Translate this page into:
Double Valve Replacement in the Pregnant Patient: A Successful Case and Brief Literature Review
*Corresponding author: Bhavna P. Singh, Department of Critical Care, Narayana Institute of Cardiac Sciences, Bengaluru, Karnataka, India. bhavna.p.singh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sneha N, Singh BP, Alva A. Double Valve Replacement in the Pregnant Patient: A Successful Case and Brief Literature Review. J Card Crit Care TSS. 2025;9:126-9. doi: 10.25259/JCCC_61_2024
Abstract
Cardiovascular disease is the leading cause of maternal mortality accounting for >25% of maternal deaths. The risk of cardiac surgery is very high with poor neonatal outcomes. The authors would like to report a patient who was a 19 year old lady with 27 weeks gestation who had severe mitral stenosis (mitral valve area-0.9cm2, pulmonary artery systolic pressure (PaSP-90mm Hg)), moderate mitral regurgitation, moderate aortic stenosis with severe aortic regurgitation, (modified world health organization class (m WHO) class IV) who successfully underwent double valve replacement under cardiopulmonary bypass (CPB) and went on to deliver a healthy but premature male baby. Cardiac surgery especially cardiopulmonary bypass is high risk procedure when needed to be performed must be done in second trimester of prgnancy. The authors have divided the discussion into 4 parts for ease of discussion i.e Anesthetic, surgical, intensivist and perfusion related considerations. Anesthetic considerations included maintaining uteroplacental perfusion, higher cardiac index other considerations of pregnancy including low systemic vascular resistance, difficult airway, lateral tilt. Surgical considerations include minimizing cross clamp and bypass time to avoid fetal complications. Post operatively intensivist considerations include hemodynamic monitoring with regular point of care ultrasound (POCUS) for fluid management. Vasopressor and fluid management in our case was tailored to the Flo Trac (cardiac output) monitoring system and POCUS assessments. The patient had a successful outcome however delivered a premature baby at 33 weeks gestation. The incidence of premature delivery is about 50% as per literature review. The literature around cardiac bypass in pregnancy is limited and we hope that our case adds to further research on this topic.
Keywords
Cardiopulmonary bypass in pregnancy
Double valve replacement in pregnancy
Fetal consideration on cardiopulmonary bypass
INTRODUCTION
Cardiovascular disease is the leading cause of maternal mortality accounting for >25% of maternal deaths; however, the risk of cardiac surgery is very high with poor neonatal outcomes.[1] The risk of cardiac surgery, especially in a pregnant woman, is very high both for the fetus and the mother. Here, the authors report a patient with a mWHO class IV heart disease who successfully underwent double valve replacement under cardiopulmonary bypass (CPB) and went on to deliver a healthy but premature male baby.
CASE REPORT
A gravida 1 para 0 living 0 abortion 1 patient presented to our center at 27 weeks of gestation with breathlessness of New York Heart Association (NYHA) IV severity. She was diagnosed to have rheumatic heart disease 5 years ago with shortness of breath (NYHA II) and eventually progressed to NYHA IV symptoms. Although she was advised of surgery, the patient had deferred and presented to author’s center.
Her echocardiogram showed severe mitral stenosis (0.9 cm2) with moderate mitral regurgitation, severe pulmonary hypertension pulmonary artery systolic pressure 90 mmHg, and moderate aortic stenosis with severe aortic regurgitation, which qualifies as a World Health Organization category IV heart disease.
