Translate this page into:
Evaluation of Clinical Characteristics and Predictors for Outcomes of In-Hospital Cardiac Arrest
*Corresponding author: Alexander Polyak, Department of Medicine, Cedars-Sinai Medical Center, Los Angeles, California, United States. alexander.polyak@cshs.org
-
Received: ,
Accepted: ,
How to cite this article: Polyak A, Tacon PR, Krom Z, Friedman O, Mirocha J, Matusov Y. Evaluation of Clinical Characteristics and Predictors for Outcomes of In-Hospital Cardiac Arrest. J Card Crit Care TSS. 2025;9:21-8. doi: 10.25259/JCCC_52_2024
Abstract
Objectives:
In-hospital cardiac arrest (IHCA) is a common event for hospitalized patients with high rates of morbidity among survivors. The goal of this study was to evaluate clinical characteristics and compare expected versus observed outcomes of IHCA.
Material and Methods:
This was a retrospective study. Patient characteristics, IHCA outcome (return of spontaneous circulation [ROSC]), and neurologic outcomes (favorable outcome defined as cerebral performance category [CPC] score of 1 or 2 at discharge) were collected. The Good Outcomes Following Attempted Resuscitation (GO-FAR) score was applied retrospectively to patients preceding cardiac arrest and compared to actual outcomes.
Results:
There was a significant association between GO-FAR score and survival to discharge (P = 0.001) and GO-FAR score and CPC score (P = 0.0001). There was also an association of shorter IHCA duration and CPC score (P = 0.03). There was no association between GO-FAR score and likelihood of ROSC (P = 0.30).
Conclusion:
The GO-FAR score has an association with favorable outcomes after IHCA and may help inpatient physicians prognosticate expected outcomes before IHCA.
Keywords
In-hospital cardiac arrest
Cardiac arrest
Good outcomes following attempted resuscitation score
return of spontaneous circulation
Neurologic outcomes after cardiac arrest
INTRODUCTION
In-hospital cardiac arrest (IHCA) is a common event with high morbidity rates among survivors. The Get with the Guidelines-Resuscitation registry found that the IHCA event rate was 0.92/1000 hospital days, estimating over 200,000 treated cardiac arrests among patients admitted to hospitals every year in the United States.[1] Survival to discharge of IHCA is estimated to be between 12% and 25%.[2,3] Among those patients who are discharged, it has been estimated that about 85% are discharged with good neurological outcomes, defined as a cerebral performance category (CPC) score of 1 or 2.[4,5] However, the likelihood of good neurologic outcomes may vary substantially based on patient comorbidities preceding IHCA.[2]
Physicians themselves have been shown to be poor predictors of IHCA outcomes.[6-8] Different scoring models have been developed to assist in objective prognostication. The Good Outcomes Following Attempted Resuscitation (GO-FAR) score was developed as a tool to help physicians prognosticate resuscitation outcomes in their patients if they were to have an IHCA.[9] A higher This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms. ©2025 Published by Scientific Scholar on behalf of Journal of Cardiac Critical Care TSS GO-FAR score is predictive of poor neurological outcomes after IHCA and has been validated in prior studies, but has also recently been suggested that it may need to be reexamined and re-calibrated as IHCA outcomes have improved since the score was first developed.[3,10-15]
The goal of this study was to describe clinical characteristics of patients experiencing IHCA and identify clinical factors and scoring systems which accurately predict return of spontaneous circulation (ROSC), survival to discharge, and survival with favorable neurologic function.
MATERIAL AND METHODS
Preparations
This was a single-center retrospective study of all adult patients who had IHCA while admitted to Cedars-Sinai Medical Center (CSMC) between August 01, 2021, and June 30, 2022. CSMC is a major quaternary academic referral center in Los Angeles, California, with an average daily census of over 980 patients. This study was approved by the CSMC Institutional Review Board (IRB #00002119, approved 5/10/2022, “Prognosis and outcomes of in-hospital cardiac arrest”). Study-specific consent was waived by the IRB and the study was conducted in accordance with the Declaration of Helsinki.
Patient screening
CSMC’s internal electronic health record (Epic Systems, Madison, WI) was used to flag all IHCA (“Code Blue”) events for analysis. Patients were excluded if they were under 18 years of age, had cardiac arrest in the emergency department, if they were not pulseless, if Code Blue was called despite Do Not Attempt Resuscitation (DNAR) orders, if they were unidentified patients, or if they had a research opt-out flag. Only the first IHCA episode was included for patients with multiple IHCA during the same hospitalization.
