Translate this page into:
Hypoxia during VV ECMO
Pranay Oza, BHMS Riddhivinayak Critical Care and Cardiac Centre S.V. Road, Malad (W), Mumbai 4000064, Maharashtra India drpranay.oza@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Venovenous extracorporeal membrane oxygenation (VV ECMO) is the preferred mode for any kind of acute respiratory failure. The desired PO2 is > 50 and SPO2 > 88% but the acceptable values can be PO2 > 45 and SPO2 > 80%. In case if we are accepting lower PO2, we have to keep a higher hematocrit and meticulously monitor neurological status, lactates, and urine output to maintain oxygen delivery. Saturation during ECMO run depends on ECMO circulation, native circulation, and ratio of ECMO flow to cardiac output (Table 1). Whenever the effective ECMO circulation decreases, saturation decreases. So, decrease in ECMO flow, ECMO FiO2, failing membrane oxygenator, and increase in recirculation will lead to hypoxia. Similarly, anything that decreases the contribution from native circulation will also lead to hypoxia. So, decrease in ventilator settings and worsening lung status lead to hypoxia. Anything that increases metabolism, such as fever and restlessness, will also cause hypoxia due to increased consumption.
|
Abbreviation: ECMO, extracorporeal membrane oxygenation. |
|
Technical problem |
|
Ventilator related |
|
Ventilator malfunctioning |
|
ET tube blockage |
|
ECMO related Decreased ECMO flow or |
|
FiO2 |
|
Oxygenator failure |
|
Increase recirculation |
|
Lung condition worsening |
|
Parenchymal worsening |
|
Pneumothorax |
|
Increased ratio of ECMO flow/cardiac output |
|
Increased cardiac output |
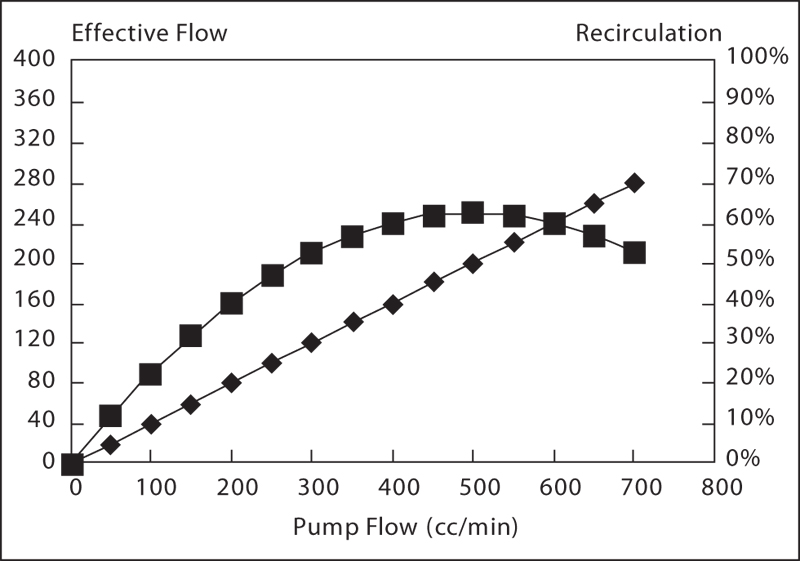
Recirculation is defined as the flow of oxygenated blood from the returning cannula to the draining cannula without entering systemic circulation. It decreases the efficacy of VV support. Around 30% of recirculation is average.1 The factors on which the recirculation depends are pump flow (Fig. 1), catheter position, cardiac output, and RA size or intravascular volume. The recirculation can be calculated with the help of following equation:2

- Recirculation: defining the curve.
