Translate this page into:
Infographics in TIVA
Tushar M. Chokshi, MD Department of Anesthesia, Sterling Hospital Vadodara, Gujarat India Chokshitushar@hotmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Infographics are a new way of visually communicating information in a colorful and concise manner. They are becoming very popular in medical field since the last decade. Through infographics, one can understand the subjects through text, graphics, and images. Total intravenous anesthesia (TIVA) is a technique of general anesthesia (GA) given via intravenous (IV) route exclusively. In perspective of infographics, TIVA is far more understandable through its simple format. TIVA is also more advantageous than inhalational anesthesia. It avoids the deleterious effects of immunosuppressant and lacks any respiratory irritation, thus providing a good alternative anesthesia technique. Many peripheral surgeries can be done with the patient breathing spontaneously without any airway device, thus avoiding airway instrumentation, leading to droplet and aerosol generation. IV agents can be utilized to provide sedation during regional anesthesia (RA), which can easily be escalated to contain pain due to sparing of blocks or receding neuraxial anesthesia. The present narrative review focuses on the infographics in TIVA technique, providing highlights pertaining to its importance.
Keywords
anesthesia
infographics
total intravenous anesthesia (TIVA)
Introduction
Infographics are an innovative and engaging method of visually communicating information in a colorful and concise manner. In infographics, the representation of information is in the graphic format, and it is a combination of text, images, and narration.1 These are the main features of infographics. Sometimes, they are used to overcome language barriers which enhance our understanding and ability to make decisions. To make infographics, first identify the audience for your infographics and accordingly collect your content and relevant data. After choosing your desired infographics template, prepare your template in accordance with PowerPoint and customize. Finally, add your logo and publish it. Good infographics should be concise and visually appealing, providing value and interest to your readers. Your infographics should be accurate, creative and transparent, citing data sources. Be mindful of the copyright of your infographics. So, successful infographics are well-designed, easy to understand, and tell a good story; their visual aspects are snackable too (Fig. 1).2
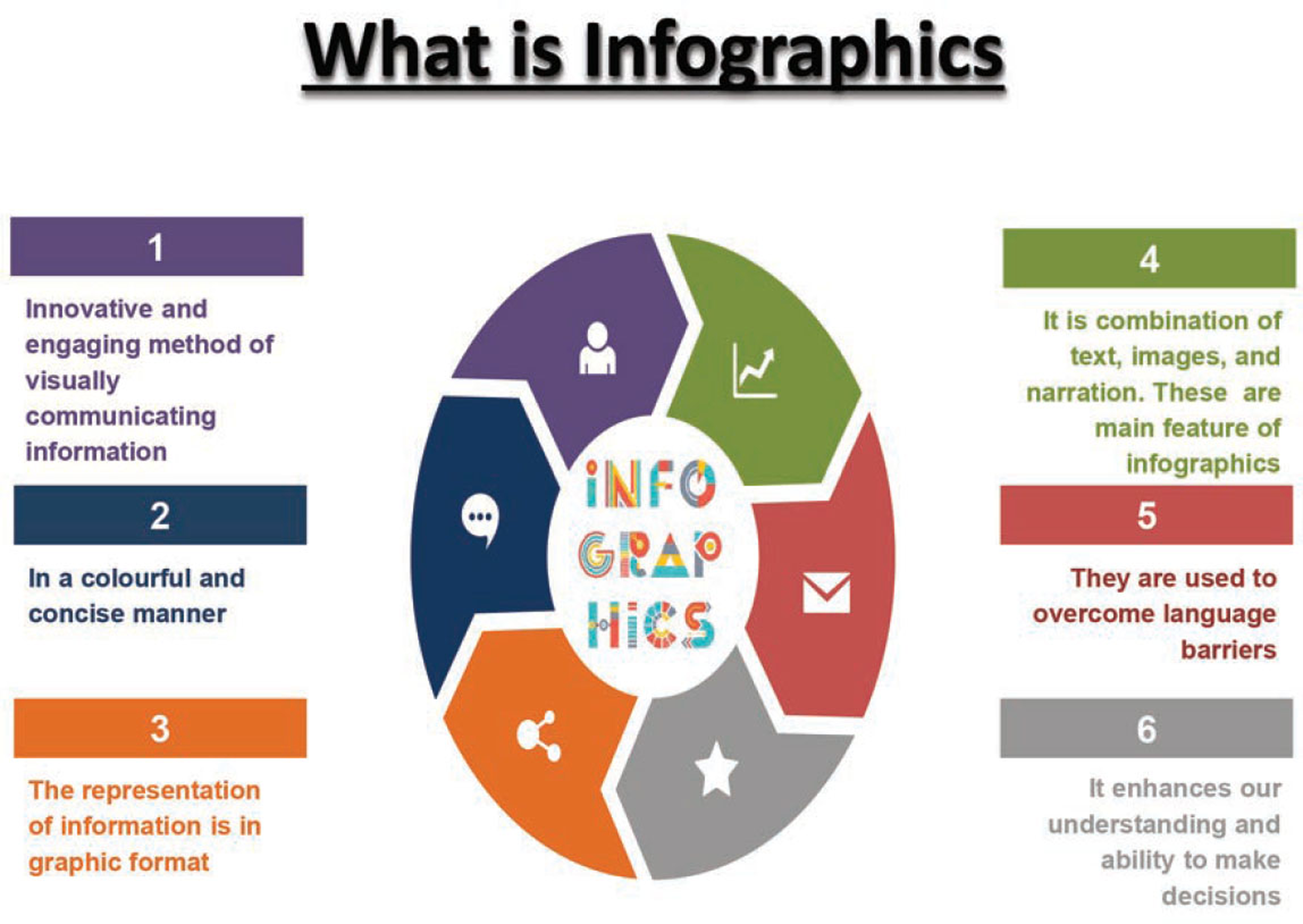
- What is infographics?
