Translate this page into:
A Cardiac Surgeon’s Magnified Views – The Loupe
*Corresponding author: Doniparthi Pradeep, Department of Pediatric and Congenital Heart Surgery, Fortis Escorts Heart Institute, New Delhi, India. pradeepdhoni023.pd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chittimuri C, Pradeep D. A Cardiac Surgeon’s Magnified Views – The Loupe. J Card Crit Care TSS. 2025;9:137-40. doi: 10.25259/JCCC_57_2024
Dear Editor,
For cardiac surgeons in their primordial phase, mornings begin early with a symphony of alarms and sterile suits and continue with the magnified world glimpsed through the loupe and occasional blood showers. The authors delve into the kith and kin of the loupe, exploring its history and optical principles within the realm of cardiac surgery, which is one of the most important chunks of the cardiac surgery armamentarium. Although the history of optical devices and principles is vast, the authors focused firmly only on the optics related to loupes in cardiac surgery, not beyond that.
BRIEF HISTORY OF APPLIED OPTICS
The utilization of optics in daily activities predates the Roman empire; however, the earliest documented evidence of its application emerged during this historical period.
TELESCOPES AND LOUPES
A telescope comprises a series of lenses designed to enlarge the apparent size of objects observed through it. Conversely, a loupe embodies a lens system where two telescopic units are mounted onto a framework, enabling binocular vision and enhancing depth perception during visual examination.
Lippershey and Janssen independently placed two lenses within a sliding system in 1590. It was the first invention of a telescope. Tuscan physicist Galileo Galilei, in 1610, made his telescope with the modification of Lippershey’s telescope with the use of convex objective and concave eyepieces, with higher optical power. This gave him the opportunity to observe the universe, solar system, and ultimately landed up in house arrest, which is known to everyone. In contemporary times, German physicist Johannes Kepler in 1611 modified Galileo’s telescope design by replacing the concave lens with a convex lens. Kepler’s modification inverted the image but provided a wider field of vision (FOV) than Galileo’s system [Figure 1].
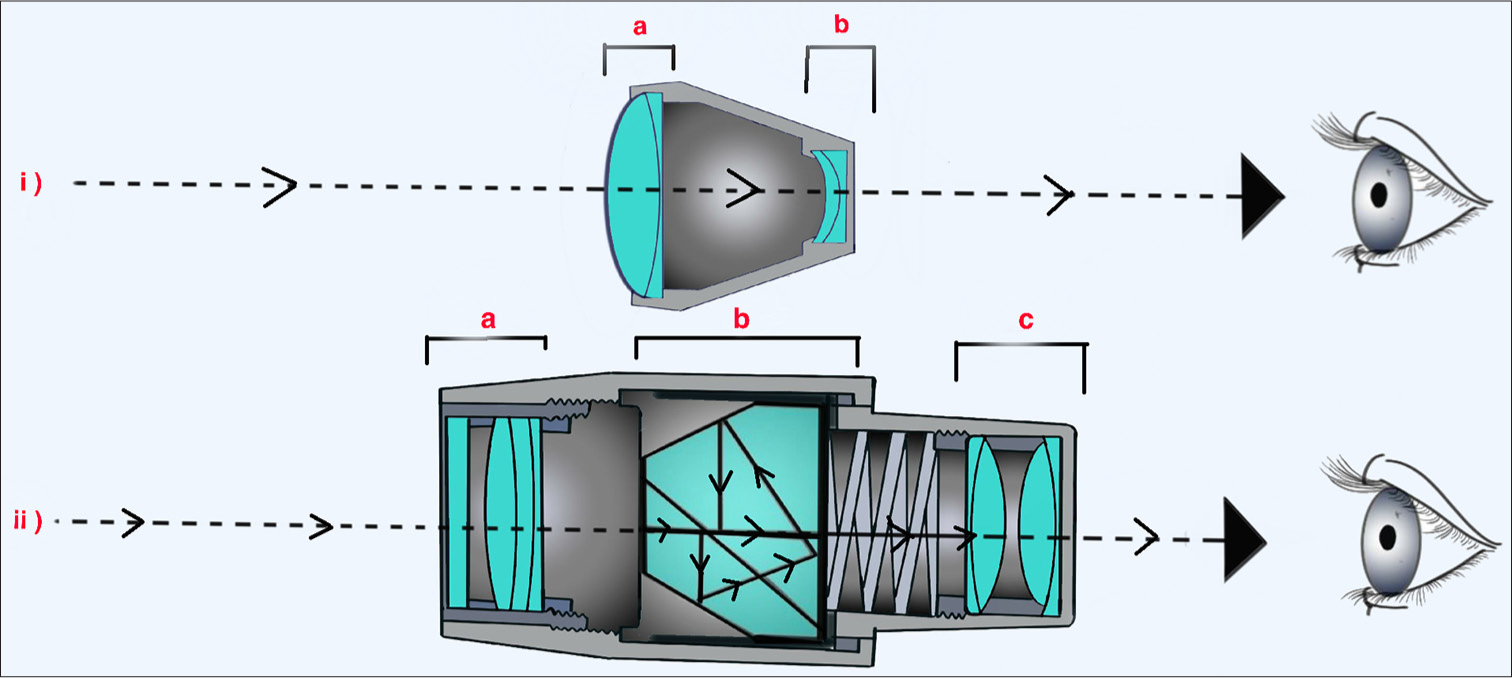
- Optics of the (i) Galilean and (ii) Keplerian systems of telescopes: (a) Objective lenses, (b) Eyepiece lenses, (c) Prismatic lenses rotate the trajectory of the light.
