Translate this page into:
Intensive Care Unit Setup for COVID-19
Muralidhar Kanchi, MD, FIACTA, FICA, MBA, FASE Department of Cardiac Anaesthesia and Critical Care, Narayana Hrudayalaya Institute of Allied Health Sciences #258/A, Bommasandra Industrial Area, Anekal Taluk, Bangalore 560 099, Karnataka India kanchirulestheworld@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The coronavirus pandemic has become a challenge to all the healthcare systems in the world. Urgent creation of an intensive care unit (ICU) for the same is the need of the hour. The ideal ICU for COVID -19 should be isolated, fully equipped with invasive and noninvasive monitoring, with 24/7 trained medical personnel, nursing staff and laboratory support. As the coronavirus infection is transmitted by droplets and is highly contagious, protection of healthcare workers is crucial. Personnel working inside the ICU should get personal protective equipment (PPE). Strict guidelines for donning and doffing of PPE should be followed to prevent cross-contamination. Respiratory failure being the commonest complication of COVID-19, knowing the ventilator management for the same is essential. It is of great importance to meticulously manage all the resources to combat this contagion.
Keywords
COVID-19
intensive care unit
personal protective equipment
ventilatory management
Introduction
We are in middle of the corona virus disease-2019 (COVID-19) pandemic that has spread far and wide across the globe. The causative agent is SARS-COV-2, an enveloped RNA corona virus. Corona viruses are broadly distributed among humans, other mammals, and birds. COVID-19 is a global health concern, considering the rapidity with which it has spread around the world, and also demonstrating high-transmissibility. The pandemic broke out from Wuhan in central China late last year, and has now spread relentlessly across the world. The mortality continues to rise, disrupting everyday life, and may portend an economic disaster. According to the World Health Organization (WHO), COVID-19 pandemic is the “defining global health crisis of our time,” capable of revealing the best and the worst in humanity. On March 22, 2020, Indian Prime Minister Mr. Narendra Modi highlighted the scale of the challenge, when he alluded to the fact that even the two world wars did not affect as many countries in comparison to this pandemic. Corona viruses belong to a family of viruses with the spike proteins on the surface–generating the appearance of a crown. Six corona virus species are known to cause human disease. Four viruses, 229E, OC43, NL63, and HKU1are widely prevalent and typically cause mild disease, including the common cold in immunocompetent subjects.
The primary mode of COVID-19 transmission is through respiratory droplets generated when an infected person coughs, sneezes, or talks. Droplets that settle on the eyes, nose, or mouth of a person in close proximity leads to the transmission of infection. Preventive measures to reduce the transmission of the infection include (a) frequent handwashing with soap and water. Soap is extremely effective, as it dissolves the fat membrane of the coronavirus, causing it to “fall apart like a house of cards,” (b) avoidance of touching the face with contaminated hands, (c) maintenance of a safe distance of at least 6 feet away from an infected person to avoid droplet infection, (d) avoidance of touching contaminated surfaces, including metal, glass, or plastic that act as fomites, which may remain infective for several days, and (d) avoiding communal gatherings and, preferably, working from home. Management of critically ill patients with respiratory failure is the need of the hour; setting up an intensive care unit (ICU) on an emergency basis is a challenge. Care should be taken during planning to prevent the spread of infection to other patients and healthcare workers (HCWs). The availability of personal protective equipment (PPE) needs to be ensured, and training should be imparted to HCWs regarding donning and doffing of PPE. The importance of hand hygiene needs to be emphasized. In this article, we focus on how to set up a dedicated “COVID-19 ICU” within a short time frame and elaborate on crucial measures aimed at infection control.
