Translate this page into:
Handheld Ultrasound Device Utilization in Extracorporeal Membrane Oxygenation Initiation
*Corresponding author: Jonathan Curley, Department of Anesthesiology, University of Virginia, Charlottesville, Virginia, United States. yzs6yf@uvahealth.org
-
Received: ,
Accepted: ,
How to cite this article: Curley J, Renwick C, Mangunta V. Handheld Ultrasound Device Utilization in Extracorporeal Membrane Oxygenation Initiation. J Card Crit Care TSS. 2024;8:246-51. doi: 10.25259/JCCC_41_2024
Abstract
Ultrasound imaging is recommended to augment the initiation of extracorporeal membrane oxygenation (ECMO). Handheld ultrasound devices may serve as potential imaging tools, given the increasing image quality and ultrasound functionality in recent models. Specifically, dual transducer ultrasound devices that provide both a phased array and linear transducer on a single device may offer exceptional value to the intensivist or ECMO clinician. A description of the potential utility of incorporating dual transducer ultrasound devices into ECMO initiation and corresponding images depicting image quality and usage. The dual transducer ultrasound device may serve as a valuable clinical tool for the intensivist or ECMO clinician.
Keywords
Extracorporeal membrane oxygenation
Extracorporeal cardiopulmonary resuscitation
Ultrasound
Critical care
INTRODUCTION
The following text describes the potential utility of utilizing a handheld ultrasound with dual transducer capabilities, specifically linear and phased array, for extracorporeal membrane oxygenation (ECMO) initiation. The authors reference the GE VScan Air SL but have no professional or financial relationship with GE and do not endorse this specific product. Instead, we highlight the advantages of dual transducer design, which offers both phased array and linear capabilities [Figures 1a and b].
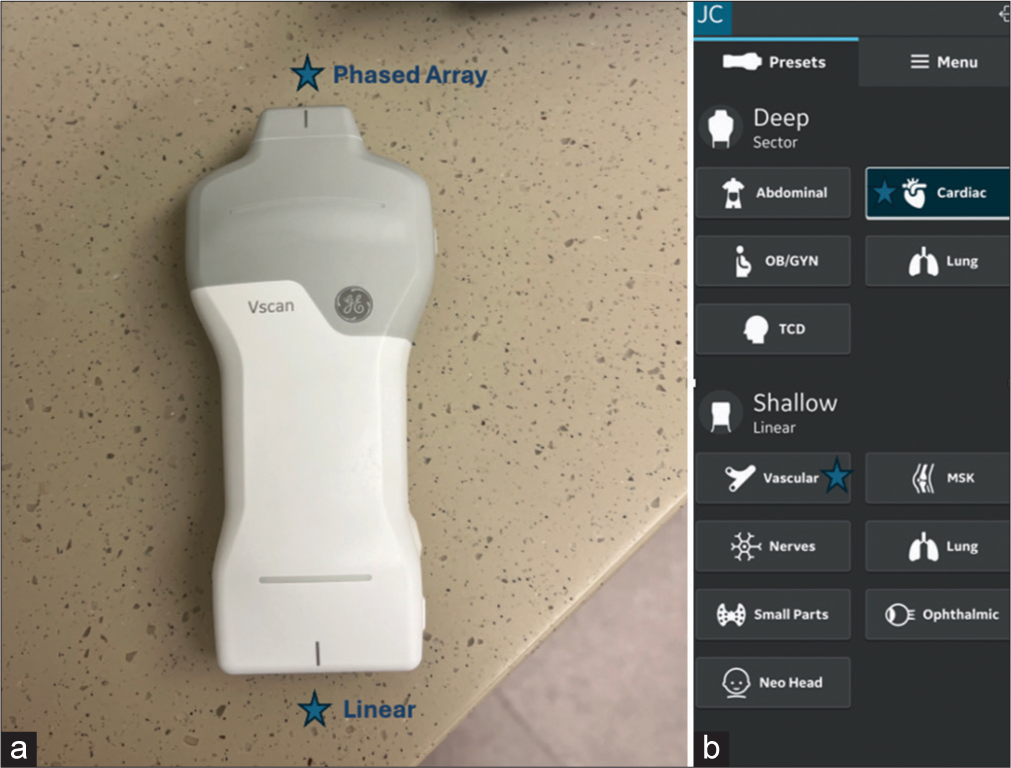
- (a) Image of dual transducer portable handheld device demonstrating phased array and linear transducers. (b) Image of a display screen for a device from a cellular phone.