Search Strategies
Keeping these words (Anesthesia; Infographics Ketamine; Etomidate; Propofol;; total intravenous anesthesia [TIVA]) as the main keys, either single or in various combinations, a systematic search was made on the Internet, exploring various databases including Pub Med, Cochrane Databases of Systematic Reviews, Scopus, EMBASE, Google, and Google Scholar from the year 1990 to 2020. The references of relevant articles were cross-checked and the review was imbibed from the articles which elaborated on these keywords
Why Infographics in Medical Field?
Had there been no infographics, interpreting and conveying complex data and information would not have been so easy. Infographics are such a powerful communication medium, that not only IT sector, but unusual sectors like medical sector have also adopted infographics. And why is that? Because it can magically transform intricate information for doctors or patients into interesting graphics that are engaging and easy to comprehend. As we all know, medical information can often be difficult for a layperson to understand, and doctors can easily interpret this complex information to them through engaging infographics.3
Benefits of Infographics in Medical Field
Doctors and patients get to see the bigger picture and a picture is worth a thousand words. One focuses more on information that is visually stimulating and offers a visual guide through infographics. They are highly customizable and exceptionally shareable. And finally, it improves health literacy.3
Why Infographics in TIVA?
Easy to understand, readily available charts through infographics of TIVA is better understandable.
Definition of TIVA
It is a technique of general anesthesia which uses a combination of agents given exclusively through the IV route without the use of inhalation agents (gas anesthesia) including nitrous oxide, but oxygen, compressed air or helium are exceptions.4
Why TIVA is Becoming Popular?
TIVA is becoming popular because gas leads to side effects in the form of aerosol and droplets. We are conducting surgeries daily, and being frontline captain in OT, we have to provide anesthesia to patients. TIVA is preferred in all planned or emergency surgeries with innovative techniques, drugs, and equipment in any setup. There are certain challenges with the use of inhalational anesthesia and numerous risks and difficulties. Smooth and rapid induction with IV anesthetic agents is always a better alternative.
Types of TIVA
TIVA is with endotracheal tubes (ETT) or without ETT. If without ETT, then with supraglottic devices (SGD) or without SGD. IF without ETT or SGD, then with nasal or oral airways. TIVA may also be without any airway instrumentation (Fig. 2).5
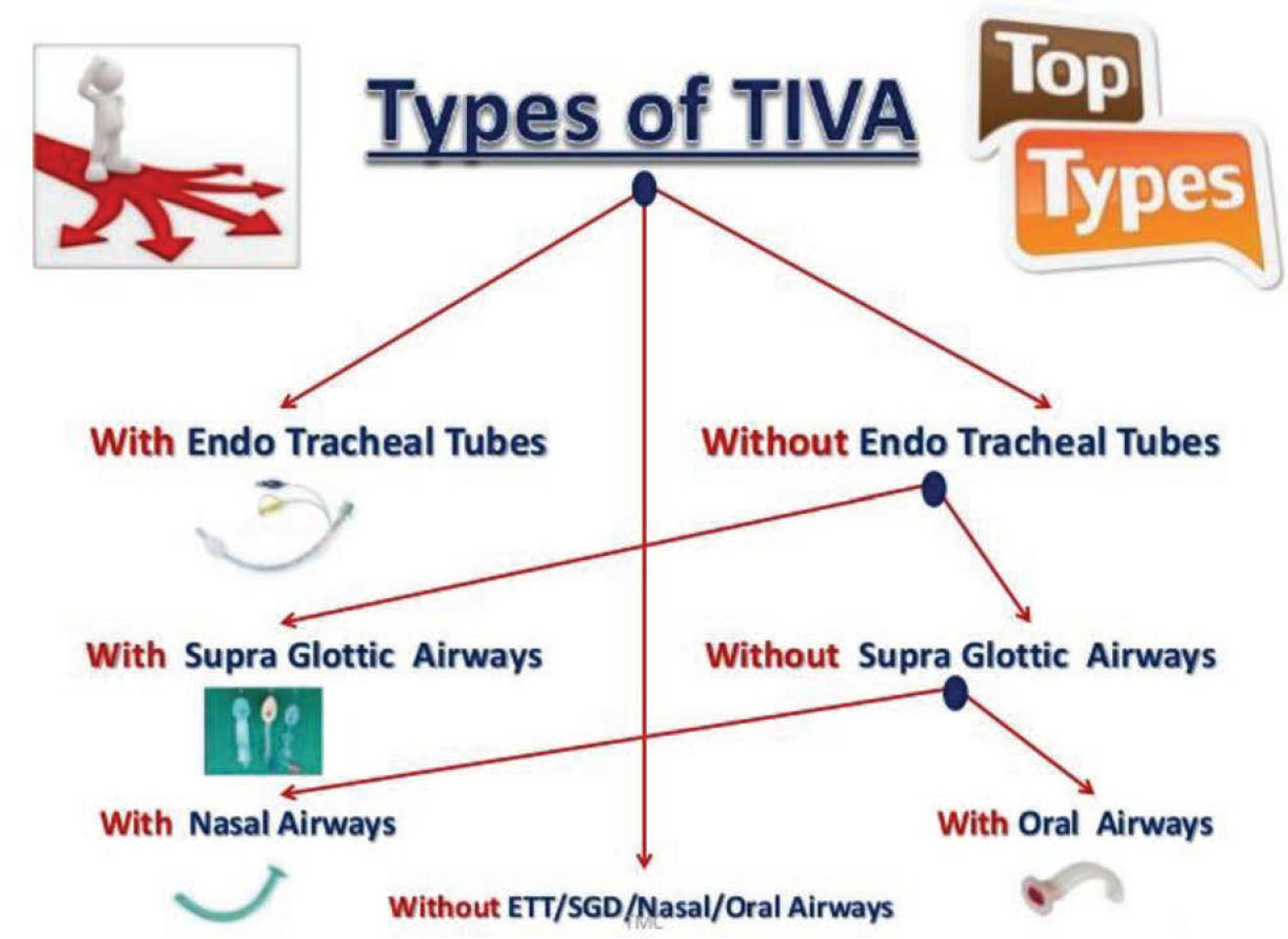
- Types of TIVA.