Data collection
We collected patient information from CSMC’s internal electronic health record, including self-reported basic demographics, number of medications on the day of IHCA, initial rhythm of IHCA, duration of IHCA, time of IHCA (day shift defined as 7:00–19:00 and night shift defined as 19:00–7:00), length of stay (LOS) before IHCA, the presence or absence of ROSC, and CPC score on hospital discharge. IHCA was defined as a pulseless rhythm necessitating code blue response and initiation of cardiopulmonary resuscitation. GO-FAR scores were calculated by collecting the following 13 variables from the electronic health record – age, neurological status, major trauma present, acute stroke present, metastatic or hematologic cancer diagnosis, septicemia present (defined as a documented bloodstream infection), non-cardiac admission diagnosis, hepatic insufficiency (defined as total bilirubin >2 mg/dL, aspartate aminotransferase >2 times the upper limit of normal, or cirrhosis diagnosis), admitted from a skilled nursing facility, hypotension or hypoperfusion (defined as systolic blood pressure <90 mmHg, mean arterial pressure <60 mmHg, or use of vaso-active medications), renal insufficiency or dialysis dependent, respiratory insufficiency (defined as PaO2/FiO2 (P/F) ratio <300, PaO2 < 60, SaO2 < 90%, respiratory rate >40 or <5, or use of noninvasive or invasive ventilation), and pneumonia present (defined as documented pneumonia by physician provider with antibiotics not yet started or still ongoing). A GO-FAR score of ≥24 equates to very low survival (<1%) to discharge with favorable neurologic outcome; score of 14–23 equates to low survival (1–3%) to discharge with favorable neurologic outcome; score of −5–13 equates to average survival (3–15%) to discharge with favorable neurologic outcome; and a score of −15–−6 equates to above average survival (>15%) to discharge with favorable neurologic outcome [Table 1].[9] Collected data and the categorization of outcome were reviewed by at least two of the authors (AP, PT, and YM) independently so as to minimize information bias.
| GO- FAR score | Likelihood of survival to discharge with a favorable neurologic outcome |
|---|---|
| ≥ 24 | Very low (<1%) |
| 14 to 23 | Low (1-3%) |
| -5 to 13 | Average (3-15%) |
| -15 to -6 | Above average (>15%) |
GOFAR: Good Outcomes Following Attempted Resuscitation, CPC: Cerebral performance category
Statistical methods
Categorical variables were summarized by frequency and percentage. Approximately normally distributed numerical variables were summarized by mean and standard deviation (SD), and non-normally distributed numerical variables were summarized by median and interquartile range. Approximate normality was assessed by visual inspection of the histograms of the variables in the comparison groups. The Fisher exact test was used to assess group differences on categorical variables. The independent samples t-test was used to assess group differences on approximately normally distributed numerical variables (age and GO-FAR score), while the Wilcoxon rank-sum test was used for group differences on numerical variables that were not approximately normally distributed (LOS, IHCA duration). The t-statistic and degrees of freedom were reported when the independent samples t-test was applied, and the z-statistic was reported when the Wilcoxon rank sum test was applied. Logistic regression models were used to assess potential factors associated with outcomes and adjusted odds ratios (OR), and their 95% confidence intervals were reported. Multivariable regression analysis could not be completed due to sample size and low event rates. A two-sided 0.05 significance level was used throughout. Statistical analysis was done in SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Description of the cohort
There were 417 Code Blue events during the study period. Of those, 161 were excluded due to being out of hospital or emergency department cardiac arrests (98), not pulseless (50), and other reasons, including pediatric patients, DNAR patients, and unidentified patients (13). The remaining 256 IHCA events included repeat IHCA (56) and were excluded from the study. The remaining 200 IHCA events met eligibility criteria and were used for statistical analysis [Figure 1].
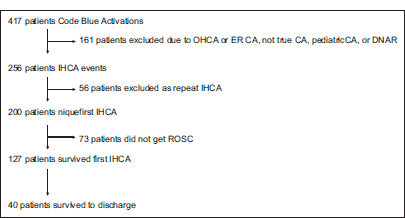
- Flow diagram of the study population. CA: Cardiac arrest, OHCA: Out of hospital cardiac arrest, ER CA: Emergency room cardiac arrest, CA: Cardiac arrest, DNAR: Do not attempt resuscitation, IHCA: In-hospital cardiac arrest, ROSC: Return of spontaneous circulation.