She was initially medically managed as acute valvular heart failure with low dose of diuretics, bilevel non-invasive positive pressure ventilation, and vasopressor support. After stabilization, she was deemed a candidate for double valve replacement by the surgical team. After a multidisciplinary discussion with a cardiologist, cardiac surgeon, intensivist, and obstetrician, she was taken up for surgery with high risk. Medical management was continued to ensure the patient reached the second trimester, which is the ideal time for surgery in the pregnant patient. Steroid was administered for lung maturity and left uterine displacement was used throughout surgery to maintain uteroplacental perfusion. Her target mean arterial pressure was maintained above 70 mmHg for which an advanced cardiac output monitoring system (FloTrac) was used and target hemoglobin value was 11 g/dL. Fetal monitoring included non-stress test and cardiotocometry both intra and postoperatively to assess fetal well-being and identify premature uterine contractions with a qualified obstetrician present throughout surgery and available in proximity postoperatively. Normothermic pulsatile CPB was used with the total duration of surgery being 6.5 h and CPB time being 1.5 h. Four packed red blood cells, fresh frozen plasma, and albumin were used during the surgery, and electrolytes and serial arterial blood gas were done and maintained within normal limits by sodium bicarbonate, magnesium, and potassium infusions. Vasopressors including noradrenaline, adrenaline, and dopamine were used to target mean arterial pressure (MAP) of 70 mmHg. Tocolytics including terbutaline were kept on standby however were not used as the obstetric monitoring was uneventful. She was transferred to the post-surgical intensive care unit (ICU) on ventilator, regular point of care ultrasound (POCUS) was used to assess fluid status [[Figures 1 and 2], and vasopressor support was titrated accordingly. For elevated pulmonary artery pressures Dobutamine was used for the first 24 hours as it is short acting in its pharmacokinetics. This was followed by milrinone for next 48 hours. Throughout the perioperative period the patients Mean arterial pressure was maintained at 70 mm Hg and Partial pressure of oxygen (PaO2) was maintained between 80-90 mm Hg. This was done using the FloTrac cardiac output monitoring system. On post-operative day 1, she was extubated and bedside ultrasonography showed a slight reduction in amniotic fluid for which diuretics were withheld, and anticoagulation was maintained with low-molecular-weight heparin and bridged to warfarin for a target INR of 2.5–3.5. Fetal monitoring was further continued even through the postoperative period. Through follow-up, we learned that the patient had delivered a baby boy through cesarean section at 33-week gestation without any major congenital abnormalities; however, her pregnancy was complicated by intrauterine growth retardation, non-reassuring non stress test (NST), and absent end-diastolic flow leading to premature delivery.
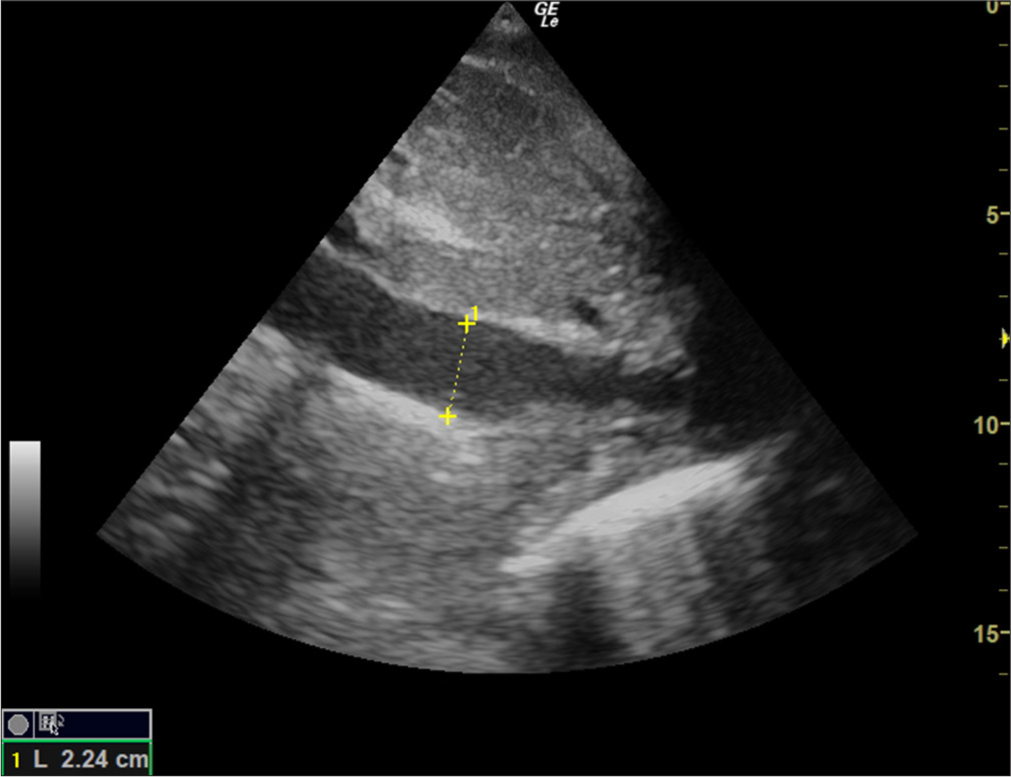
- Subcostal view of the inferior vena cava during inspiration on positive pressure ventilation. The yellow dotted line is the length as measured which is 2.24 cm.