TIVA Indications
TIVA is indicated almost in all surgical procedures like airway procedures, daycare surgery, neurosurgery & neuromonitoring, nonoperating room anesthesia, and short procedures, for example, CT, MRI, and cardiac catheterization. It is also best choice in postoperative nausea and vomiting (PONV)-risk patients, malignant hyperthermia (MH) susceptible patients, trainee teaching and patient’s choice.6
Advantages of TIVA
Except for a slight prick in the arm, the patient is unaware of having an anesthetic. There is no mask over the face and sudden concentration of gas or vapor. No risk of MH and very low incidence of postoperative delirium. There are less chances of emergence phenomena, and it avoids distension air-filled spaces in the patient’s body, so better operating conditions for surgeons. TIVA gives less operating room pollution. Better preservation of cerebral autoregulation is best in TIVA. Reduced stress response and patients wake up, as if from natural sleep, with less PONV. Finally, there is no smell of volatile agents at all in the room, and the patient is usually most grateful for not having his system saturated with such a drug.7
Disadvantages of TIVA
Possibility of not finding the vein is its first disadvantage. Sometimes, there is pain on injection and injection is irreversible. Disposables may be costly, and incidence of awareness if not given properly, because of not having another apparatus to carry on the TIVA. Environmental effect of plastic waste and risk of bacterial contamination. One should careful with TIVA for shallow respirations. Caution should be exercised in prolonged procedures and in obese patients
TIVA Drugs
Includes all benzodiazepines, all narcotics, propofol, ketamine, etomidate, dexmedetomidine, all muscle relaxants, dexamethasone, magnesium sulfate, lidocaine, nonsteroidal anti-inflammatory drugs (NSAIDs), and beta blockers (Fig. 3).
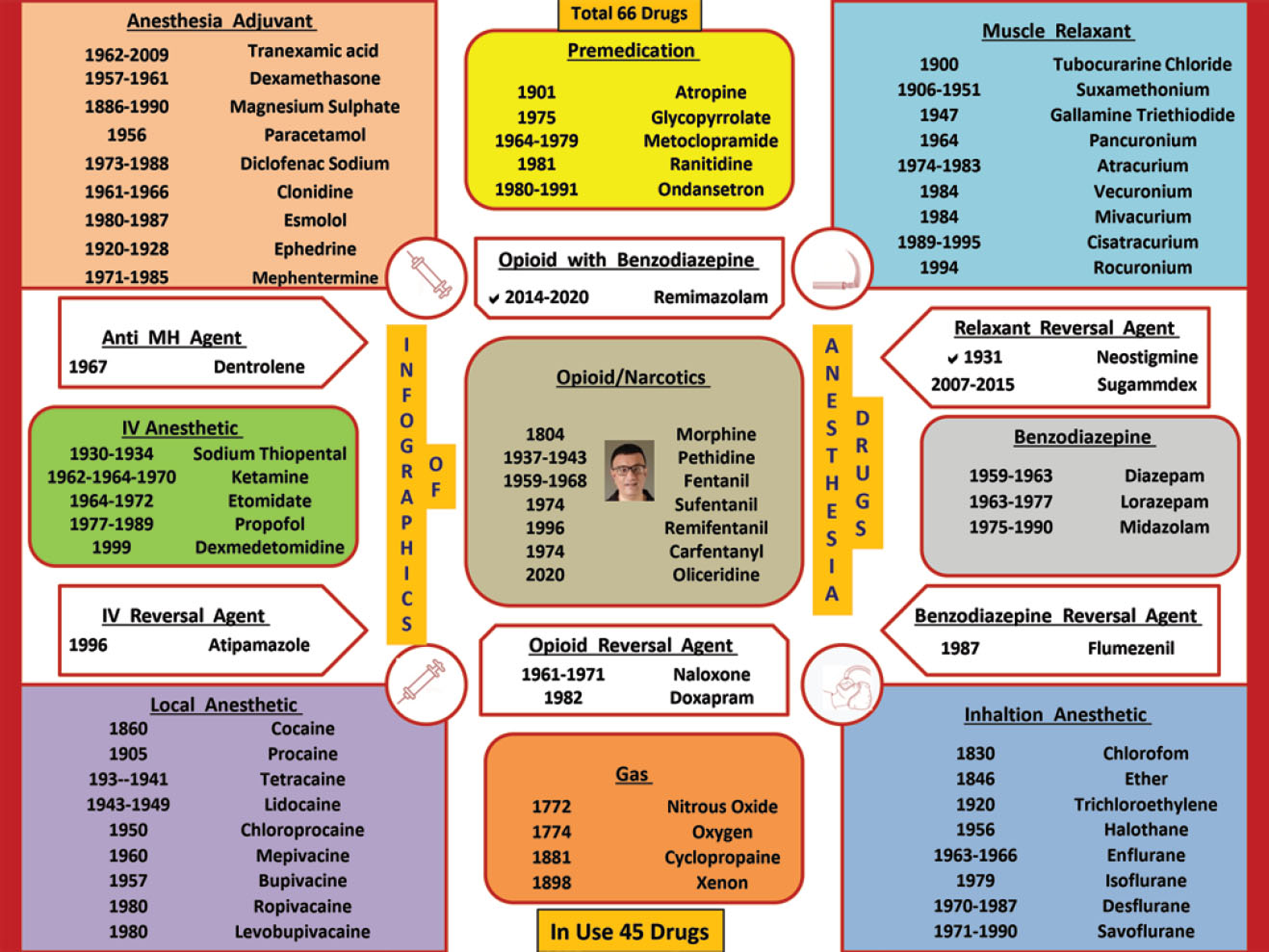
- Infographic of TIVA drugs.
Ideal TIVA Drug
It will be having rapid onset of action, rapid and predictable recovery, and also be stable in any solution. It should be water-soluble to minimize toxicity associated with the solvent and chemically compatible with other drugs. There will not be any perivascular sloughing if extravasated or absorbed by plastics. It will be devoid of adverse side effects and also be low cost. Most importantly, it can be mixed with other anesthetic agents without any complication.