The study’s primary outcome was the association between GO-FAR score and survival with good neurologic function (CPC score 1–2). Secondary outcomes were associations between age, race, number of medications prescribed at the time of IHCA, duration of IHCA, LOS before IHCA, initial rhythm of IHCA (shockable [pulseless ventricular tachycardia or ventricular fibrillation] vs. non-shockable [pulseless electrical activity, asystole]), time of IHCA, ROSC, and CPC score at discharge.
Baseline characteristics
The baseline characteristics of the 200 patients are described in Table 2. The mean age of patients was 69.2 years (SD 16.2), 81 patients (40.5%) were female, 136 patients (68.0%) were white, and 46 patients (23.0%) identified as Hispanic/LatinX. At the time of IHCA, patients were on a median of 17 different medications (scheduled and as needed). The mean GO-FAR score was 14.0 and the median was 12.0. Fifty-five (27.5%) patients had a GO-FAR score of 24 or greater (predictive of very low survival of <1%). IHCA occurred at a median of 6.6 days into the admission, occurred during the day shift 48.5% of the time, and was in the intensive care unit (ICU) 39.0% of the time. The initial rhythm was a shockable rhythm (ventricular fibrillation or pulseless ventricular tachycardia) 17.0% of the time. The median IHCA duration was 17.0 min. ROSC was achieved in 127 (63.5%) patients. Forty (20.0%) patients survived to discharge. Of those patients who survived to discharge, 26 (65.0%) had a favorable CPC score.
| Variable | Total, n=200 |
|---|---|
| Mean ageyears (SD) | 69.2±16.2 |
| Female sex n(%) | 81 (40.5) |
| Race n(%) | |
| AfricanAmerican/Black | 25 (12.5) |
| Asian | 22 (11.0) |
| Other/Multiple | 17 (8.5) |
| White | 136 (68.0) |
| EthnicityHispanic/LatinX n(%) | 46 (23.0) |
| Median number of medications on day of IHCA(IQR) | 17 (13–23) |
| Median LOS before IHCAdays (IQR) | 6.6 (1.7–15.0) |
| Location of IHCA (ICU)n(%) | 78 (39.0) |
| Time of day of IHCA (day shift)n(%) | 97 (48.5) |
| Median IHCA durationminutes (IQR) | 17.0 (7.0–25.0) |
| Mean GOFAR score(SD) | 14.0±13.1 |
| Median GOFAR score(IQR) | 12.0 (3.0–25.5) |
| Initial rhythm of CA n(%) | |
| Not shockable | 166 (83.0) |
| Shockable | 34 (17.0) |
| Outcome of IHCA n(%) | |
| Expired | 73 (36.5) |
| ROSC | 127 (63.5) |
| Survival to discharge n(%) | 40 (20.0) |
Shockable rhythm defined as ventricular tachycardia or fibrillation without a pulse, nonshockable rhythm defined as asystole or pulseless electrical activity, IHCA: Inhospital cardiac arrest, IQR: Interquartile range, SD: Standard deviation, LOS: Length of stay, ICU: Intensive care unit, GOFAR: Good Outcomes Following Attempted Resuscitation, CA: Cardiac arrest, ROSC: Return of spontaneous circulation
Association between variables and likelihood of ROSC
Of the identified variables, the duration of IHCA was associated with ROSC [Table 3]. Patients who did not survive to ROSC had a code that was, by median, 14.0 min longer than that of patients who did survive to ROSC (P < 0.0001).