ECMO may be utilized in cases of severe heart or lung failure refractory to optimal medical management per the extracorporeal life support organization (ELSO) guidelines.[1-3] In these circumstances, the guidelines recommend imaging guidance for initiation of venovenous (VV)-ECMO, venoarterial (VA)-ECMO, and extracorporeal cardiopulmonary resuscitation (ECPR).[2-4] Specifically, the guidelines recommend vascular ultrasound if percutaneous access is utilized, followed by either fluoroscopy or ultrasound to ensure appropriate wire and cannula placement. The ultrasound modalities recommended for wire and cannula placement and positioning include transthoracic echocardiography (TTE) or transesophageal echocardiography (TEE). The decision on which imaging modality to employ may be based on individual clinician experience, clinical urgency of initiation, available equipment, and available personnel to operate this equipment.
Ultra-portable handheld ultrasound devices, with the ability to project clinical imaging directly onto a phone or other mobile device, are becoming increasingly common in medical practice. Historically, the primary utility of these handheld devices has been diagnostic rather than procedural. A likely explanation for this is that clinicians have been required to choose a specific single transducer with functional capabilities limited to that transducer’s specific properties. While lower frequency-phased array transducers offer the excellent ability to image deep structures and, therefore, diagnose pathology, these ultrasound devices are limited in their ability to image the shallow structures necessary for procedural use. However, several manufacturers are now offering ultrasound devices with two separate transducers on a single device. One such example is the GE VScan Air SL, which includes a high-frequency linear and a low-frequency phased array transducer [Figures 1a and b]. This new technology allows clinicians to have immediate ultrasound access for both diagnostic and procedural purposes and holds exceptional potential value to the ECMO clinician.
UTILIZATION OF HANDHELD ULTRASOUND IN ECMO INITIATION
Pre-ECMO initiation
In 2015 ELSO general guidelines on ultrasound use, the authors note that vascular and cardiac assessment of a patient in the pre-ECMO initiation period may be useful for determining the etiology of organ failure, identifying contraindications for ECMO support, and determining cannula sizing based on vessel size.[5] A dual transducer ultrasound device may serve as an effective tool for the ECMO practitioner, as it allows the clinician to assess both cardiac and vascular structures using a single portable device that can be conveniently carried in the provider’s pocket, rather than requiring mobilization of a large cart-based system [Figures 1a and b].
ECMO initiation
The clinical availability of handheld dual transducer ultrasound devices facilitates ongoing ultrasound assessment throughout the ECMO initiation process, requiring only minor adjustments to the initial preparation and draping process. First, the ECMO clinician may consider cutting ultrasound access points into the patient draping and covering these sites with a sterile adhesive barrier, as demonstrated in Figure 2. The sites the cannulating operator may consider exposing for ultrasound access include the planned vascular access site, a right-sided trans-hepatic site to allow visualization of the inferior vena cava (IVC) and aorta, and/or the subcostal standard FoCUS view for cardiac as well as IVC and aorta visualization. Second, the wireless handheld ultrasound device can be placed in a sterile ultrasound cover and positioned on the sterile field for ongoing use at the clinician’s discretion. This is demonstrated in Figure 3a, where the handheld ultrasound, in a sterile ultrasound probe cover, is placed on the sterile field after being used to obtain vascular access with imaging displayed on a cellular phone screen. This process allows the clinician to maintain ongoing ultrasound assessment of all potential sites of interest using a single device confined to the sterile field. This process may offer several benefits, including a theoretical reduction of infection risk by eliminating a wired connection to the non-sterile environment and providing the clinician with the ability to easily alternate between deep and shallow imaging using the single ultrasound with two available transducers – a function not available with cart-based ultrasound systems.
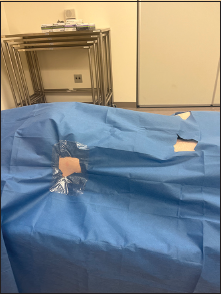
- Demonstration of sterile draping with ultrasound access points covered with a sterile ultrasound-compatible barrier.
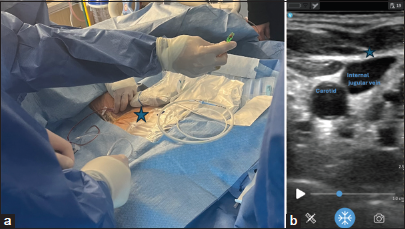
- (a) Image of contained ultrasound device on sterile field without wired connection. This image depicts the utilization of a portable handheld device and a cellular phone image display for placing a venous return cannula in a venovenous-extracorporeal membrane oxygenation patient. Asterix: Venous return cannula in VV ECMO. (b) Demonstration of the cellular phone image obtained from the procedure in 3a. Cell phone ultrasound image of the venous ECMO cannula.