IV Anesthetic Drugs
Ketamine
It is the only IV anesthetic with hypnotic, analgesic, and amnesic properties. It produces rapid hypnosis with profound analgesia and amnesia after IV administration of 0.5 to 2.0 mg/kg. It can be mixed with all types of anesthetic and narcotic agents in single syringe. Ketamine with midazolam (Ketomed), ketamine with propofol (Ketofol), and ketamine with dexmedetomidine (Ketodex/Dexket) are established TIVA mixtures. So, ketamine is very commonly used drug in the TIVA technique (Fig. 4).
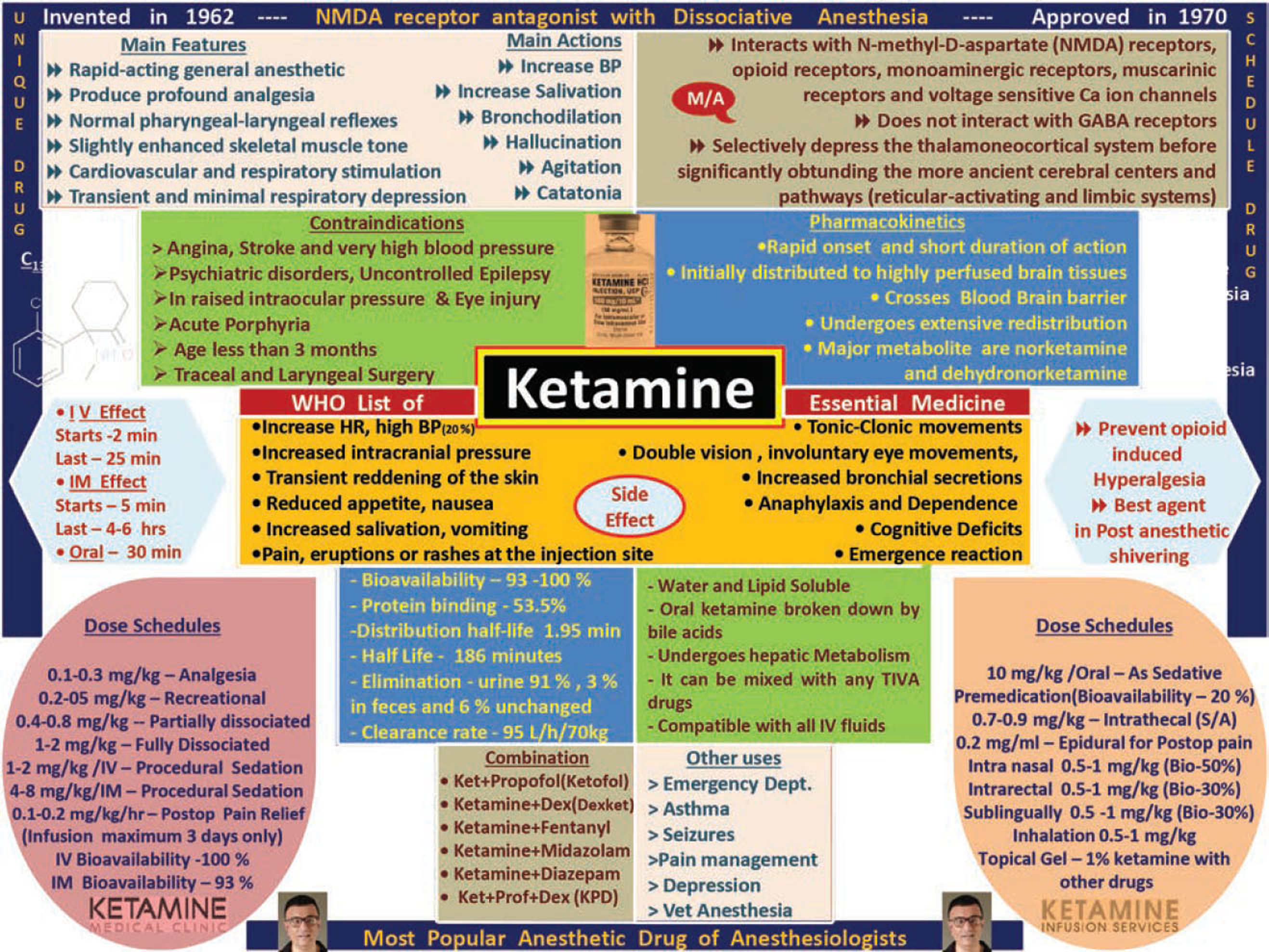
- Infographic of Ketamine.