The loupes were first designed by Parisian optician Charles Louis Chevalier in the 1840s. He has fashioned a loupe with a magnification of ×6. The ophthalmic surgeon, Edwin Theodore Saemisch of Bonn, made the first simple loupe for surgical practice in 1876. Carl Wilhelm Von Zehender, an ophthalmology professor, gave an account of a new compound binocular device in 1886 in the journal “Klinische Monatsblatter fur Augenheilkunde,” of which he was the editor and called this device “Binokulare Cornealupe,” designed by Heinrich Westien. Westien later mounted Von Zehender’s device on a headband with a light source. It had a magnification power of 5-6-fold but was not well received because of its heavy weight. In 1912, Moritz Von Rohr of Jena fashioned a much lighter loupe, which would be manufactured by Carl Zeiss, Inc. and gained popularity despite having low magnification.[1]
If the usage of the loupes or microscopes in cardiac surgery is seen, it was the popular teaching that the arteries of <7 mm size could not be anastomosed successfully. However, a groundbreaking moment occurred in 1960 at the University of Vermont when Dr. Julius H Jacobson achieved the successful anastomosis of a 2 mm blood vessel, facilitated by a Carl Zeiss-designed microscope. He had experimented in denervated canine carotid arteries for pharmacological experiments. Dr. George E Green was successful in canine coronary anastomosis experiments, showing the patency of the anastomosis with a diameter of 1 mm aided by an operating microscope of ×16 magnification and monofilament Nylon 9-0 suture. He also did the first human coronary anastomosis in 1968 with the aid of an operating microscope. Probably, this was the first usage of optics in cardiovascular surgery. Every cardiac surgeon is familiar with the pioneering work of Cleveland Clinic in coronary bypass surgery. In Cleveland Clinic, the chief of thoracic surgery, Dr. Don Effler and Dr. Rene G Favaloro, had non-satisfactory results in the beginning, following which Dr. Rene G Favaloro came across the promising results achieved with a microscope and the need for 100 h laboratory training to use the same. Dr. Don Effler approached Dr. Julius H Jacobson in Burlington, spent a week, and learned to anastomose the arteries of 1-mm diameter. Dr. Julius H Jacobson sent his senior laboratory fellow to the Cleveland Clinic to aid in the training of staff. Moreover, the rest is history.[2-6]
There are two vital parts in any loupe. One is the telescope system, and the other is the mount. Two telescopes are mounted on either a spectacle frame or a head mount [Figure 2]. Aside from these important parts, other customized parts, such as the headlight for better illumination and the camera record or display the real-time procedure on the screen. Based on the optics of the lens systems, loupes are broadly classified [Table 1] into two types.[7]

- Cardiac surgeon in surgical attire, wearing vascular loupes and headlight.