Setting Up an ICU for COVID-19
The ICU is staffed and equipped to care for critically ill patients. Infection control, staff protection, and isolation/quarantine are the three key factors that are crucial in the management of patients with COVID-19. Amongst patients diagnosed with COVID-19, 20 to 30 % require hospitalization and 5 to 11% may require ICU treatment.1
An ideal COVID-19 ICU should be physically separate from other patient care areas. There should be a separate entry and exit with a dedicated lift or ramp. Every bed in a COVID-19 ICU should have two oxygen outlets, one air outlet, two suction outlets, and 12 or more electrical points.1 The ICU should be equipped with adequate monitoring facilities. Ventilators should have the provision for closed suction and heat–moisture exchangers (HME) with viral filtration capability. The ideal COVID-19 ICU should have dedicated defibrillators, portable X-ray machines, ultrasound, electrocardiography (ECG), and echocardiography machines to prevent cross-contamination. Intubation aids including masks, airways, endotracheal tubes, tracheostomy tubes, laryngoscopes, video laryngoscope, fiber-optic bronchoscope, bougie, and Magill forceps should be available. Besides, the facility for organ support such as renal replacement therapy (RRT) and extracorporeal membrane oxygenation (ECMO) may be advisable. Multiple infusion pumps, intravenous sets and cannulae, syringes, central venous pressure (CVP) and arterial lines, nasogastric tubes, and urinary catheters should be available. A ready supply of medications, IV fluids, and a 24-hour blood bank is mandatory. The COVID-19 ICU should be equipped with efficient laboratory support and expert nursing care round the clock. Separate air handling unit with high-efficiency particulate air (HEPA) filters and inflow of low-velocity sterile air with 30 to 60% relative humidity is recommended. Each cubicle should have at least six air changes per hour, of which two should be fresh air.
Aerosol generation with a high-viral load may occur with COVID-19; hence, negatively pressurized rooms are advisable if aerosol-generating procedures are planned. Multiple exhaust fans should be installed if a makeshift ICU needs to be established on an urgent basis in the absence of negative pressure isolation rooms.
Personal Protective Equipment (PPE)
WHO recommends the rationale use of PPE for HCWs who are involved in the care of COVID-19 patients2 PPE includes gloves, medical masks, respirators or N95 masks, face shields or goggles, leg covers, and gowns. As COVID-19 is transmitted through close contacts and droplets, preventive and mitigation measures are of prime importance. PPE is part of a package of administrative controls, including appropriate infrastructure, clear infection control and prevention policies, appropriate triage, and adequate staff-to-patient ratios. Environmental and engineering controls includes maintenance of a social distance of at least 1 meter and adequately well-ventilated isolation rooms for confirmed COVID-19 cases as described in WHO’s infection prevention and control of epidemic and pandemic-prone acute respiratory infections in healthcare.3
As the current supply of PPE is limited, the WHO has recommended strategies to optimize the availability of PPE, including minimization of the need for PPE through evaluation of suspected cases of COVID-19 by telemedicine.4 Physical barriers including glass or plastic windows may be used to separate HCWs and patients. The use of PPE must be rational and appropriate. HCWs directly involved with the care of COVID-19 patients should wear gowns, gloves, medical masks, and eye protection. For potential aerosol-generating procedures including cardiopulmonary resuscitation (CPR), endotracheal intubation and tracheostomy, N95 respirators or equivalent and level 3 PPE should be used. Extended use of respirators for not more than 4 hours is advised when PPE is short in supply while caring for different patients with the same diagnosis.5, 6, 7, 8 Guidelines for donning and doffing PPE at Narayana Health City, Bangalore, is described in the article by Dr. Vijay Richard.9
Human Resource Management
Optimum and judicious utilization of human resources is of utmost importance because of the limited availability and risk of infection. A team leader is of paramount importance, and closed-loop communication of all the team members with the leader is crucial. The following is the standard operating procedure for reallocation of residents, postgraduates and nursing students as part of the hospital management plan for COVID-19 recommended by the Ministry of Health and Family Welfare, Government of India.10
The hospital may be divided into three broad zones including (i) non-COVID area, (ii) COVID area caring for patients with mild-to-moderate illness and (iii) critical area including the ICU. In Besides, a triage area needs must be earmarked to evaluate patients who present with acute severe respiratory illness.