Propofol
Prime drug in all TIVA combinations. Initially, TIVA dose is 2 to 2.5 mg/kg IV (if used alone), and in TIVA mixture, 1 mg/kg IV. Coadministration of propofol and remifentanil by target-controlled infusion (TCI) is highly effective and constitutes ideal total IV anesthesia (Fig. 5).8
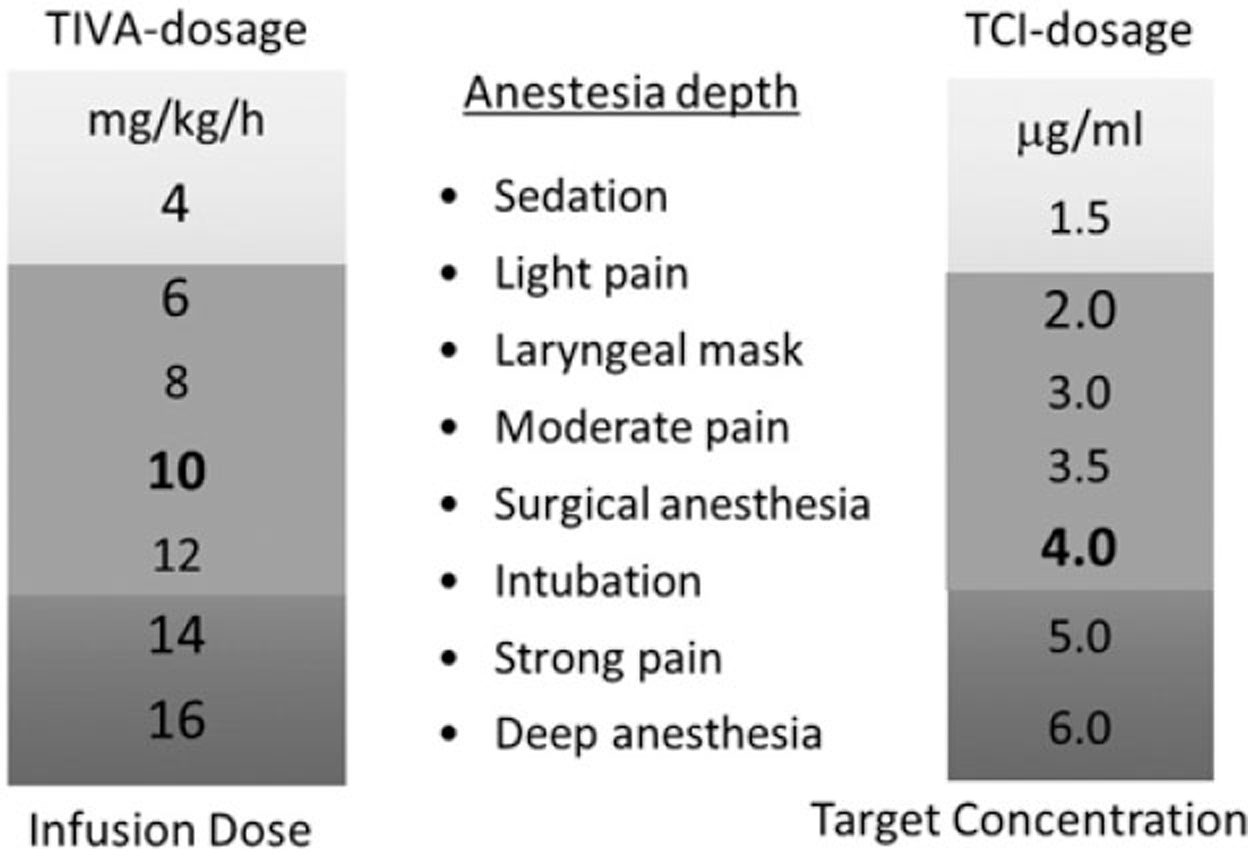
- TIVA Doses of Propofol.
Dexmedetomidine (Dex)
A highly selective α2 agonist, having anxiolytic, sedative, analgesic, and sympatholytic properties with less respiratory depression, make dexmedetomidine a much-preferred drug in TIVA anesthesia. For TIVA, it is advisable to combine other drugs with Dexmedetomidine (Dex) in dose ranges of 0.5 to 1 mcg per kg, according to patient status and surgery needs. Maintenance infusion is generally initiated at 0.6 μ/kg/hour and titrated to achieve desired anesthesia effects. In pediatric TIVA, Dex with ketamine (Ketodex) combination is mostly preferred for endoscopic and radiological procedures (Fig. 6).
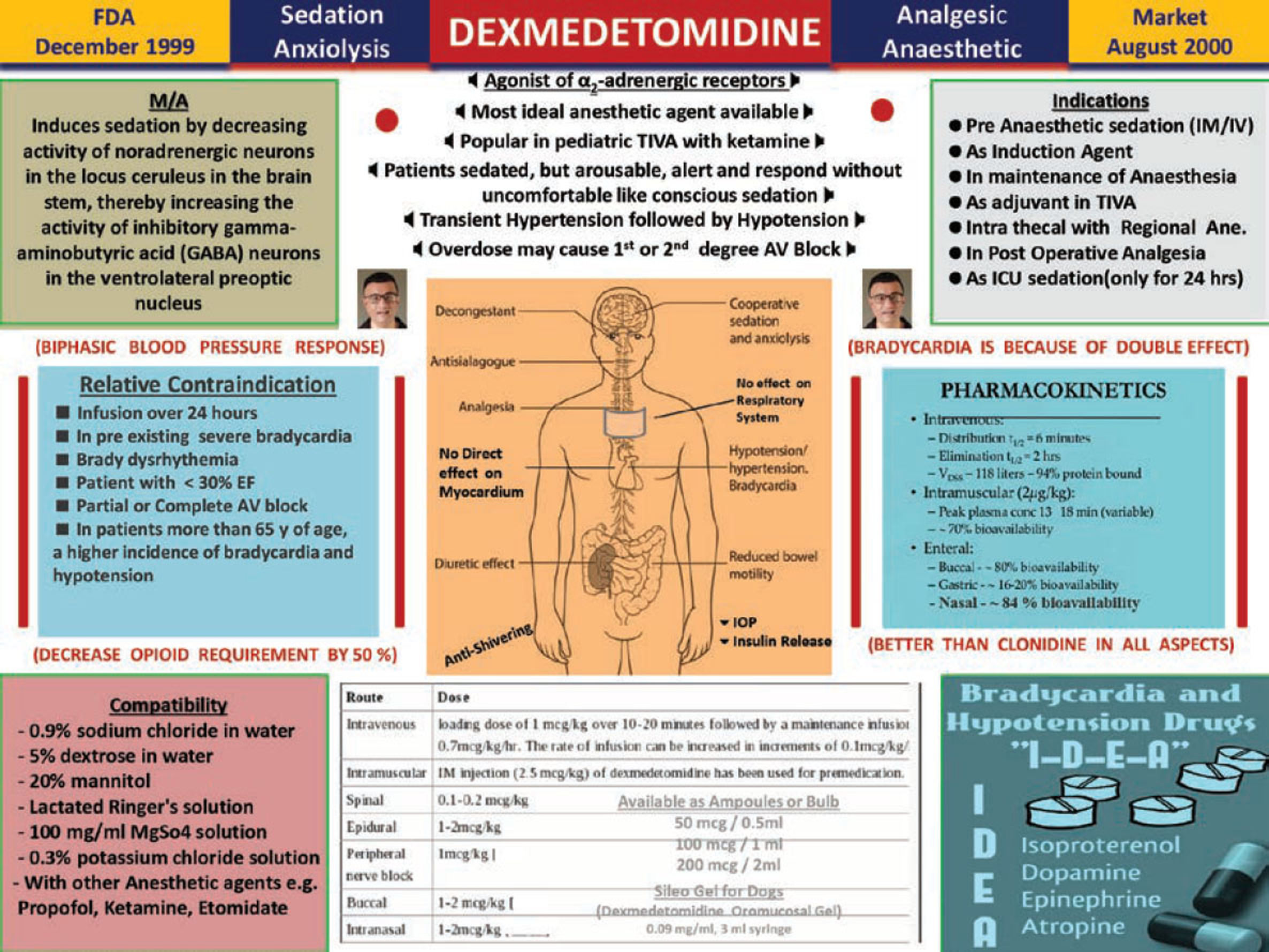
- Infographic of dexmedetomidine.