After the patient is adequately prepared and draped with the above-described techniques, the dual transducer ultrasound device allows for ongoing ultrasound utilization throughout the ECMO initiation. First, if a percutaneous Selinger technique is to be used, the vascular imaging transducer should be utilized to guide vascular access in accordance with ELSO guidelines.[1-7] The current handheld ultrasound devices’ image quality has greatly improved since arriving on the market and currently provides adequate quality for image-guided procedures. This handheld ultrasound linear transducer image quality is demonstrated in Figure 3b and Video 1, depicting needle entry into the right internal jugular vein as part of placing a venous return cannula in a VV ECMO patient. In addition, Figure 4a-c demonstrate imaging of relevant femoral anatomy in a live model, and Figure 5a-e demonstrate imaging of a synthetic model with needle and wire placement. Once vascular access is established, if access to the right transhepatic or subcostal view was previously made accessible, the clinician can switch to the low-frequency phased array transducer to ensure stiff wire and cannula placement in the appropriate deep vascular structure. This transition is of particular importance when placing an internal jugular bi-caval dual lumen cannula to prevent severe complications such as ventricular rupture secondary to wire and subsequent dilator/cannula misplacement. Figure 6a-c and Videos 2 and 3 demonstrate the ultrasound imaging of the IVC and aorta through imaging the right transhepatic view. As indicated by the images and descriptions above, a dual-transducer handheld ultrasound device uniquely enables the identification of relevant anatomic vascular structures, procedurally access to these structures, and finally, the assessment of proper positioning of wires and cannulas within an appropriate deep vascular structure, all using a single device.
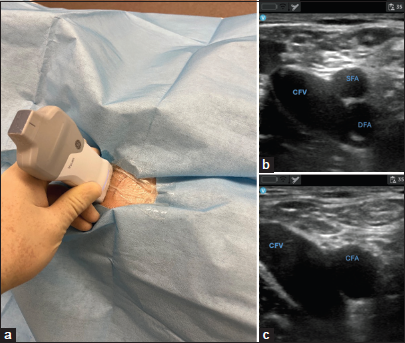
- (a) Demonstrating femoral vascular image acquisition. (b and c) Demonstrating imaging obtained on cellular phone display.
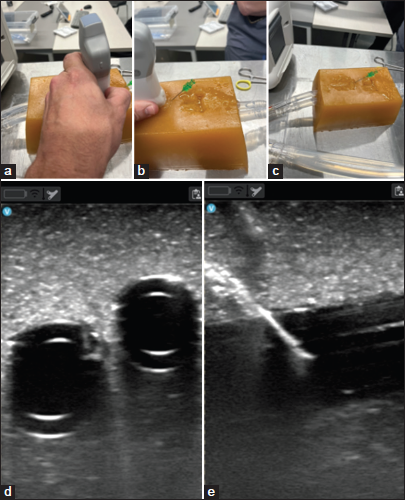
- (a-c) Demonstrating image acquisition, access, and wire placement in synthetic model. (d and e) demonstrates ultrasound imaging in synthetic model.
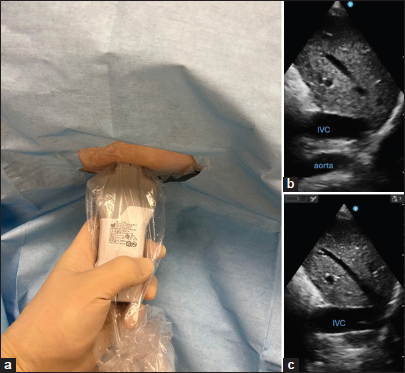
- (a) Demonstrating transhepatic view for confirming wire placement. (b and c) Demonstrating transhepatic ultrasound view anatomy.
Video 1:
Video 1:Demonstration of right internal jugular vein access utilizing cellular phone for image display.Video 2:
Video 2:Demonstrating transhepatic ultrasound view obtained on cellular phone alternating between inferior vena cava and aorta.Video 3:
Video 3:Demonstrating transhepatic ultrasound view obtained on cellular phone demonstrating inferior vena cava view.Post ECMO initiation
In the 2015 ELSO guidelines for the use of ultrasound in VV[6] and VA ECMO[7], the authors recommend the use of ultrasound after ECMO initiation to evaluate for cardiac tamponade, hypovolemia, and left ventricle distention and to assess cannula positioning. Early assessment of cannula positioning before securing and applying sterile dressings may be particularly helpful as repositioning may be required. This is of particular importance when using the bi-caval dual-lumen single-site cannula, which requires bi-caval positioning in both the superior vena cava and IVC, with the outflow jet directed toward the tricuspid valve. The assessment of this positioning, along with the evaluation of the other items above, can be completed using the phased array portion of a handheld device applied to the subcostal view, as demonstrated in [Figure 7] and [Video 4].
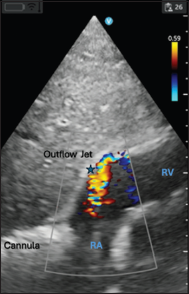
- Demonstrating the appropriate positioning of a dual lumen single site veno-venous extracorporeal membrane oxygenation cannula. RA: Right Atrium, RV: Right Ventricle, Asterix: Demonstrating flow of cannula return directed toward tricuspid valve with color flow doppler.