Residents and postgraduate students will be categorized as follows:
Category A: core departments (departments of anesthesiology and critical care, medicine, pulmonary medicine, geriatric medicine, and emergency medicine). Category B: clinical specialties already running ICU or high-dependency units (HDUs) under their care (medical specialties–departments of cardiology, gastroenterology, neurology, nephrology, pediatrics, medical oncology, and hematology; surgical specialties–departments of gastrointestinal [GI] surgery, neurosurgery, cardiothoracic and vascular surgery, ENT, and pediatric surgery). Category C: other specialties with clinical postgraduates, but not running ICUs/HDUs under their care (medical specialties–departments of endocrinology, rheumatology, obstetrics and gynecology, radiotherapy, and radiation oncology; surgical specialties–departments of orthopedics, urology). Category D: clinical specialties with limited or no responsibility for critically ill patients (departments of dermatology, ophthalmology, physical medicine and rehabilitation, psychiatry, community medicine, and transfusion medicine). Category E: medically trained, MBBS residents from preclinical and paraclinical departments (departments of anatomy, physiology, biochemistry, biophysics, pathology, microbiology, forensic medicine, pharmacology, laboratory medicine, nuclear medicine, and radiodiagnosis). Category F: interns
Facilities will be categorized based on the characteristics of the patients who are present at each location, and management decisions are implemented accordingly. In brief, three levels of healthcare facilities are envisaged, namely, level A: screening areas; level B: facility for hospitalized patients who are in a stable clinical condition; level C: facility for critically ill, hospitalized patients.
The team constitution for each level of the healthcare facility is as follows: level A (screening area)–team leader from B or C category of resident; teams to include residents primarily from C, D, and F categories; level B (facility for hospitalized patients who are in a stable clinical condition)–team leader from A or B; teams to include residents primarily from C and D categories; level C (facility for critically ill hospitalized patients); residents only from category A and B to be allocated to this area. It has also been decided that category E residents can be posted at any level of health facility, primarily for coordination activities. It is pertinent to note that roles and responsibilities must delineated by the team leaders or supervising faculty at each level.
The total number of individuals required in each team/shift, and the duration of a shift (depending on the need to wear PPE), will be decided by the COVID-19 task force and the faculty-in-charge for various levels of facilities. The total number of individuals per team can be modified based on patient load and the proportion of critically ill patients. It is, however, suggested that the numbers may be computed after initial experience and serve as a template for future planning.
Shift timing duration maybe adjusted based on the ease of travel. The internal working arrangements during a shift maybe at the discretion of the faculty-in-charge, accounting for the time taken for donning and doffing PPE. The total duration for which an individual maybe allocated to a facility should be adjusted to prevent burnout. This duration can be varied according to the level of the facility.
Training of Residents
It is also important to ensure adequate communication with the team that provides training and the COVID-19 task force which is responsible for the deployment of residents. Residents should not be posted to any COVID-19 facility without undergoing an essential training module conducted by the hospital infection control team. Additional training must be provided at the facility where the resident is allocated, based on the levels of the facility. For instance, if there are two locations where screening takes place, the content of the facility level training must be the same, although delivered by different team leaders at different locations. This will ensure training all key aspects, irrespective of the site of delivery and trainer. This requires that the coordination by the faculties who supervise these facilities will need to coordinate to ensure a uniform level of training. Training on COVID-19 and clinical evaluation of patients should also be provided for residents, especially those from departments with no regular patient-care activity (pre- and paraclinical departments). Optional training must be offered to residents from departments that have limited engagement with sick patients. These modules are developed by the COVID-19 task force. The inclusion of psychologists may be considered part of the training, to enhance the motivation of participating residents.
Faculty Deployment
The same general principles, according to the department involved (based on clinical exposure and participation in the management of critically ill patients) and the level of the facility, should be used for deployment of faculty for this purpose. Private hospitals and medical colleges may also follow identical guidelines.