| Variable | Expired | ROSC | Statistic (Degrees of freedom) | P -value |
|---|---|---|---|---|
| Total, n=200 | 73 | 127 | ||
| Mean age-years (SD) | 68.7±17.0 | 69.5±15.8 | t=0.37 (198) | 0.71 |
| Female sex-n (%) | 31 (42.5) | 50 (39.4) | * | 0.76 |
| Race-n (%) | ||||
| African-American/Black | 11 (15.1) | 14 (11.0) | * | 0.79 |
| Asian | 8 (11.0) | 14 (11.0) | ||
| Other/Multiple | 7(9.6) | 10 (7.9) | ||
| White | 47 (64.4) | 89 (70.1) | ||
| Ethnicity-Hispanic/Latinx-n (%) | 14 (19.2) | 32 (25.2) | * | 0.38 |
| Median medications on day of IHCA-(IQR) | 15.5 (12-24) | 18 (14-23) | z=1.51 | 0.13 |
| Median LOS before IHCA-(IQR) | 6.7 (2.5-16.6) | 6.1 (1.4-14.4) | z=1.14 | 0.26 |
| Location of IHCA (ICU)-n (%) | 37 (50.7) | 41 (32.3) | * | 0.02 |
| Time of day of IHCA (day shift)-n (%) | 38 (52.1) | 59 (46.5) | * | 0.47 |
| Median IHCA duration-minutes (IQR) | 24.5 (20.0-37.0) | 10.0 (5.0-18.0) | z=7.56 | <0.0001 |
| Mean GO-FAR score-(SD) | 15.2±12.6 | 13.2±13.4 | t=1.04 (198) | 0.30 |
| Median GO-FAR score (IQR) | 14.0 (5.0-27.0) | 12.0 (3.0-23.0) | ||
| Non-shockable rhythm-n (%) | 61 (83.6) | 105 (82.7) | * | >0.99 |
Expired patients (no ROSC) were compared to all patients who achieved ROSC. *There is no test statistic for the Fisher exact test. IHCA: In-hospital cardiac arrest, IQR: Interquartile range, LOS: Length of stay, ICU: Intensive care unit, GO-FAR: Good Outcomes Following Attempted Resuscitation, ROSC: Return of spontaneous circulation, Bold values: indicates statistical significance (P < 0.05)
A larger proportion of patients who expired had IHCA in the ICU, as compared to outside the ICU (P = 0.02). There was no association with survival to ROSC between age, sex, number of medications prescribed to the patient on the day of IHCA, LOS before IHCA, time of day of IHCA, GO-FAR score, or initial rhythm. Using logistic regression, we found no evidence of an association between White and non-White patients and the likelihood of ROSC (OR 1.30, 95% CI 0.70–2.39, P = 0.41).
Logistic regression models showed that having a normal mental status earlier in the day preceding IHCA (OR 2.1, 95% CI 1.2–3.9; P = 0.01) and having IHCA outside of the ICU (OR 2.2, 95% CI 1.2–3.9; P = 0.01) were associated with ROSC. For every 10-minute increase in IHCA duration, there was an associated reduced odds of ROSC (OR 0.5, 95% CI 0.4–0.6; p < 0.001). There was no evidence of association between age, GO-FAR score, race, shockable versus nonshockable initial rhythm, time of day, and ROSC.
Association between predictive variables and survival to hospital discharge
Although the GO-FAR score was not associated with achieving ROSC, it was strongly associated with survival to discharge, as shown in Table 4; patients who survived to hospital discharge had a mean GO-FAR score of 7.9 versus 15.5 for those who died before discharge (95% CI 3.14–12.06; P = 0.001). Figure 2 shows a ROC curve for GO-FAR score and survival to discharge. A 5-point decrease in GO-FAR score was associated with a 30% increase in odds of survival to discharge (OR 1.3, 95% CI 1.10– 1.50; p-value 0.002). Other factors individually associated with survival to discharge were LOS before IHCA and duration of IHCA – an IHCA earlier in a patient’s admission (P = 0.01) and a shorter duration of IHCA (P < 0.0001) were associated with survival to discharge. Of patients who survived to discharge, 25% had IHCA in the ICU, as compared to 42.5% of patients who died before discharge (P = 0.05).
