubMed] [Google Scholar]
- Partial Anomalous Pulmonary Venous Return In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, eds. Nelson Textbook of Pediatrics (18th ed). Philadelphia, PA: Saunders; 2007. p. :1886.
- [Google Scholar]
- Partial and Total Anomalous Pulmonary Venous Connection in the Fetus: Two-dimensional and Doppler Echocardiographic Findings. Ultrasound Obstet Gynecol. 2003;22:257-63.
- [CrossRef] [PubMed] [Google Scholar]
- Association of a Cor Triatriatum Sinister and a Right Partial Anomalous Pulmonary Venous Return. A Case Report. Acta Chir Belg. 2005;105:217-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary Venous Return Anomaly. 2003. Orphanet Encyclopedia. Available from: http://www.orpha.net/data/patho/gb/uk-pvra.pdf [Last accessed on 2011 Aug 01]
- [Google Scholar]
- Complex Venous Anomalies: Magnetic Resonance Imaging Findings in a 5-Year-old Boy. Surg Radiol Anat. 2006;28:534-8.
- [CrossRef] [PubMed] [Google Scholar]
- An Unusual Presentation of an Atrial Septal Defect. J Cardiovasc Ultrasound. 2009;17:151-2.
- [CrossRef] [PubMed] [Google Scholar]
- Partially Anomalous Pulmonary Venous Connection: Demonstration of Dual Drainage Allowing Nonsurgical Correction. Cathet Cardiovasc Diagn. 1998;44:330-5.
- [CrossRef] [Google Scholar]
- Partial Anomalous Pulmonary Venous Connection to the Superior Vena Cava. Ann Thorac Surg. 2006;82:978-82.
- [CrossRef] [PubMed] [Google Scholar]
- Partial Anomalous Pulmonary Venous Return into Coronary Sinus with Intact Atrial Septum. J Korean Soc Echocardiogr. 2004;12:94-6.
- [CrossRef] [Google Scholar]