| S. No. | Galileo’s system | Kepler’s system |
|---|---|---|
| 1 | Two-lens system: Objective convex lens and concave eyepiece lens | Two or more convex lens systems, with a prism in between. |
| 2 | Lens system forms an upright image | Lens system forms an inverted image. Inclusion of the prism makes the image upright |
| 3 | For low magnification power | For high magnification power |
| 4 | Light source is not mandatory | Light source is essential |
| 5 | Smaller in size and lighter in weight but provides a smaller field of vision and shorter working distance. | The prisms extend the light path, which in turn increases the magnification depth and provides a longer working distance |
| 6 | Inexpensive due to their simpler design. | Expensive due to their complex design |
Based on the design, loupes can be divided into two types: Through-the-lens (TTL) and front lens mounted (FLM) or flip-up loupes. In TTL loupes, the ocular barrels of the telescope systems are drilled, mounted, and secured directly into the carrier lenses; hence, TTL loupes are lighter than their counterparts. TTL loupes are fully customizable and are personalized to satisfy the specific visual and comfort needs of the surgeon. These TTL loupes provide a wider FOV and the steeper angle of declination (the angle between the reference line that connects the top of the ears to the corner of the eyes and the optical axis of loupe oculars). Flip-up loupes are a type of loupe with ocular barrels of telescope that are attached to the frame through a hinge mechanism. Owing to the added weight of the hinge mechanism and protruding position of the ocular barrels of the telescope systems, FLM loupes tend to be heavier than TTL loupes. FLM loupes offer a flexible angle of declination and adjustable interpupillary distance and, hence are easily adjusted for multiple users and variable working distances (WDs). Adding and changing prescriptions for refractive errors are also easier with flip-up loupes.
PROPERTIES OF LOUPE
Magnification and resolution
Magnification is the ability to make small objects seem larger and resolution is the ability to distinguish two objects from each other precisely. Magnification depends on the focal length of the system and resolution depends on the refractive index of the system. The magnification power is chosen based on the surgeon’s personal preference and the procedures they perform. A higher magnification power limits the FOV. Adequate magnification allows the surgeon and assistants to work from an optimal distance, which provides ergonomic balance.[8,9] This allows the team to see the operating field and suture material closely and precisely. The magnification of the loupe is entirely a personal preference. The lowest magnification allows the viewer to see a larger FOV. For a trainee cardiac surgeon, a magnification of 2.5 times (×2.5) is advised. For adult cardiac surgeries, magnification of ×2.5–×3.5 is advised and for coronaries and congenital heart surgeries, above ×3.5 is usually advised. For magnifications more than ×6.0 surgical loupes are usually not recommended and an operating microscope is a better choice.
Working distance (WD)
In practical scenarios, when the surgeon is operating, the back should be straight and the surgeon should not lean forward to obtain a clear surgical field. WD is the distance between the eyes of the surgeon and the actual procedural site. When the magnification power increases, the WD increases hand in hand. In common scenarios, for a loupe of ×2.5 magnification, WD is 340 mm; for ×3.0 magnification, WD is 420 mm; and for ×3.5 magnification, WD is 500 mm.
Illumination
The higher the magnification, the less light can enter the eye, which mandates extra lightening. When the surgeon uses an extra light source, the surgeon’s pupil will naturally dilate, which diminishes the depth of field when using a loupe. That is why a light source is mandatory when using higher magnification loupe systems, exclusively Kepler’s system, either by an inbuilt light source on the frame of the spectacle or a separate headlight. Additional light sources should be moderately intense. Light that is too bright can shut the rods and render them useless; light that is too dim will not be able to keep up as magnification increases.