| Variable | Discharged alive | Expired before discharge | Statistic (Degrees of freedom) | P-value |
|---|---|---|---|---|
| Total, n=200 | 40 | 160 | ||
| Mean age-years (SD) | 67.2±14.7 | 69.7±16.6 | t=0.90 (198) | 0.37 |
| Female sex-n (%) | 15 (37.5) | 66 (41.3) | * | 0.72 |
| Race-n (%) | ||||
| African-American/Black | 7 (17.5) | 18 (11.3) | * | 0.66 |
| Asian | 4 (10.0) | 18 (11.3) | ||
| Other/Multiple | 4 (10.0) | 13 (8.1) | ||
| White | 25 (62.5) | 111 (69.4) | ||
| Ethnicity-Hispanic/Latinx-n (%) | 11 (27.5) | 35 (21.9) | * | 0.53 |
| Median medications on day of IHCA (IQR) | 17 (12.5-21) | 17 (13-23) | z=0.88 | 0.38 |
| Median LOS before IHCA (IQR) | 1.8 (0.6-10.6) | 6.9 (2.9-16.8) | z=2.63 | 0.01 |
| Location of IHCA (ICU)-n (%) | 10 (25.0) | 68 (42.5) | * | 0.05 |
| Time of day of IHCA (day shift)-n (%) | 22 (55.0) | 75 (46.9) | * | 0.38 |
| Median IHCA duration-minutes (IQR) | 8.1 (4.0-13.0) | 19.5 (9.0-28.5) | z=4.52 | <0.0001 |
| Mean GO-FAR score (SD) | 7.9±11.0 | 15.5±13.2 | t=3.35 (198) | 0.001 |
| Median GO-FAR score (IQR) | 8.5 (-0.5-14.0) | 14.0 (5.0-27.0) | ||
| Non-shockable rhythm-n (%) | 32 (80.0) | 134 (83.8) | * | 0.64 |
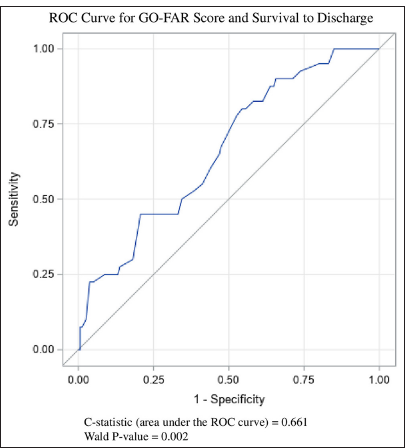
- Receiver operating characteristic (ROC) curve for good outcomes following attempted resuscitation (GO-FAR) score and survival to discharge.
There was no evidence of association between survival to hospital discharge and age, sex, race, ethnicity, number of medications, time of day, or initial rhythm of IHCA.
Association between variables and neurologic outcome (CPC score) at discharge
Among patients who survived to discharge, only their respective GO-FAR score and duration of the IHCA had an association with a favorable neurologic outcome at discharge, as shown in Table 5. The median duration of IHCA with a favorable neurologic outcome was 6.0 min compared to 10.5 min for unfavorable neurologic outcome (P = 0.03). The mean GO-FAR score among patients with an unfavorable neurologic outcome was 16.3, compared to a mean GO-FAR score of 3.4 for patients with a favorable neurologic outcome (95% CI 6.70–19.10; P = 0.0001). The distribution of GOFAR scores between unfavorable and favorable neurologic outcomes is shown in Figure 3. A ROC curve is shown in Figure 4 with a 5-point decrease in GO-FAR score associated with an 110% increase in odds of a favorable outcome to discharge (OR 2.1, 95% CI 1.29–3.52; P = 0.003).
| Variable | Unfavorable (CPC score 3-5) | Favorable (CPC score 1-2) | Statistic (Degrees of freedom ) | P-value |
|---|---|---|---|---|
| Total, n=40 | 14 | 26 | ||
| Mean age-years (SD) | 66.5±12.5 | 67.5±16.0 | t=0.84 (38) | 0.84 |
| Female sex-n (%) | 6 (35.7) | 10 (38.5) | * | >0.99 |
| Race-n (%) | ||||
| African American/Black | 3 (21.4) | 4(15.4) | * | 0.56 |
| Asian | 0 (0) | 4(15.4) | ||
| Other/Multiple | 1 (7.1) | 3 (11.5) | ||
| White | 10 (71.4) | 15 (57.7) | ||
| Ethnicity-Hispanic/Latinx-n (%) | 5 (35.7) | 6 (23.1) | * | 0.47 |
| Median medications on day of IHCA (IQR) | 17.0 (13.0-20.0) | 16.5 (11.0-21.0) | z=0.03 | 0.98 |
| Median LOS before IHCA (IQR) | 4.6 (0.8-11.6) | 1.5 (0.5-8.1) | z=0.74 | 0.47 |
| Location of IHCA (ICU)-n (%) | 4 (28.6) | 6 (23.1) | * | 0.72 |
| Time of day of IHCA (day shift)-n (%) | 9 (64.3) | 13 (50.0) | * | 0.51 |
| Median IHCA duration-minutes (IQR) | 10.5 (8.0-22.0) | 6.0 (4.0-10.0) | z=2.14 | 0.03 |
| Mean GO-FAR score (SD) | 16.3±9.7 | 3.4±9.0 | t=4.22 (38) | 0.0001 |
| Median GO-FAR score (IQR) | 15.0 (9.0-19.0) | 3.0 (-4.0-11.0) | ||
| Non-shockable rhythm-n (%) | 12 (85.7) | 20 (76.9) | * | 0.69 |
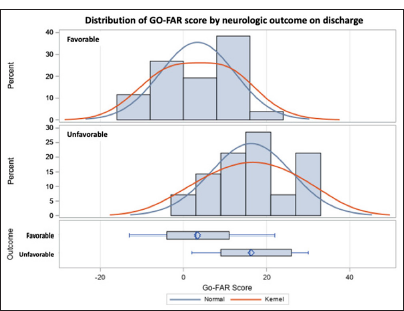
- Good outcomes following attempted resuscitation (GOFAR) score distribution among patients with a favorable neurologic outcome at discharge compared to the GO-FAR score distribution of patients with an unfavorable neurologic outcome at discharge. The top graph is the distribution of GO-FAR scores in patients with favorable neurologic outcomes and the middle graph is a distribution of GO-FAR scores in patients with an unfavorable neurologic outcome. The bottom chart is a distribution plot. A kernel graph is a smooth curve that estimates the probability density function of a continuous variable.