Nursing student allocation to handle workforce shortage for COVID-19: India is facing an unprecedented public health emergency with the COVID-19 pandemic affecting several parts of the nation. The number of COVID 19 patients are increasing with the requirement for adequate workforce to handle the surge of cases. If the need arises, nursing students may be recruited to handle the crisis, based on their level of skills and training (Fig. 1).
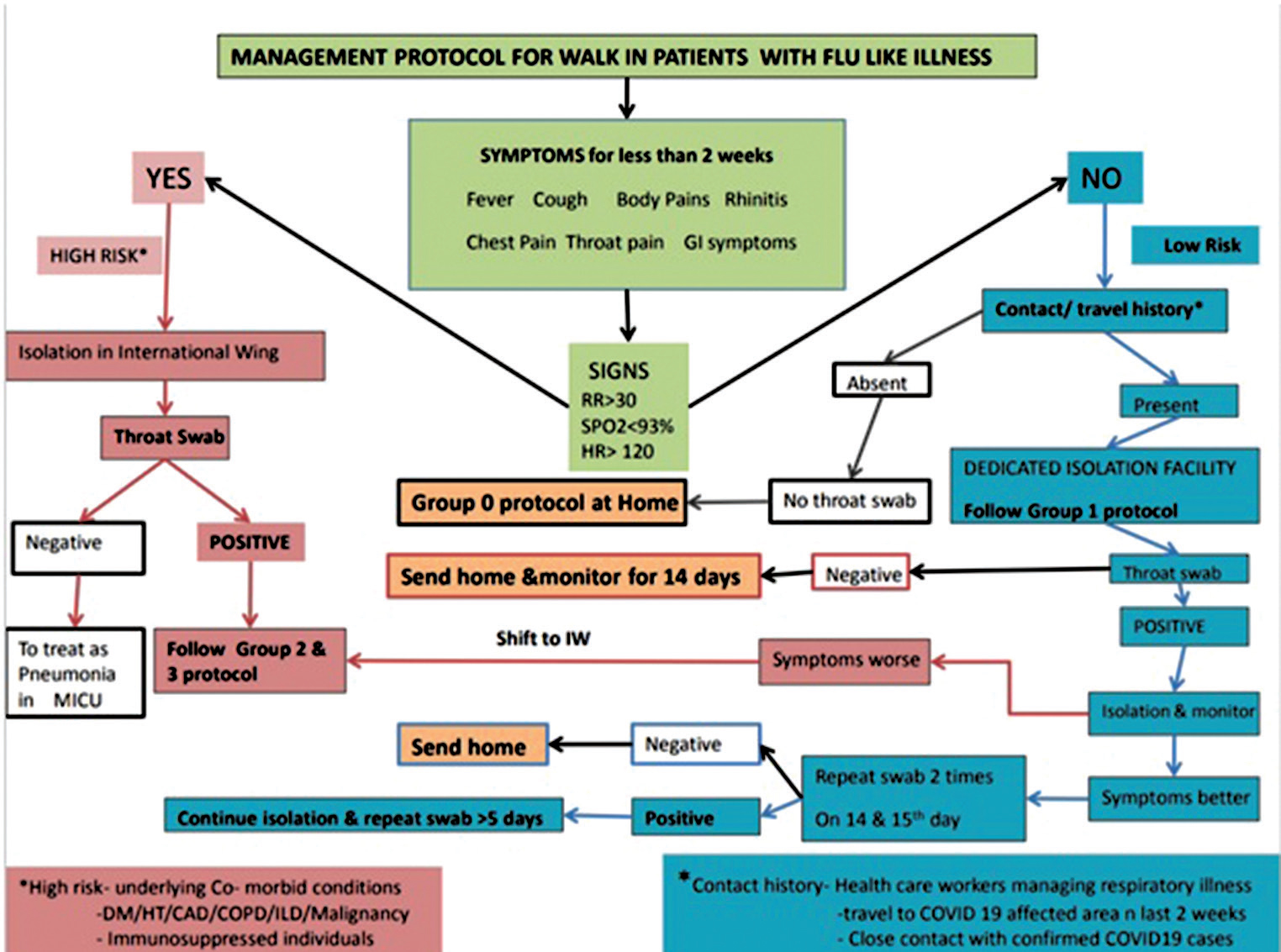
- Management protocol for walk-in patients with flu-like illness.