Video 4:
Video 4:Demonstrating subcostal view for dual lumen single site venovenous-extracorporeal membrane oxygenation with return flow directed toward the tricuspid valve.CONCLUSION
The use of handheld ultrasound devices is increasing in the field of medicine. The newly available handheld dual-transducer ultrasound devices, which combine phased array capabilities along with a linear transducer, may be particularly useful for the ECMO clinician. These devices are highly portable compared to cart-based systems and remain immediately available to the ECMO clinician in any setting. With these devices, the clinician can independently perform all necessary imaging without assistance, rather than relying on providers outside of the sterile field to operate traditional cart-based ultrasonography (TTE or TEE) or fluoroscopy. Using a single ultrasound device, the clinician can establish vascular access, follow wire and cannula placement, continuously assess all interventions, and optimally position cannulas post-ECMO initiation. This immediate availability of handheld “pocket” ultrasound devices, along with the ability to independently perform access, placement, positioning, and ongoing assessments, may be of value to the intensivist ECMO clinician. In addition, the utilization of such a device offers further advantages, such as freeing up space that would otherwise be occupied by imaging devices and personnel and allowing complete containment of the imaging device within the sterile environment, potentially enhancing the sterility of the procedure.
Despite these advantages over traditional cart-based ultrasonography or fluoroscopy, the authors do not currently advocate for the replacement of standard imaging modalities with handheld ultrasound devices in all cases. Instead, the authors emphasize the many advantages these devices offer and recommend that individual ECMO clinicians consider these advantages in relation to specific clinical scenarios. For instance, in cases of ECPR, a handheld ultrasound device may provide superior value to the ECMO clinician compared to cart-based systems due to its portability and ability to serve as both a diagnostic and procedural tool. Similarly, handheld devices may prove more valuable to clinicians in resource-limited settings, whether due to financial constraints, limited physical space, or a shortage of personnel to operate other modalities. While the authors do not suggest replacing traditional imaging modalities in resource-rich, non-ECPR, or non-emergent settings, they do propose that handheld devices could serve as useful adjuncts, for example, when used alongside fluoroscopy as a secondary imaging tool.
To the authors’ knowledge, there is currently no described usage of portable handheld ultrasound devices for ECMO initiation in the literature. This description is both the first documented clinical use of a handheld portable ultrasound device in ECMO initiation as well as the first generalized description of the potential benefits of incorporating a handheld ultrasound into routine ECMO equipment. This description may be of value to the intensivist and ECMO clinician, particularly in ECPR cases and in resource or personnel-limited settings. The authors present this discussion to bring awareness to the potential benefits of these devices. However, further research/discussion on this topic is warranted before mass implementation.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available online at
Financial support and sponsorship
Nil.
References
- General Guidelines for Cardiopulmonary Extracorporeal Life Support. 2017. Ann Arbor, MI, USA: ELSO; Version 1.4 Available from: https://www.elso.org [Last accessed on 2024 Aug 21]
- [Google Scholar]
- Management of Adult Patients Supported with Venovenous Extracorporeal Membrane Oxygenation (VV ECMO): Guideline from the Extracorporeal Life Support Organization (ELSO) ASAIO J. 2021;67:601-10.
- [CrossRef] [Google Scholar]
- ELSO Interim Guidelines for Venoarterial Extracorporeal Membrane Oxygenation in Adult Cardiac Patients. ASAIO J. 2021;67:827-44.
- [CrossRef] [Google Scholar]
- Extracorporeal Cardiopulmonary Resuscitation in Adults. Interim Guideline Consensus Statement from the Extracorporeal Life Support Organization. ASAIO J. 2021;67:221-8.
- [CrossRef] [Google Scholar]
- Ultrasound Guidance for Extracorporeal Membrane Oxygenation General Guidelines. Ann Arbor, MI, USA: Extracorporeal Life Support Organization. 2015. Available from: https://www.elso.org [Last accessed on 2024 Aug 21]
- [Google Scholar]
- Ultrasound Guidance for Extracorporeal Membrane Oxygenation Veno-Venous ECMO Specific Guidelines. Ann Arbor, MI, USA: Extracorporeal Life Support Organization. 2015. Available from: https://www.elso.org [Last accessed on 2024 Aug 21]
- [Google Scholar]
- Ultrasound Guidance for Extracorporeal Membrane Oxygenation Veno-Arterial ECMO Specific Guidelines. Ann Arbor, MI, USA: Extracorporeal Life Support Organization. 2015. Available from: https://www.elso.org [Last accessed on 2024 Aug 21]
- [Google Scholar]