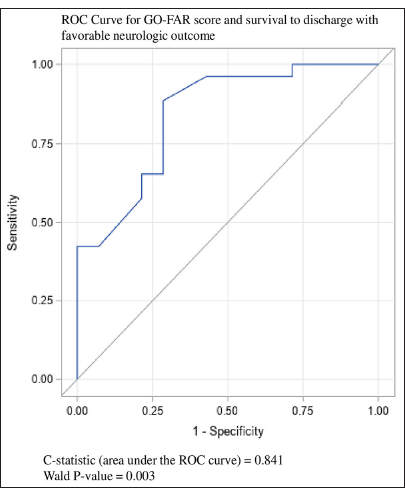
- Receiver operating characteristic (ROC) curve for good outcomes following attempted resuscitation (GO-FAR) score and survival to discharge with favorable neurologic outcome.
There was no evidence of association with favorable neurologic outcomes between age, sex, race, ethnicity, number of medications, LOS before IHCA, location, time of day, or initial rhythm of IHCA.
DISCUSSION
In this retrospective analysis of 200 first episodes of IHCA at a large, quaternary medical center, we found that duration of cardiac arrest was strongly associated with ROSC, likelihood of survival to discharge, and more favorable CPC score at discharge among those who survived. In addition, we found that GO-FAR score preceding IHCA was strongly associated with survival to hospital discharge and a more favorable CPC score at discharge. A smaller proportion of patients who had IHCA in the ICU survived to ROSC or hospital discharge, as compared to patients who had IHCA outside of the ICU. Importantly, this study, done following the peak of the COVID-19 pandemic, provides an updated use of the GO-FAR score as well as other clinically relevant variables during a time of heightened inpatient volume and acuity, which has only been described by one group previously.[16] This data may be a more current reflection of relevant prognostic factors for outcomes of IHCA.
It can be challenging for physicians to predict the possible outcomes of IHCA, which is important when discussing advance care plans with patients and their families.[6,17] Multiple studies have previously examined specific pre-arrest factors associated with reduced odds of ROSC and survival with good neurologic function, including male gender, age >60, body mass index, race, history of diabetes mellitus, history of arrhythmia, history of congestive heart failure, history of cancer, history of liver disease, and history of chronic kidney disease.[2,18,19] Intra-arrest factors have also previously been shown to be associated with IHCA outcomes; initial rhythm of CA (shockable), shorter duration of CA (<15 min), daytime CA, and regional cerebral oxygen saturation were correlated with increased odds of survival to discharge.[2,20-23] In this cohort, in addition to the GO-FAR score, we also found an association to survival to discharge with a shorter LOS before IHCA, shorter duration of IHCA, and non-ICU setting. However, when compared to survival to discharge with neurologic outcomes, only the GOFAR score and shorter duration of IHCA were associated to favorable neurologic outcomes at discharge. This finding was reflective of larger validation studies that demonstrated that the GO-FAR score can be a useful tool to prognosticate survival to discharge with good neurologic function after IHCA.[9] The associative information between likelihood of survival and good neurologic function on discharge may provide additional support for the use of the GO-FAR tool in clinicians’ discussions of patient goals of care in the event of cardiac arrest.