Case Definition of COVID-19
Mild disease: Symptoms of upper respiratory tract infection and fever with no breathlessness/no hypoxia, and hemodynamically stable.
Moderate disease: if any one of the following is present: respiratory rate (RR) >24/min or SpO2 ≤ 93% on room air. Bilateral opacities on chest radiograph or CT scan.
Severe disease: features of moderate disease plus any one of the following: SpO2 < 90%, PaO2/FiO2 < 300 mm Hg; confusion/drowsiness; systolic blood pressure < 90 mm Hg or diastolic blood pressure < 60 mm Hg, chest radiograph or CT scan showing bilateral opacities not fully explained by effusion/lung collapse/nodules. Worsening of underlying illness in the past 1 week despite adequate management.
Classification of Disease
Group 0: Mild disease/no risk for COVID-19/throat/nasopharyngeal swab not performed.
Group 1: (a) Group 1x–mild disease/report awaited; (b) Group 1a–mild disease/report negative; and (c) Group 1b–mild disease/report positive
Group 2: (a) Group 2x–moderate disease/report awaited; (b) Group 2a–moderate disease/report negative; and (c) Group 2b–moderate disease/report positive
Group 3: (a) Group 3x–severe disease/report awaited; (b) Group 3a–severe disease/report negative; and (c) Group 3b–Severe disease/ report positive
Management Protocol for COVID-19
Group 0
Investigations: No investigations are performed unless recommended by the COVID-19 physician treatment–desloratidine 5 mg once daily orally or levocetrizine 5 mg once daily orally, paracetamol 650 mg (15 mg/kg/dose) in case of fever > 100°F/body pain. Salt water gargle thrice a day. Consultation by physician or pulmonologist in case of clinical deterioration.
Group 1
Investigations: No investigations to be performed unless recommended by COVID-19 physician treatment–oseltamivir 75 mg twice daily orally for 5 days; azithromycin 500 mg once daily, orally for 3 days, desloratidine 5 mg or levocetrizine 5 mg once daily, orally and paracetamol 650 mg (15 mg/kg/dose) orally if fever > 100°F/ body pain/ headache; salt water gargle four times a day.
Group 2
Routine investigations: complete blood count, C-reactive protein, renal and liver function tests, procalcitonin level, blood culture, serum ferritin level, arterial blood gas analysis, chest radiograph, ECG, 2D echocardiography, urine routine and culture. Optional: creatine kinase (CK), CK-MB, troponin-I, and brain natriuretic peptide (BNP), as recommended by the COVID physician or cardiologist.
Treatment: supportive–oxygen therapy via nasal prongs/mask, titrated to achieve SpO2 > 93%; IV antibiotics if bacterial infection is suspected. Ceftriaxone 1 g IV 12 hourly or co-amoxiclav 1.2 g IV 8 hourly (may be modified based on culture reports); desloratidine 5 mg orally or levocetrizine 5 mg orally, once daily. Metered dose inhalers: ipratropium 20 mcg + levosalbutamol 100 mcg) two puffs 8 hourly and budesonide (200 mcg, one puff 12 hourly through spacer)
COVID-19 specific therapy: hydroxychloroquine (HCQ) 400 mg orally, twice daily on day 1, followed by 200 mg twice daily for 5 days; oseltamivir 75 mg twice daily, orally, for 5 days. HCQ may be withdrawn once the COVID-19 test report is negative.
Group 3
Investigations: routine investigations–complete blood count, C-reactive protein, renal and liver function tests, procalcitonin level, blood culture, serum ferritin level, arterial blood gas analysis, chest radiograph, ECG, 2D echocardiography, urine routine and culture.
