Translate this page into:
Continuous Erector Spinae Plane Block in Patients with Failed Epidural
*Corresponding author: Prasanta Kumar Das, Department of Anaesthesiology All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. docdas.aiims@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadavilli K, Das PK, Rao P, Mohanty S. Continuous Erector Spinae Plane Block in Patients with Failed Epidural. J Card Crit Care TSS. 2024;8:239-41. 10.25259/JCCC_30_2023
Abstract
Pain following thoracotomy is severe and requires adequate analgesia for better postoperative recovery. Epidural analgesia is considered the gold standard for thoracotomy pain. A newer ultrasound-guided analgesic technique, erector spinae plane block, has multidermatomal sensory block. We report two cases, for which an ultrasound-guided continuous erector spinae plane block was given using an 18G catheter. Both the patients received a continuous local anesthetic infusion for 48 hours and were pain-free. Erector spinae plane block can be a suitable alternative for analgesia in patients with failed epidural or contraindication to epidural analgesia.
Keywords
Thoracotomy
Analgesia
Erector spinae plane block
Regional analgesia
Ultrasound
INTRODUCTION
Pain following thoracic procedures is one of the most severe, and it negatively influences the chest wall mechanism, preventing adequate chest physiotherapy and recovery.[1] Thoracic epidural analgesia (TEA) is considered the gold standard even today as it has superior analgesia compared to systemic opioids.[2] Erector spinae block (ESPB) is a novel ultrasound-guided analgesic technique with a multidermatomal sensory block.[3] It is a suitable alternative to TEA due to lesser adverse effects and minimal intensive care unit (ICU) stay.[4] We describe two cases of continuous ESPB for postoperative analgesia in patients undergoing thoracotomy.
CASE SERIES
Case 1
A 48-year-old female presented with a complaint of shortness of breath and pain in the chest for the past three years. She is a known diabetic and hypertensive on telmisartan 40 mg. Her laboratory investigations were normal. High-resolution computed tomography (HRCT) is suggestive of a hydatid cyst in the left lower lobe. Pulmonary function test showed forced vital capacity (FVC) at 99%, forced expiratory volume in 1 s (FeV1) at 86%, and FeV1/FVC at 88%, and bronchoscopy showed no abnormality in the bronchial tree. She was scheduled for a hydatid cyst excision.
On the day before surgery, pre-anesthetic advice was given. The patient was explained about epidural analgesia, and consent was taken. Inside the operating theater, monitors were connected, IV cannulation was done, and an invasive arterial line was taken. Epidural catheterization was planned but could not be done as the catheter could not be threaded into the epidural space. Hence, we decided to proceed with ESPB with a catheter. Under ultrasound guidance, the Tuohy needle was introduced at the T5–T6 level on the left side, and the erector spinae plane was identified between the erector spinae muscle and the transverse process. A bolus dose of 0.25% ropivacaine 20 mL was given, and an 18G epidural catheter was threaded. The patient was induced with fentanyl, propofol, and vecuronium as per standard institutional protocol and intubated with 35 Fr left-sided double lumen tube (DLT). Mechanical ventilation was instituted, and lung isolation was done.
0.125% ropivacaine was started as an infusion in the ESP catheter at five mL/h. Intraoperative hemodynamics were stable. At the end of the surgery, DLT was exchanged with a 7.0 mm ID ETT, and the patient was shifted to ICU.
Two hours after mechanical ventilation, the patient was extubated. The pain score after extubation was 1/10. An infusion of 0.125% ropivacaine at five mL/h was continued. Hemodynamics were stable. On the postoperative day (POD) 1, the morning pain score is 2/10 at rest and 3/10 on movement. Ropivacaine infusion was continued for 48 h, and the patient was pain free.