Fentanyl
It is commonly used opioid in TIVA in bolus 3 μg/kg over 30 seconds, followed by 2 μg/kg/hr for 30 minutes, 1.5 μg/kg/hr from 31 to 150 minutes, and 1 μg/kg/hr until 30 minutes before skin closure.
Remifentanil
Most widely used opioid in world in TCI with propofol. Available as 1 mg/vial, 2 mg/vial, and 5 mg/vial. Its initial dose is 1 mcg/kg. For TIVA maintenance, it is given in dose of 0.25 to 0.5 mcg/kg/min IV, and for postoperative period, 0.025 to 0.2 mcg/kg/min IV.
Midazolam
Coadministration of midazolam in TIVA reduces the induction dose and the total dose of any other anesthetic drug. It is given in dose of 0.05 mg/kg, keeping in mind not to cross total dose more than10 m.
Lidocaine
Bolus dose is 1 to 1.5 mg/kg, infusion as 1.5 mg/kg/hr and as adjuvant in TIVA, reducing the TIVA dose of other anesthetic agents by 10 to 20%
Magnesium Sulfate
As an analgesic adjunct, MgSo4 useful in patients receiving TIVA. It reduces Propofol, Dex, atracurium and postoperative narcotic consumption. Also, it improves the quality of postoperative analgesia during TIVA. Commonly, it is given in bolus dose of 30 to 50 mg/kg with other anesthetic agents, and maintenance dose is 6–10 mg/kg/hr as continuous infusion. It is the most cost-effective drug in TIVA practice (Fig. 7).
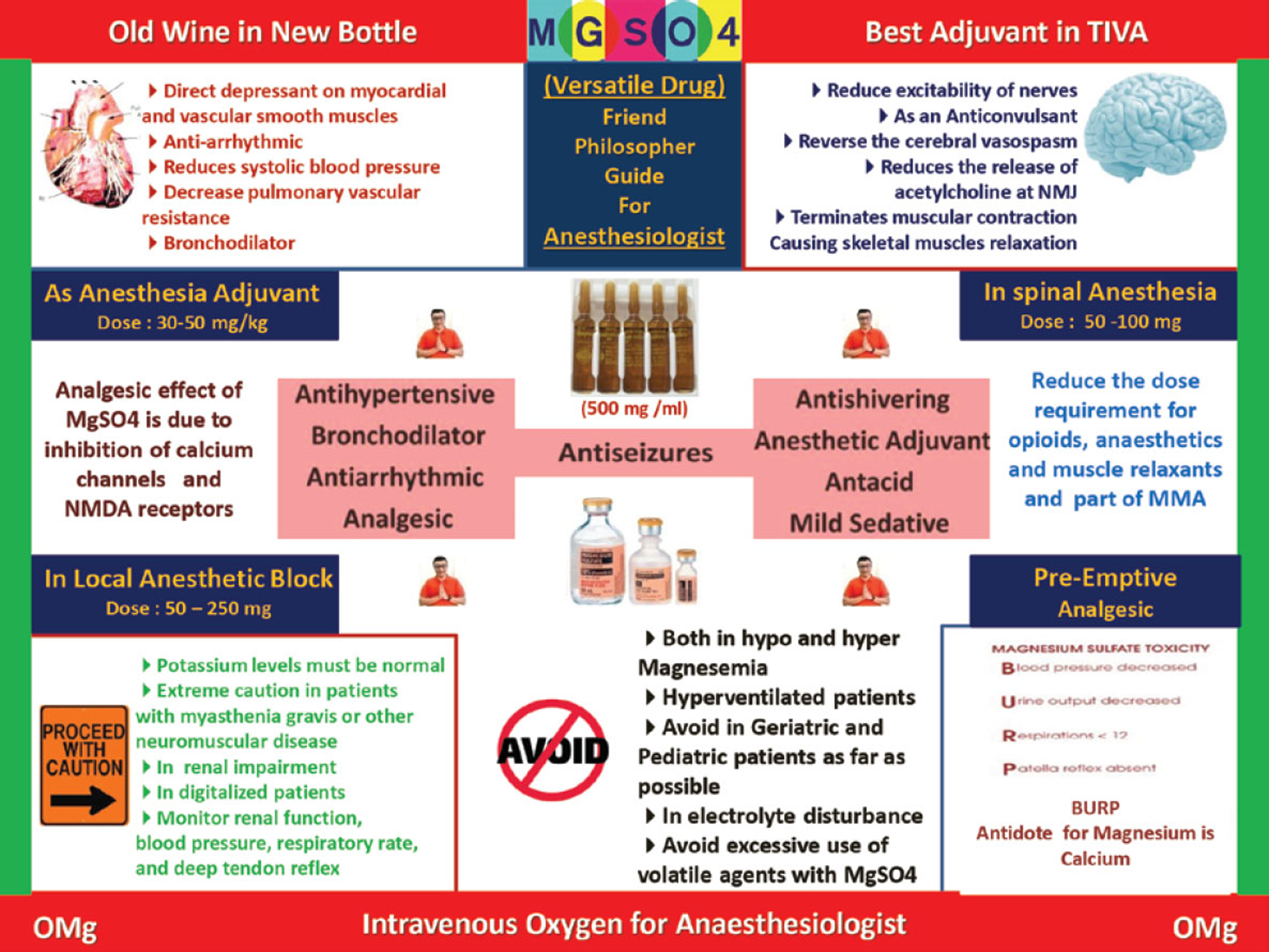
- Infographic of magnesium sulphate.