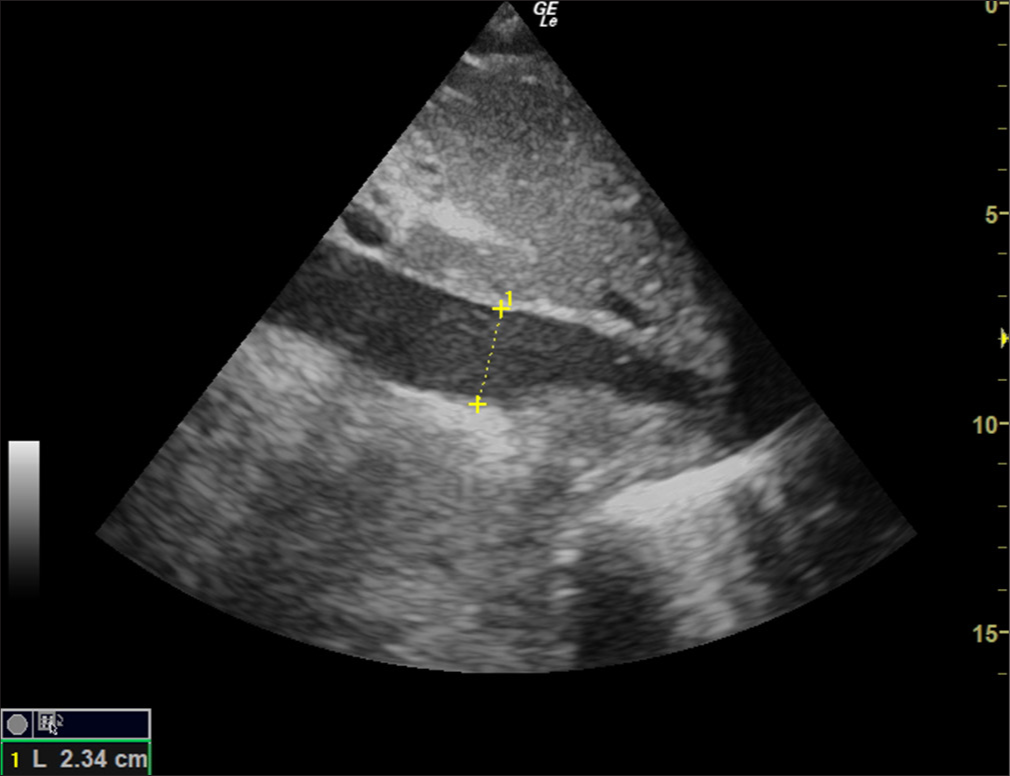
- Subcostal view of inferior vena cava on expiration during positive pressure ventilation. The yellow dotted line is the length as measured which is 2.24 cm.
DISCUSSION
Heart disease complicates around 1% of pregnancies with rheumatic being the etiology in over 60% of the cases frequently presenting with mitral and aortic valvular disease in our country.[2]
We have divided the discussion into 4 parts anesthetic, surgical, intensivist, and perfusion considerations.
Anesthetic considerations
A recent review in circulation highlighted the need for specialized cardio-obstetric anesthesia services.[3] Women with heart disease are stratified based on the mWHO class, our patient was mWHO class IV, where ideally, she should not have planned pregnancy as mortality is extremely high due to a fixed low cardiac output state in the setting of low systemic vascular resistance (SVR) of pregnancy risking heart failure, arrhythmias, and transfusion-related risks. Anesthetic goals include avoiding hypertension/hypotension with a mean arterial pressure target more than 70 mmHg to maintain uteroplacental perfusion, to choose vasopressor medications with chronotropic and inotropic properties, limit iv fluids to avoid fluid overload, and maintain a good hematocrit closer to 10 g/dL. Intraoperative monitoring includes transesophageal echocardiography, which is used intermittently to assess the valves and pulmonary artery pressure. Additional considerations include maintaining PaO2 between 85-110 mm Hg, PaCO2 between 35-45 mm Hg and normal acid-base status without either acidosis or alkalosis.[4] An intraoperative obstetrician is present to deliver the fetus if there is persistent fetal bradycardia detected on non-stress test monitor and cardiotocography of fetus. Other pregnancy considerations, such as lateral tilt and difficult airway preparation, must be made but those are beyond the scope of the current report.
Surgical considerations
The indications for surgery are based on severity of symptoms and the risk of surgery is stratified by the mWHO classification. Principal considerations are same as any other surgery in pregnant patients, namely avoiding fetal hypoxia and preventing premature contractions. While medical management is preferred, our patient was severely symptomatic with a fixed output state and hence was planned for surgery. When planned, the surgery is best done in the second trimester. Surgical considerations include minimizing cross-clamp and bypass time with normothermic pulsatile bypass preferred to maintain uteroplacental perfusion and avoid fetal complications.[5] Prenatal corticosteroids were administered for lung maturity in case the fetus needs to be delivered.