Case 2
A 36-year-old male, a smoker and alcoholic with a history of pulmonary tuberculosis ten years back, complained of a productive cough for the past two years and breathlessness for six months. The patient is known to be hypertensive on amlodipine 10 mg. On auscultation, breath sounds were decreased on the right. The rest of the clinical examination is insignificant. His chest X-ray showed mild opacities in the right upper zone. HRCT thorax is suggestive of aspergilloma. He was scheduled for the right upper segmentectomy.
The pre-anesthetic evaluation was done, and his laboratory investigations were within normal limits. Spirometry showed a restrictive pattern (FVC 69%, FeV1 68%, and FeV1/FVC 100%). Bronchoscopy showed a normal bronchial tree. On the night before surgery, routine pre-operative advice was given. The patient was explained about the ESPB, and consent was taken.
Inside the operating theater, monitors were connected, IV cannulation was done, and an invasive arterial line was taken. Under ultrasound guidance, the Tuohy needle was introduced in the erector spinae plane on the right side at the T5–T6 level between the erector spinae muscle and the transverse process [Figure 1]. A bolus dose of 0.25% ropivacaine 20 mL was given, and an 18G epidural catheter was threaded. The patient was induced with fentanyl, propofol, and vecuronium as per the standard institutional protocol and intubated with 39 Fr left-sided DLT. Mechanical ventilation was instituted, and lung isolation was done.
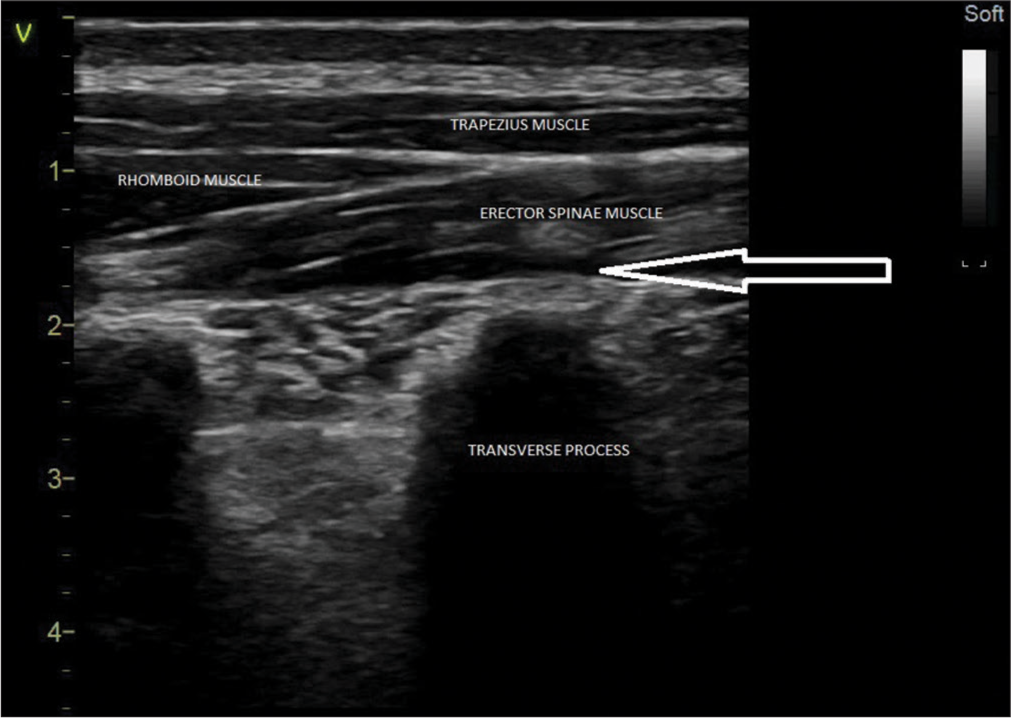
- Erector spinae plane above the transverse process and below the erector spinae muscle (arrow). Also seen are trapezius and rhomboid muscles.
0.125% Ropivacaine was started as an infusion in the ESP catheter at five mL/h. Intraoperative hemodynamics were stable. At the end of the surgery, DLT was exchanged with an 8.0 mm ID ETT and shifted to the ICU.