Dexamethasone
Dexamethasone is used widely in TIVA as an adjuvant. It is an anti-inflammatory agent, prevents and treats PONV, suppresses inflammation, and is a good analgesic agent. It also provides a sense of well-being. In TIVA, it gives good quality of recovery and early discharge of patients; commonly, single prophylactic dose of Dex 8 mg can be given irrespective of sex, disease, or American Society of Anesthesiologists (ASA) risk
TIVA Drug Combinations
Propofol, dexmedetomidine and fentanyl (PDF TIVA), midazolam, dexmedetomidine and fentanyl (MDF TIVA), ketamine, propofol and Dex (KPD TIVA), ketamine and propofol (KETOFOL TIVA), ketamine and Dex (KETODEX/DEXKET TIVA), ketamine and midazolam (KETOMED TIVA), and remifentanil and propofol (RP TIVA), but thumb rule in TIVA with drug mixture is shake well and use within 4 to 6 hours.
Ketofol
First established TIVA combination, physically compatible, chemically stable 1:1 mixture in capped syringe for 3 hours at room temperature with exposure to light. No significant change in pH up to 3 hours with no separation, cracking, color change, or gas formation. This combination is widely used by anesthesiologists across globe.
Ketodex
Combination of ketamine 1mg/kg and Dex 1 mcg /kg and useful in pediatric patients
Ketomed
Combination of ketamine 1mg/kg and midazolam 0.1 mcg /kg. It is useful in outside OT procedures.
KPD TIVA
It is a combination of ketamine, propofol and Dex 1:1:1 dose for TIVA. It will permit lower dose of each individual agent for TIVA and reducing their adverse hemodynamic and respiratory effects, which is very safe and important for patient and anesthesiologist. The advantage is low dose of each agent as compared with full dose, providing excellent analgesia and anesthesia with reduced dose of individual. Also, there is stable hemodynamics, decrease airway complications, and rapid recovery
RP TIVA
Combination of remifentanil and propofol which can be mixed in polypropylene syringes and used for up to 36 hours–remifentanil concentration is 50 mcg/mL (1 mg in 20 mL propofol). Color and clarity good with pH stable at 3.9 to 4. This combination is a very short-acting with adequate analgesia, satisfactory hemodynamic, rapid recovery, shorter postanesthesia care unit (PACU) stay, and excellent patient acceptance. It is an ideal agent for TCI model and most widely used TIVA combination with TCI in the world
Propofol and Fentanyl
Combination of propofol (1% & 2%) with fentanyl(10 & 50 mcg/mL) showed no significant degradation of emulsion within 20 hours. In this, propofol dose reduction happened by 50%
Methods of Giving TIVA
Either with a single drug or with a combination of drugs, by single syringe technique with mixture of drugs or with only one drug, continuous IV infusion through drips, with Syringe infusion pumps, with TCI machines, and automated drug delivery through closed loop systems.6
Single Syringe TIVA (SS TIVA)
It explores the feasibility and conduct of combining IV agents in a single syringe technique to provide balanced anesthesia. No additional investment for TCI or closed loop systems and no need for expertise in it. Simple syringe or pump can be made use of. Only one syringe is used, with the advantage of dose titration at a single level and fixed dose mixtures. Short procedures can be managed with intermittent boluses, without a syringe pump. It can be practiced in low-dependent setups and outside the operating rooms.
Manually Controlled Infusion (MCI)
In this method, there is manual dosing of anesthetic agents during TIVA with fixed infusion rate, which is done by syringes or with IV drips
Target-controlled Infusion (TCI)
A TCI is an infusion controlled to achieve a preset drug concentration in the plasma or the effect site. Key components of TCI infusions are user interface to enter details and target blood concentration and software with pharmacokinetic model, validated for specific drug to control infusion rate. There is communication between control unit and pump hardware. Clinical benefits of TCI are more predictable onset and offset of anesthetic effect with higher stability during maintenance. Advantages are short time to recovery, low incidence of PONV, short time to discharge, economic benefits, and saving nursing time in the recovery room. It also limits the need for antiemetic therapy and allows patients an early return to work
Closed Loop Anesthesia Delivery Systems or Automated TIVA (ATIVA/CLADS)
A closed loop system is the ideal means of automated drug delivery where the input involves drug delivery (propofol, opioids, etc.), output evoked potential, bispectral index (BIS), blood pressure, and pulse rate.
Clinical Benefits of Closed Loop Anesthesia
Automatic delivery of anesthetic drugs to the patient at the time of induction of anesthesia using IV anesthetic agents depend upon the patient’s condition or choice of anesthetist. It frees the anesthetist from the repetitive task of looking at the anesthetic depth and altering the drug delivery manually. Also, it frees the anesthetist’s hands to allow him/her for other activities while keeping a watch on the monitor. The anesthetist is warned of the abnormal rates of drug delivery as well as abnormal response of the patient through visual and audio warning. Fine-tuning of the drug delivery is done according to the requirement of the patient as well as the surgical stimulus requirement. Safety of patient is kept in mind by cutting off anesthetic drug delivery in case of severe drop in blood pressure or heart rate. The anesthetist defines the safety limits of blood pressure as well as heart rate and blood gas levels for not only warning the anesthetist but also stopping delivery of the anesthetic agents. The anesthetist defines the inspired and expired concentrations of anesthetic agent, beyond which the system stops delivery of anesthetic agent.
iControl-RP
It is autorobotic TIVA with remifentanil-propofol, US FDA approved. It was developed in Vancouver at the University of British Columbia in 2015 by a team including Dr. Ansermino (pediatric anesthesiologist) and Dr. Dumont (professor of electrical and computer engineering).