Intensivist considerations
Regular cardiac surgical postoperative care includes hemodynamic monitoring, maintaining adequate mean arterial blood pressure, extubation of the patient when appropriate, ventilator management, and metabolic parameter monitoring. In addition to these, pregnant women need left lateral tilt, extubation is at higher risk because of difficult airway, continuous non-stress test with cardiotocography must be continued in the ICU with obstetrician backing for urgent delivery; in case, there are signs of fetal distress. Here, uteroplacental perfusion maintenance is of utmost importance. Higher hematocrit but avoidance of fluid overload is found to be beneficial. Drugs such as sodium nitroprusside must be avoided due to placental transfer. Vasopressors again must be used with caution due to the risk of uteroplacental hypoperfusion.[4] In addition to usual care of monitoring, our tertiary ICU has an ultrasound machine which was used to identify the fetal heart rate and regular POCUS examinations were performed.
Perfusion team considerations
The effect of CPB is more on the fetus than on the pregnant woman.[3] Pregnant women are known to tolerate CPB as well as non-pregnant women.[6] CPB compromises uteroplacental perfusion, releases vasoactive mediators from leucocytes, and activates the complement pathway. There is also a risk of air embolism and alterations of the coagulation pathway leading to intrauterine clotting or bleeding episodes. The non-pulsatile flow of CPB with hypothermia and hypotension can further risk the fetus causing fetal loss.[7] The uterine hypoperfusion and fetal hypoxia can trigger uterine contractions.[8]
Fetal bradycardia can be intermittent or can continue postoperatively. Placental circulation is not autoregulated leading to drop in perfusion with maternal blood pressure changes causing a high fetal mortality up to 30%.[9]
Hemodilution is deleterious to the fetus; hence, blood prime is used. Heparin requirements are higher due to the prothrombotic state induced by pregnancy. Cardioplegia requirement may be higher which in turn leads to higher potassium that needs close monitoring. Normothermic bypass with pulsatile flow is better for maintaining placental perfusion.[10] We used normothermic cardioplegia with St Thomas solution with 1 packed red cell for priming. Pulsatile perfusion was established after cross-clamp application until cross-clamp release and cardioplegia were administered approximately every 20 min. Serial blood gases showed mild acidosis which was corrected using sodium bicarbonate solution. Cardiovascular health in women, which is effective in the prevention of cardiovascular disease (CVD), should be promoted worldwide, with great efforts in overcoming the still existing disparity. The goal set could be achieved by greater educational information about the importance of CVD in women by the definition of diagnostic and treatment algorithms peculiar to women, greater socioeconomic integration, and improved interdisciplinary and cooperative care.[11]
CONCLUSION
CPB is a high-risk procedure whose risk exponentially increases with pregnancy. Our patient needed surgery due to persistent and progressive symptoms. In summary, it is possible to perform cardiac surgery on CPB in pregnancy if clinically indicated in a tertiary care setting without complications if the risk is ascertained and preparation is done accordingly. In our center, we followed the basic anesthesia safeguards in pregnancy with additional adjustments by the perfusion team while our surgeons minimized the bypass and cross-clamp time. While the patient did well and was discharged on post operative day 9 (POD9), she had a premature delivery at 33 weeks due to uteroplacental insufficiency. The baby boy was in neonatal ICU for 1 week and discharged alive and healthy. The incidence of premature delivery in patients who continue pregnancy after cardiac surgery is nearly 50%. The literature on cardiac bypass in pregnancy is limited and we hope that our case adds to a series or literature review.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Pregnancy-related Mortality in the United States 2011-2013. Obstet Gynecol. 2017;130:366-73.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy Outcomes in Women with Heart Disease: The Madras Medical College Pregnancy and Cardiac (M-PAC) Registry from India. Eur Heart J. 2023;44:1530-40.
- [CrossRef] [PubMed] [Google Scholar]
- ACOG Practice Bulletin No. 212 Pregnancy and Heart Disease. Obstet Gynecol. 2019;133:e320-56.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Surgery During Pregnancy. Ann Thorac Surg Short Rep. 2023;1:203-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Operation Under Cardiopulmonary Bypass During Pregnancy. J Cardiothorac Surg. 2020;15:92.
- [CrossRef] [PubMed] [Google Scholar]
- Indications for Cardiopulmonary Bypass During Pregnancy and Impact on Fetal Outcomes. Geburtshilfe Frauenheilkd. 2014;74:55-62.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiopulmonary Bypass During Pregnancy. Ann Thorac Surg. 1996;61:1865-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Surgery Under Cardiopulmonary Bypass in Pregnancy: Report of Four Cases. J Cardiothorac Surg. 2021;16:268.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Operations During Pregnancy: Review of Factors Influencing Fetal Outcome. Ann Thorac Surg. 2000;69:1622-6.
- [CrossRef] [PubMed] [Google Scholar]
- Women's Cardiac Health in 2020: A Systematic Review. J Card Crit Care TSS. 2020;4:104-10.
- [CrossRef] [Google Scholar]






