Translate this page into:
Idiopathic Left Posterior Fascicular Ventricular Tachycardia in Children: A Case Report
Abhijit Ari, MD Department of Pediatric Critical Care, DMICC Plot 14, Sector 10, Vidhyadhar Nagar, Jaipur, 302039 Rajasthan India drabhijitari@hotmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The incidence of idiopathic ventricular tachycardia is scarce; however, it is the most common type of ventricular tachycardia in previously normal children. Left posterior fascicular ventricular tachycardia is one of them, and many times it is mismanaged as paroxysmal supraventricular tachycardia. The characteristic features of this arrhythmia are a monomorphic tachycardia, right bundle branch block, and superior axis. This type of arrhythmia is highly sensitive to verapamil, even in infancy, but refractory to adenosine or amiodarone. As nonrecognition of this condition can be fatal, it should be identified early.
Keywords
LPFVT
PSVT
RBBB
superior axis
ECG
verapamil
Introduction
Idiopathic ventricular tachycardia (IVT) is an arrhythmia where conventional evaluation cannot find any defect in the heart. The incidence of this disease in the pediatric population in published studies is scarce1 however, this type of narrow complex ventricular tachycardia (VT) can perplex paroxysmal supraventricular tachycardia (PSVT) particularly when there is no capture or fusion beat. Unfortunately, most cases only show an incomplete right bundle branch block (RBBB) along with a superior axis like our index case.2 Moreover, it is also resistant to adenosine, amiodarone, and direct current cardio version, leading to ventricular dysfunction.3 On the other hand, intravenous calcium channel blockers (e.g., verapamil) terminate 93% of cases in children.4 Therefore, clinicians should be aware of this condition to provide accurate treatment to the patient before further deterioration.
Case
An 8-year-old girl presented to our emergency with a complaint of chest pain and three episodes of vomiting for the last 3 days, along with shortness of breath on the day of admission. There was no significant past medical, family, or surgical history, and she was not on any regular medication. Physical examination findings were normal sensorium, temperature 98.5∙F, heart rate 170/min, blood pressure 107/60 mm Hg, periphery warm, and capillary refilling time was less than 3 seconds. Her respiratory rate was 32/min, no work of breathing, and saturation was 98% in room air. On auscultation, there was bilateral vesicular breath sound and no murmur. Her other systemic examination was unremarkable. In view of respiratory distress and disproportionate tachycardia, a chest X-ray, venous blood gas, serum electrolytes including magnesium, and electrocardiogram (ECG) were requested urgently. Her ECG revealed narrow complex tachycardia (Fig. 1), whereas other investigations were within normal limits. Bedside two-dimensional echocardiogram by the intensivist revealed an apparently normal heart structure with reasonable good cardiac function. In response to the suspected PSVT, she received three doses of injection adenosine; however, her heart rate did not change. Her ECG was discussed with a remote on-call cardiologist who revealed it could be a case of IVT originating from the left ventricle as there was RBBB along with a superior axis and it was refractory to adenosine. Her heart rate and axis returned to normal immediately after receiving one dose of injection verapamil (0.2 mg/kg) over a half-hour infusion (Fig. 2). After overnight monitoring in the critical care unit, the patient was started on oral verapamil the following day and discharged home. A repeat echocardiogram by a pediatric cardiologist before discharge demonstrated morphologically normal heart and systolic function.
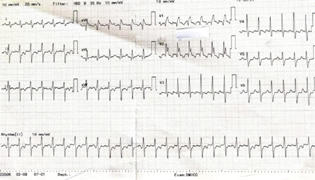
- ECG showing narrow complex tachycardia with suspicion of a PSVT. Showing RBBB with right axis deviation suggesting a idiopathic posterior fascicular ventricular tachycardia.
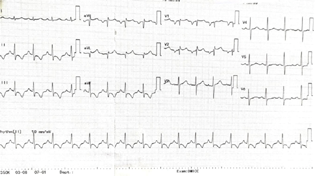
- Normalisation of heart rate and axis on ECG after verapamil infusion.
Discussion
IVT is the most common type of VT in children, in contrast to adults, and it is often misdiagnosed as PSVT.5 It is one type of monomorphic tachycardia with various underlying mechanisms (reentry, triggered activity, and automaticity).6 One variety among them is fascicular VT, and it is further classified into three types7:
-
LPFVT (left posterior fascicular VT): RBBB and superior axis deviation.
-
LAFVT (left anterior fascicular VT): RBBB and right axis deviation.
-
Upper septal fascicular VT (rare): atypical morphology—usually RBBB but can look like left bundle branch block; cases with narrow QRS and normal axis have also been reported.
Incidence of LPFVT is highest in children (65%) and age of onset has two peaks—infancy and adolescence. Clinical features can range from asymptomatic to a variety of symptoms, including nonspecific symptoms such as nausea, vomiting, palpitations, difficulty breathing, and syncope. The triggering factors are exercise, emotional stress, fever, and various medications (e.g., risperidone). However, it is also common even at rest.5
In the emergency department, 13.5% of patients were wrongly labeled as PSVT, and most of them were refractory to common therapy.5 Calcium channel blocker can turn the corner in most cases even when it is used judiciously in infancy.3 Although it could resolve spontaneously, it should be treated aggressively along with a maintenance dose of calcium channel blocker (CCB) or radio frequency catheter ablation as there is an incidence of death as well as tachycardia-induced cardiomyopathy from this disease.5
Conclusion
Idiopathic LPFVT should be considered in differential diagnosis of any PSVT where it does not respond to adenosine and ECG shows characteristic features.8 Knowing about this rare but easily treatable condition in children, physician could prevent morbidity and mortality in them.
Conflict of Interest
None declared.
References
- Idiopathic ventricular tachycardia in infancy and childhood: a multicenter study on clinical profile and outcome. J Am Coll Cardiol. 1999;33(7):2067-2072.
- [Google Scholar]
- Fascicular tachycardia in a child: striking features that improve emergency management. BMJ Case Rep. 2020;13(10):e239657.
- [Google Scholar]
- Fascicular tachycardia in infancy and the use of verapamil: a case series and literature review. Arch Dis Child. 2019;104(8):789-792.
- [Google Scholar]
- Fascicular and nonfascicular left ventricular tachycardias in the young: an international multicenter study. J Cardiovasc Electrophysiol. 2013;24(6):640-648.
- [Google Scholar]
- Clinical spectrum and prognostic factors of pediatric ventricular tachycardia. Circ J. 2010;74(9):1951-1958.
- [Google Scholar]
- Mechanisms of idiopathic left ventricular tachycardia. J Cardiovasc Electrophysiol. 1997;8(5):571-583.
- [Google Scholar]
- Ventricular arrhythmias in the absence of structural heart disease. J Am Coll Cardiol. 2012;59(20):1733-1744.
- [Google Scholar]
- Ten-years follow-up of 20 patients with idiopathic ventricular tachycardia. Pacing Clin Electrophysiol. 1990;13(9):1142-1147.
- [Google Scholar]