We found no associations to ROSC, survival to discharge, or survival to discharge with good neurologic function between races. Prior studies have shown differences in IHCA outcomes, with White patients having a higher likelihood of survival to discharge; however, some of these differences were attributed to hospital disparities or missing race and ethnicity data in large cardiac arrest registries.[24,25] Similarly, it is difficult for us to make more specific conclusions due to fairly small numbers of non-White patients in this study, and thus, race and ethnicity should be examined in larger registries of IHCA outcomes.
Interestingly, we found no association between initial rhythm and likelihood of survival to ROSC, hospital discharge, or survival with favorable neurologic function. Conventionally, non-shockable rhythm cardiac arrest is viewed as having a lower likelihood of survival with better neurologic function[26-28] although the majority of this data originate in out of hospital cardiac arrest, registry data for IHCA suggest an increased ROSC likelihood with shockable rhythms.[28,29] The lack of difference seen in this study population may reflect a robust IHCA response system at Cedars-Sinai which could, potentially, negate the differences conferred by type of IHCA, or it be that other measures of severity of illness (including duration of IHCA) are greater drivers of mortality in this selected patient population.
This study has several limitations. It is a relatively small, single-center experience at a major academic medical center in the US, which limits external generalizability and potentially is underpowered to detect major mortality differences, although our ROSC rates of 63% are comparable to previously reported rates of 48–52%.[25] As a retrospective chart review, data collection was limited by the information available in the electronic medical record, as well as possible selection bias although all patients who met inclusion criteria were used in analysis. Among patients who experienced IHCA multiple times, we included only the first event, and cannot exclude the impact of subsequent IHCA on outcomes. Finally, we did not include data on advance care planning, which may have affected the code status of patients during the study period and thus potentially excluded some patients with a higher likelihood of mortality. The study also has several strengths. We provided contemporary data on the function of the GO-FAR score and its potential use in prognostication. We also provided data on other factors commonly thought of as having prognostic significance during cardiac arrest, including age, duration of IHCA, day versus night at time of IHCA, location of IHCA, initial rhythm, and polypharmacy; duration of IHCA and location of IHCA had associations with IHCA and outcomes and would benefit from further studies.
Key Points
This study aims to evaluate and compare expected versus observed outcomes of IHCA. The GO-FAR score has previously been shown to be predictive of poor neurological outcomes after IHCA, but multiple recent studies have called this into question and that the calculation may need to be reexamined. We found that GO-FAR score has an association to favorable neurologic outcomes after IHCA and thus may be used as a tool by hospitalists to help and guide clinical decision making for patients with poor predicted outcomes.
CONCLUSION
This single-center retrospective cohort study found that likelihood of survival to ROSC, hospital discharge, and discharge with favorable neurologic status was associated with a shorter duration of IHCA. A lower GO-FAR score was associated with a greater likelihood of survival to discharge and discharge with a favorable neurologic status. These observations may assist clinicians with real-world prognostication and counseling during advance care planning for hospitalized patients and may lead to improved patient care and goal-concordant care.
Ethical approval:
The research/study approved by the Institutional Review Board at Cedars-Sinai Medical Center IRB, number 00002119, dated 05th October 2022.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- Incidence of Treated Cardiac Arrest in Hospitalized Patients in the united states. Crit Care Med. 2011;39:2401-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pre-arrest and Intra-arrest Prognostic Factors Associated with Survival after In-hospital Cardiac Arrest: Systematic review and meta-analysis. BMJ. 2019;367:l6373.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective Validation of the Good Outcome Following Attempted Resuscitation (Go-far) Score for In-hospital Cardiac Arrest Prognosis. Resuscitation. 2019;140:2-8.
- [CrossRef] [PubMed] [Google Scholar]
- Heart Disease and Stroke Statistics-2018 Update: A Report from the American Heart Association. Circulation. 2018;137:e67-492.
- [CrossRef] [Google Scholar]
- Neurophysiological and Neuroradiological Test for Early Poor Outcome (cerebral Performance Categories 3-5) Prediction after Cardiac Arrest: Prospective Multicentre Prognostication Data. Data Brief. 2019;27:104755.
- [CrossRef] [PubMed] [Google Scholar]
- Are Providers Overconfident in Predicting Outcome after Cardiac Arrest? Resuscitation. 2020;153:97-104.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicians' Approach to Predicting Post-cardiac Arrest Outcomes for Patients Enrolled in a United States Clinical Trial. Resuscitation. 2024;199:110226.