Treatment: supportive–oxygen therapy and ventilatory management according to the ICU team; oseltamivir 75 mg twice daily for 5 days; IV antibiotics if bacterial infection is suspected; ceftriaxone 1 g IV 12 hourly or co-amoxiclav 1.2 g IV 8 hourly (may be modified based on culture reports); desloratidine 5 mg or levocetrizine 5 mg orally, once daily. Metered dose inhalers: ipratropium 20 mcg + levosalbutamol 100 mcg 2 puffs 8 hourly and budesonide 200 mcg, one puff 12 hourly through spacer
COVID-19 specific: HCQ 400 mg orally, twice daily on day 1, followed by 200 mg twice daily for 5 days; oseltamivir 75 mg twice daily, orally, for 5 days.
Critical Care Management of COVID-19 Patient
Moderate disease (mild tyachypnea rate around 24–26/min, Sp02 <94% on room air, P/F ratio 200–300 mm Hg): start oxygen with face mask at 6 to 10 l/min. Observe over 1h if tachypnea worsens/SpO2 not maintained/falls considering high-flow nasal cannula (HFNC) after ruling out underlying (a) altered mental status (b) hypercarbia on arterial blood gases (ABG), (c) hypotension (SBp < 90 mm Hg, DBp < 60 mm Hg), and (d) multiorgan failure
HFNC: modifications to HFNC use; specific to COVID-19: (i) flow should be limited to 30 L/min to prevent aerosol generation, (ii) patient’s airway should be covered with N95 mask. Keep a close watch on clinical scenario and repeat ABG after 1h on HFNC.
Endotracheal intubation and mechanical ventilation must be considered in case of (i) worsening tachypnea/paradoxical breathing, (ii) increasing FiO2 requirements, (iii) altered sensorium, (iv) hypotension, and (v) hypercarbia on ABG at 1 h from initiation of HFNC.
Ventilatory Management of COVID-19 Patient
Patients with severe disease should be intubated and mechanically ventilated.
-
Endotracheal intubation should be performed by a trained and experienced provider using aerosol precautions. Patients with ARDS, especially young children or those who are obese or pregnant, may desaturate quickly during intubation. Preoxygenate with 100% FiO2 for 5 minutes via a face mask with reservoir bag, bag-valve mask, and HFNO. Rapid sequence intubation is appropriate after an airway assessment that identifies no signs of difficult intubation. In patients with severe acute respiratory distress syndrome (ARDS), prone ventilation for > 16 hours per day is recommended. All patients after intubation should be connected to appropriate bacterial and viral filter (one attached to endotracheal tube and second at end of expiratory circuit connecting to ventilator) to prevent dissemination of virus into the atmosphere.
Procedure for initial ventilator settings: (i) adjust the tidal volume (Vt) to a maximum of 4 to 8 mL/kg ideal body weight. For volume modes, simply adjust the set or target Vt, and for pressure modes, adjust the peak pressure to achieve initial Vt; (ii) adjust the set RR based on PaCO2 levels; (iii) permissive hypercapnia can be allowed with target pH of 7.2; (iv) set the initial positive end expiratory pressure (PEEP) to maintain the SpO2 within 88 to 92%; (v) after changes have been completed, check the plateau pressure (Pplat). If the Pplat is > 30 cm H2O and driving pressure (Pplat minus PEEP) is >15 cm H2O, decrease the Vt by 1 mL/kg increments until the Pplat is less than or equal to 30 cm H2O or driving pressure < 15 cm H2O (minimum Vt = 4 ml/kg); (vi) recruitment maneuvers (RMs) may be used if necessary, delivered as episodic periods of high continuous positive airway pressure (CPAP) (30–40 cm H2O); and (vii) in patients with moderate-to-severe ARDS (PaO2/FiO2 <150), neuromuscular blockade by continuous infusion can be used to prevent ventilator desynchrony.