TIVA in Different Groups of Patient
TIVA in Pediatric Patients
Pediatric TIVA can facilitate surgery, reduce airway responsiveness, and minimize complications such as PONV and emergence agitation. Manual infusions remain an important option in clinical practice due to variability of dose regime. Kataria and Paedfusor TCI models are used. The Kataria model is used in children aged 3 to 16 years and weighing 15 to 61 kg, and the Paedfusor model is used in children aged 1 to 16 years and weighing 5 to 61 kg. Propofol, ketamine, remifentanil and Dex play important role in TIVA. For obese children, use the total body weight (TBW) to calculate the dose needed for infusion. Avoid TIVA in neonates as far as possible.9
TIVA in Geriatric Patients
Compared with inhalation anesthesia, TIVA is more suitable, as it has less observable effects on cognitive function in elderly patients after surgery. Comparing with TIVA, inhalational anesthetics may augment complications related with reduced lung blood flow and circulatory depression. Inhalational anesthetic agents may further reduce cardiac output and cause potentially lethal increase in alveolar concentration. Always start with a low concentration/infusion rate and slowly work upward. Go low, go slow and always follow. Most important is to avoid hypotension. Consider IV fluids and vasopressors when appropriate. Multipara monitoring and oxygen is a must during TIVA in geriatric patients
TIVA in ASA III Patients
TIVA can be given to seriously ill patients in whom systemic disease is not a threat to their life (ASA III). There are no specific protocols for TIVA in ASA III patients but dose of TIVA among elderly patients can be adopted, requiring a lower concentration to produce anesthesia. Multipara monitoring and oxygen is must during TIVA in these patients. Choose the most appropriate TIVA drugs according to the patient’s physical condition–whether the patient is elderly or young or whether the patient is obese or non- obese.
TIVA in Obese Patients
TIVA is an excellent method of administering general anesthesia to obese patients. The recommended drug dose in obese patients is always lower than nonobese patients, and the actual blood concentration is higher than the calculated target dose of drugs. The “no-relaxant” technique (for intubation) is not advisable for obese patients, and suxamethonium for intubation in TIVA is ideal choice. In obese patients, always secure airway to avoid respiratory depression with nasal or oral airways. Multipara monitoring and oxygen is a must during TIVA in Obese patients
Surgical Procedures under TIVA
From OT to outside OT (nonoperating room anesthesia [NORA]), from pediatric to geriatric, from any surgical to medical specialty.
TIVA Checklist
All anesthesia drugs, airway equipment, oxygen and multipara monitors are must before giving TIVA. Ensure no leakages from cannula and patient’s IV cannula is always visible during the surgery (if possible). Syringes should be labeled with the drug name, date, and concentration. Infusion lines should be checked every 15 minutes during surgery. The infusion set through which TIVA is delivered should have a Luer-lock connector at each end. If BIS is used, check placement before and after surgical draping. At the end of the case, ensure all tubing/IV cannulae which had TIVA drugs by any method are flushed to prevent inadvertent boluses in the ward.5
TIVA Monitoring
Anesthesiologists are the best monitors. Also, loss of response to shaking and shouting, loss of hemodynamic response or limb movement with vigorous jaw thrusting, and absence of tachycardia or even bradycardia with laryngoscopy and intubation. Other monitors include multipara monitoring, BIS monitor, evoked potentials, and processed electroencephalogram (pEEG) monitor, are recommended when a neuromuscular blocking drug is used with TIVA.5
TIVA Update
TIVA has become more popular, practical, and possible due to two main reasons–First, the advance knowledge of pharmacokinetic and pharmacodynamics properties of drugs such as propofol, ketamine, Dex and newer short-acting opioids, making them suitable for IV administration. Second, new concepts in pharmacokinetic modeling coupled with advances in the technology of infusion pumps, which allow the use of algorithms such as syringe infusion pumps, TCI, and closed loop system. Propofol with remifentanil seems to be the dominating TIVA technique all over world, delivered either by conventional pumps or by target control systems or by close loop systems5
So TIVA in Fact
Patient friendly, surgeon friendly, anesthesiologist friendly, economically friendly, environmentally friendly, productivity friendly (Fig. 8).5
- TIVA facts.
Conclusion
It was revealed that informational graphics have a more powerful effect, as they emphasize the relationship between two disciplines such as graphic design and TIVA and can inform the anesthesiologist within formative. The infographics are necessary for anesthesiologist, and it is important that they clearly formed enabling methods of TIVA. Infographics can facilitate the understanding of the details of drugs, method, and benefits. It makes it easier to detect understanding of TIVA with simple but perceptual images and information with different colors. TIVA is a viable and safer alternative than inhalation anesthesia now, with lots of advantages over the latter. TCI pumps and advance monitors make administration of TIVA easy and precise. Manually controlled infusions using regular syringe pump can be used to deliver precalculated doses. The newer IV hypnotics and analgesic agents with favorable pharmacokinetic properties have made TIVA feasible in a wide array of varying clinical scenarios. TIVA has become more popular, practical, and possible and will be a new norm in the coming era. Think outside the box and step out of your comfort zone for safe anesthesia, safe surgery, safe patient and safe anesthesiologist with the simple infographics of TIVA.
Conflicts of Interest
None declared.
References
- 2012. p. :199-224. The Power of İnfographics. Indianapolis: Que Publishing
- Ocampo M. Why Infographics are Important? Naldz Graphics. Available at: http://www.naldzgraphics.net/tips/reasons-why-infographics-are-important/. Accessed November 4, 2020
- Principles of total intravenous anaesthesia: practical aspects of using total intravenous anaesthesia. BJA Educ. 2016;16(8):276-280.
- [Google Scholar]
- Guidelines for the safe practice of total intravenous anaesthesia (TIVA): Joint Guidelines from the Association of Anaesthetists and the Society for Intravenous Anaesthesia. Anaesthesia. 2019;74(2):211-224.
- [Google Scholar]
- Haemodynamic effects of the prone position: a comparison of propofol total intravenous and inhalation anaesthesia. Anaesthesia. 2006;61(2):138-141.
- [Google Scholar]
- The antioxidant potential of propofol (2,6-diisopropylphenol) Br J Anaesth. 1992;68(6):613-618.
- [Google Scholar]
- PeDI-Collaborative. Pediatric airway management in COVID-19 patients: Consensus Guidelines from the Society for Pediatric Anesthesia’s Pediatric Difficult Intubation Collaborative and the Canadian Pediatric Anesthesia Society. Anesth Analg. 2020;131(1):61-73.
- [Google Scholar]