- [CrossRef] [PubMed] [Google Scholar]
- Physicians' Cognitive Approach to Prognostication after Cardiac Arrest. Resuscitation. 2022;173:112-21.
- [CrossRef] [PubMed] [Google Scholar]
- Development and Validation of the Good Outcome Following Attempted Resuscitation (Go-far) Score to Predict Neurologically Intact Survival After In-hospital Cardiopulmonary Resuscitation. JAMA Intern Med. 2013;173:1872-8.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of the good Outcome Following Attempted Resuscitation Score on In-hospital Cardiac Arrest in Southern Sweden. Int J Cardiol. 2016;221:294-7.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of the Good Outcome Following Attempted Resuscitation (Go-far) Score in An East Asian Population. Resuscitation. 2020;150:36-40.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting Neurologically Intact Survival after In-hospital Cardiac Arrest-external Validation of the Good Outcome Following Attempted Resuscitation Score. Resuscitation. 2018;128:63-9.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting Outcomes of In-hospital Cardiac Arrest: Retrospective us Validation of the Good Outcome Following Attempted Resuscitation Score. J Gen Intern Med. 2019;34:2530-5.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting the Probability of Survival with Mild or Moderate Neurological Dysfunction after In-hospital Cardiopulmonary Arrest: The Go-far 2 Score. Resuscitation. 2020;146:162-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pre-arrest Prediction of Survival Following Inhospital Cardiac Arrest: A Systematic Review of Diagnostic Test Accuracy Studies. Resuscitation. 2022;179:141-51.
- [CrossRef] [PubMed] [Google Scholar]
- Survival of In-hospital Cardiac Arrest in Covid-19 Infected Patients. Healthcare (Basel). 2021;9:1315.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic Models for Outcome Prediction Following In-hospital Cardiac Arrest using Pre-arrest Factors: A Systematic Review, Meta-analysis and Critical Appraisal. Crit Care. 2023;27:32.
- [CrossRef] [PubMed] [Google Scholar]
- Lactate and Hypotension as Predictors of Mortality after In-hospital Cardiac Arrest. Resuscitation. 2021;158:208-14.
- [CrossRef] [PubMed] [Google Scholar]
- Factors of Importance to 30-day Survival after In-hospital Cardiac Arrest in Sweden-A Population-Based Register Study of More than 18,000 Cases. Int J Cardiol. 2018;255:237-42.
- [CrossRef] [PubMed] [Google Scholar]
- Regional Cerebral Oxygen Saturation During Cardiopulmonary Resuscitation as a Predictor of Return of Spontaneous Circulation and Favourable Neurological Outcome-A Review of the Current Literature. Resuscitation. 2018;125:39-47.
- [CrossRef] [PubMed] [Google Scholar]
- In-hospital Cardiac Arrest: The State of the Art. Crit Care. 2022;26:376.
- [CrossRef] [PubMed] [Google Scholar]
- Pre-arrest Predictors of Failure to Survive after In-hospital Cardiopulmonary Resuscitation: A Meta-analysis. Fam Pract. 2011;28:505-15.
- [CrossRef] [PubMed] [Google Scholar]
- The Effect of Missing Data on the Measurement of Cardiac Arrest Outcomes According to Race. Prehosp Emerg Care. 2022;27:1054-7.
- [CrossRef] [PubMed] [Google Scholar]
- Survival After Out-of-hospital Cardiac Arrest: The Role of Racial Residential Segregation. J Urban Health. 2022;99:998-1011.
- [CrossRef] [PubMed] [Google Scholar]
- Temporal changes in the racial gap in survival after inhospital cardiac arrest. JAMA Cardiol. 2017;2:976-84.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic Implications of Conversion from Nonshockable to Shockable Rhythms in Outof-hospital Cardiac Arrest. Crit Care. 2014;18:528.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of Favorable and Poor Prognosis in Unwitnessed Out-of-hospital Cardiac Arrest with a Non-shockable Initial Rhythm. Int J Cardiol. 2014;176:910-5.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Associated with Shockable Versus Non-shockable Rhythms in Patients with In-Hospital Cardiac Arrest. Resuscitation. 2021;158:166-74.
- [CrossRef] [PubMed] [Google Scholar]