Special Situations in COVID 19
Cardiac Arrest
Chest compressions and intubation subjects HCWs to a high-risk of aerosol exposure. Proper use of PPE should be adhered to while minimizing the number of personnel to three to four during code management. Use of an automated compression device should be considered to minimize exposure.11 Code responders should don full PPE prior to entering the patient area. The team includes a code leader, code registered nurse, anesthesiologist, and an extra person for performing chest compressions.
Circulation: Until a definitive airway is obtained, compression-only CPR should be performed. Multiple studies have shown that compression-only CPR is noninferior to standard CPR.12 If the patient has a shockable rhythm (VF/VT), defibrillate as soon as possible.
Airway: Prior to securing a definitive airway, oxygen should be applied via a nonrebreather mask at 15 L/min without humidification. Avoid bag mask ventilation (BMV) ventilation, high-flow nasal cannula, and noninvasive ventilation (CPAP, BiPAP) to minimize aerosolized virus.13 If passive oxygen is not available, place a surgical face-mask and a blanket over the patient’s face prior to chest compressions. If the patient does not have a shockable rhythm, proceed with rapid sequence intubation as early as possible to limit aerosolization.
Endotracheal intubation: Endotracheal intubation is the procedure that subjects the rescuer to the highest risk of infection during resuscitation. To maximize the success rate of intubation, airway interventions should be performed by experienced individuals, and chest compressions should be stopped. This may deviate from usual cardiac arrest care, leading to a pause in chest compressions; however, this is acceptable to maintain the safety of code responders.13
Chest compressions should resume once the endotracheal tube (ETT) cuff is inflated, and it is connected to the ventilator. If the pause in chest compressions is excessive and endotracheal intubation does not seem likely, consider laryngeal mask airway or other supraglottic airway device.3 Code responders other than the one who is intubating should distance themselves from the head of the bed during the intubation procedure (6 ft distance).4 Continuous capnography should be used to monitor ventilation.
Etiologies to Consider
Data from a retrospective study in Wuhan revealed the cause of death to be as follows14:
-
Respiratory failure (53%).
-
Heart failure with respiratory failure (33%).
-
Myocardial damage (7%).
-
Unknown cause (7%).
It is important to attempt to identify and treat reversible causes (5H’s, 5T’s) before stopping the code.
Terminating Resuscitative Efforts
-
Avoid prolonged resuscitation if there is no easily reversible etiology identified.
-
No one factor alone, or in combination, is predictive of outcome during cardiac arrest; however, it is reasonable to stop resuscitation efforts if return of spontaneous circulation (ROSC) has not been achieved within 30 minutes.
-
In intubated patients, failure to achieve an ETCO2 of greater than 10 mm Hg by waveform capnography after 20 minutes of CPR should be considered as one component of a multimodal approach to decide when to end resuscitative efforts.15
Postresuscitation Care
-
Dispose of, or clean, all equipment used during CPR. Any work surfaces used for airway/resuscitation equipment will also need to be cleaned.
-
After the resuscitation has ended, adhere to strict doffing procedure to limit exposure.
-
If ROSC is achieved, provide usual postresuscitation care consistent with current recommended guidelines, including targeted temperature management.16
In summary, when setting up an ICU specific to the needs of the COVID-19, the following must be considered:
-
Personal protective equipment: In view of shortage of PPE, consideration is given to usage of PPE beyond the manufacturer’s designated shelf life. Training of medical personnel must include junior physicians, nurses, physiotherapists, other technical and housekeeping staff. Correct methods of donning and doffing of the PPE must be inculcated for all these medical personnel (please see above). Contact surface decontamination of medical equipment is necessary. Cell phones may be banned inside the COVID-19 ICU, and if cell phones are permitted, disposable polythene bags should cover the cell phones, and this disposable polythene bag must be discarded at the end of the shift. Restrict and limit the number of visitors and visiting time of the family members: it is preferable to use video conferencing methods for the patient family to react with the patient if the patient is conscious in the ICU
-
ICU infrastructure capacity building: If there is a surging number of critically ill patients, increasing the ICU capacity is needed. The ICU care may be provided in HDUs outside the ICU, and special ward beds may be converted into a semi-ICU for moderately sick patients. This also calls for attention to logistics and supply chains to maintain all essential components of care. Elective surgery must be postponed.