Management of hypoxia will depend on treating the underlying cause (Fig. 2). The usual strategy is to increase oxygen transfer by increasing ECMO flow, ECMO FiO2, or by increasing hematocrit and thereby improving oxygen delivery. Many a times hypoxia is secondary to increased metabolic rate and just controlling that (controlling fever, giving sedation) will improve saturation. Recirculation can be managed by adjusting the flow; sometimes a higher flow is the cause of recirculation and just by decreasing flow we can get better saturation.3 Too close placement of tip of drainage and return cannula may lead to recirculation and just repositioning of cannula can improve saturation.4 If the recirculation persists, the last solution is to put additional cannula for drainage and switch to VVV ECMO.
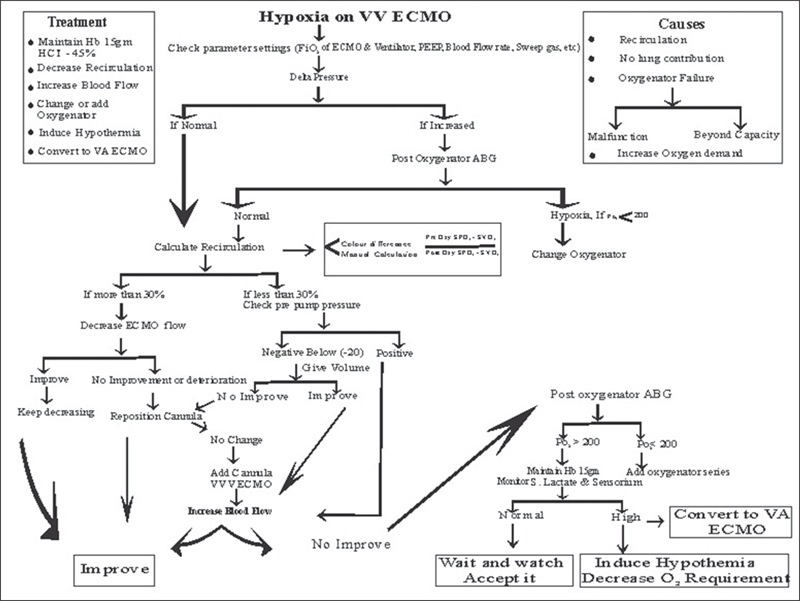
- Approach to hypoxia during VV ECMO. VV ECMO, venovenous extracorporeal membrane oxygenation.
In spite of all the above measures if the patient remains hypoxic and lactates are rising, then the last resource is to induce hypothermia and ultimately switch to VA or VAV ECMO (Table 2).
|
Abbreviations: ECMO, extracorporeal membrane oxygenation; IVC, inferior vena cava; SVC, superior vena cava; VAV, veno-arterial-venous, VV, venovenous. |
|
Maximizing gas transfer |
|
Increase blood flow through the ECMO |
|
Increasing FiO2 of ECMO |
|
Increasing hematocrit |
|
Minimizing oxygen utilization |
|
Decreasing metabolic rate: control fever, sedation, etc |
|
Hypothermia |
|
Decreasing recirculation in VV ECMO |
|
Define the curve |
|
Cannula reposition |
|
Add cannula: for drainage, cannula can be added in IVC, SVC, and preferred cephalad cannula |
|
Conversion to VA or VAV ECMO |
Conclusion
Management of hypoxia during VV ECMO requires attentive monitoring and expedited, algorithmic monitoring.5 It is a balancing act that requires intense vigilance and expertise.
Acknowledgments
We sincerely thank the entire mobile ECMO team of the Riddhivinayak Critical Care and Cardiac center for their dedication and hard work.
References
- Goyal V, Oza P. ECMO Volume I, Practical Manual. Vol. 1
- Heard M, Davis J, Fortenberry J. Principle and practice of venovenous and venoarterial ECMO. ECMO Specialist training manual. Billie Lou Short, Lisa Williams MHA, BSN, RNC-NIC; 2010:59–76
- Bartlett R. Management of ECLS in adult respiratory failure.In: Van Meurs K, Lally K, Peek G, Zwischenberger J, eds. ECMO Extracorporeal Cardiopulmonary Support in Critical Care, Red Book. 3rd ed. ELSO, Ann Arbor;2005:403–416