Two hours after mechanical ventilation, the patient was extubated. The patient did not complain of pain, and a score of numerical rating scale (NRS) 3/10 was present on questioning. 0.125% Ropivacaine infusion at five mL/h was continued. Hemodynamics were stable. On POD-1, the morning pain score is 2/10 at rest and 4/10 on movement. Ropivacaine infusion was continued for 48 hours, and the patient was pain-free.
DISCUSSION
Postoperative pain following thoracotomy is one of the most severe pain, which may persist for many months, worsening the quality of life.[1] Good analgesia improves cough, depth of breathing, and expectoration, reducing retention of secretions, atelectasis, and respiratory failure. Epidural analgesia provides superior analgesia to systemic opioids, making it the gold standard.[1,2] However, there is risk of spinal hematoma with neuraxial blockade if the patient is under anticoagulation. Hence, anticoagulants must be withheld before performing neuraxial blockade and for removal of epidural catheters.[5,6]
Alternatives include paravertebral block when coagulopathy is a concern, which has some side effects such as hypotension and bradycardia. Systemic analgesia with opioids can be given, but the potential side effects, such as respiratory depression, make it a less suggested alternative.[2] An intercostal nerve block is highly effective but only feasible as a single-shot block.[7]
ESPB is a novel ultrasound-guided technique associated with a multidermatomal sensory block. Local anesthetic deposited in the fascial plane deeper to the erector spinae muscle at the tip of the transverse process of the vertebra results in cephalocaudal spread from 3 to 9 spaces within the erector spinae muscles, neural foramina, and into the epidural space.[8] The site of action is at the dorsal and ventral ram of thoracic spinal nerves.[3] This provides analgesia to the posterior hemithorax, ribs, periosteum, sand lateral, and anterior chest wall.[9] It can be given as a single shot or continuous technique with a catheter. The absence of major blood vessels and neural structures in the vicinity minimizes concerns of developing a significant hematoma, even in the presence of anticoagulation.[7] It is associated with lesser adverse effects and early mobilization following open thoracic surgeries, making it a suitable alternative to TEA.[4]
CONCLUSION
ESPB is a novel ultrasound guided technique for analgesia which can be an effective alternative to TEA for thoracic surgeries with fewer adverse effects.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Preventing and Treating Pain after Thoracic Surgery. Anesthesiology. 2006;104:594-600.
- [CrossRef] [PubMed] [Google Scholar]
- The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med. 2016;41:621-7.
- [CrossRef] [PubMed] [Google Scholar]
- Abstract No: ABS2374: Comparison of Erector Spinae Block Versus Thoracic Epidural Anaesthesia for Post-operative Pain Management in Adult Patients Undergoing Thoracotomy. Indian J Anaesth. 2022;66:S3.
- [Google Scholar]
- Regional Anesthesia in the Anticoagulated Patient: Defining the Risks (the Second ASRA Consensus Conference on Neuraxial Anesthesia and Anticoagulation) Reg Anesth Pain Med. 2003;28:172-97.
- [CrossRef] [PubMed] [Google Scholar]
- Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition) In: Reg Anesth Pain Med. Vol 43. 2018. p. :263-309.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous Erector Spinae Plane Block for Rescue Analgesia in Thoracotomy after Epidural Failure: A Case Report. A A Case Rep. 2017;8:254-6.
- [CrossRef] [PubMed] [Google Scholar]
- A Magnetic Resonance Imaging Study of Local Anesthetic Spread in Patients Receiving an Erector Spinae Plane Block. Can J Anaesth. 2020;67:942-8.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound Guided Erector Spinae Plane Block Versus Thoracic Epidural Analgesia in Traumatic Flail Chest, a Prospective Randomized Trial. J Anaesthesiol Clin Pharmacol. 2023;39:250-7.
- [CrossRef] [PubMed] [Google Scholar]