-
ICU staffing: Increase in the ICU bed numbers should proportionately increase the number of staff working in the ICU. The hospital staff may be augmented from the noncritical areas with appropriate short-term training programs. Staff need to be educated about critical care in a short time and such personnel should receive clear communication about the limitation of shift hours, provision of rest areas and psychological support. A scheme of utilization of medical personnel as proposed by the Government of Karnataka is highlighted above.
-
ICU triage is an essential component of prioritizing patients for intensive care. Patients who are young with prognostically good outcome must be given priority over patients who are elderly with multiple comorbidities
-
ICU research: Prompt conduct and sharing of information through communication and publications is necessary but when analyzing and interpreting the published literature, caution must be needed because some of these literature may be published in haste and the applicability must be tailored to the needs of the particular institution.
Acknowledgment
The guidelines of resident and postgraduate student allocation is adapted from Ministry of Health and Family welfare recommendations. We gratefully acknowledge this.
Conflict of Interest
None.
References
- Rapid Creation of COVID 19 ICU. Available at: https://youtu.be/y8gYvRcPdhQ. Accessed May 21, 2020
- Rational Use Of Personal Protective Equipment (PPE) For Corona Virus Disease (COVID-19). Available at: https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf. Accessed May 21, 2020
- WHO. In: Infection Prevention and Control of Epidemic-and Pandemic-Prone Acute Respiratory Infections in Health Care. Geneva: World Health Organization; 2014.
- [Google Scholar]
- WHO. In: Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth. Geneva: World Health Organization; 2009.
- [Google Scholar]
- Evaluation of respiratory protection programs and practices in California hospitals during the 2009-2010 H1N1 influenza pandemic. Am J Infect Control. 2013;41(11):1024-1031.
- [Google Scholar]
- Criteria for the collection of useful respirator performance data in the workplace. J Occup Environ Hyg. 2014;11(4):218-226.
- [Google Scholar]
- Workplace protection factors for an N95 filtering facepiece respirator. J Occup Environ Hyg. 2007;4(9):698-707.
- [Google Scholar]
- A practical guide to a safe sequence of donning and doffing of personal protective equipment in relation to COVID-19. J Card Crit Care. ;4(1):xx-xxx.
- [Google Scholar]
- Ministry of Health and Family Welfare, Government of India. SOP for reallocation of residents/PG students and nursing student as part of hospital management of COVID. Available at: https://www.mohfw.gov.in/pdf/COVID19SOPfordoctorsandnurses.pdf. Accessed June 6, 2020
- Arrest C. Brigham and Women’s Hospital COVID-19 Clinical Guidelines: Cardiac Arrest. Available at: https://COVIDprotocols.org/protocol/08-cardiac-arrest. Accessed May 21, 2020
- Compression-only CPR or standard CPR in out-of-hospital cardiac arrest. N Engl J Med. 2010;363(5):434-442.
- [Google Scholar]
- Staff safety during emergency airway management for COVID-19 in Hong Kong. Lancet Respir Med. 2020;8(4):e19.
- [Google Scholar]
- Ruan Q. Song, J. Clinical Predictors of mortality due to COVID-19 Based on an Analysis of Data of 150 Patients from Wuhan, China. Intensive Care Medicine. Available at: https://link.springer.com/article/10.1007/s00134-020-05991-x?fbclid=lwAR1EbkrPza14lwx-dNFQDrlYG2HRomm-8Lb7NEvWZlqP1Gff8EBDaLmL7Ig. Accessed May 21, 2020
- Part 3: Ethical issues: American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18)(02):S383-S396.
- [Google Scholar]
- Part 8: post cardiac arrest care. American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18)(02):S465-S482.
- [Google Scholar]