Weight of the loupe
For better comfort, a loupe should be lightweight and the weight should be uniformly distributed. It avoids discomfort and headache. It should not render any scar over the nasal bridge.
Prescription needs
Loupes are available with built-in prescription lenses for surgeons with refractive errors. Alternatively, they can wear contact lenses while wearing a non-prescription loupe.
Ergonomics of the body
Ergonomic posture is not a natural posture. It is the instinct to tilt the head and twist the body to obtain a closer view of work. For a cardiac surgeon, the correct position of the body is essential, as operating hours are long, standing for hours altogether with antigravity muscles, extreme degree of bimanual dexterity, bleeding suture lines, failing hemodynamics, and concentration seeking meticulous procedures with tilted head in the FOV through a loupe can be strenuous. Among these factors, the ergonomics of the body is a modifiable factor. The loop declination angle is intended to measure how well loupes help the user look downward. The greater the declination angle, the less the surgeon must tilt his head. A literature search showed that continually tilting the head >25° forward can cause discomfort, chronic pain, and even career-ending injury. Loupe ergonomics of the body are determined by two major inputs for customization: the WD and the declination angle needed to avoid chronic pain and injury due to persistent head tilt.
ACCESSORIES AND ADVANCES
There are a lot of companies manufacturing high-standard loupes across the globe such as Carl Zeiss AG (German), Keeler, Design for Vision, Inc. (American), Doctor Scope (Korean), and many others that customize the loupes for surgeons.
Fogging of the lens is a big problem for surgeons; it interferes with the operating field, particularly when the nose is partially covered with the mask. To overcome this, loupes are available with silicon eyecup, which covers the eye, exhaled air does not come in contact with the loupe lens. This silicon eyecup also protects from spilled contaminated body fluids
Nowadays, loupes are available with frame-mounted light sources along with high-resolution cameras. Bluetooth-enabled wireless foot-pedals are available for hands-free recording, with sensors to reduce auto exposure and bloom in bright light
Loupes with panoramic views offer a larger FOV, incorporating multiple lens systems with complex optics. The FOV of a classic ×3.5 magnification is 8 cm, with a panoramic design it is 11.1 × 9 cm; the FOV of a ×4.5 magnification is 5.5 cm, with a panoramic design, it is 9 × 7 cm (Design for Vision, Inc.)
Heavy lens system renders the scars over the nasal bridge if the loupes when worn for a longer time. Lens manufacturers miniaturize the hardware to reduce the weight of the loupes and overcome the problem. The average weight of the loupe is 108 g, the light source is 14 g, and the 4 K camera weighs is 32 g (Design for Vision, Inc.).
CONCLUSION
Although different types of loupes are available on the market at different prices that are manufactured by different companies, it is ultimately the surgeon’s choice and what suits his ergonomics. The cost of the loupes (Design for Vision, Inc.) for a trainee surgeon ranges from 3000 USD (×2.5 magnification) to 4700 USD (×4.5 magnification). For any cardiac surgeon, a loupe is such an ornament that most of the surgeons are very passionate while shopping for it. In some situations, such as coronary button harvest and anastomosis of the coronary button to neo-aorta in arterial switch operation; when internal mammary artery intima is dissected while doing graft anastomosis to target vessel in coronary bypass, magnification is of utmost importance; when cardiac surgeon wears a loupe, time becomes infinity; their mediation in the surgery is indispensable. The authors want to conclude this discussion with the words of Dr. Julius H Jacobson, as said at the Annual Meeting of the Northeastern Society of Plastic and Reconstructive Surgeons, Washington, DC, in November 2005 “The eye could not see to tell the hand what to do or, to put it another way, a small error in an aortic anastomosis was of no significance but the same error in a small artery would account for failure.”
Acknowledgments
The authors want to thank Mr. PK. Pandey and Mr. Dev, Loupe specialists, for providing valuable information on Loupes and their optics.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Operating Microscopes: Past, Present, and Future. Neurosurg Focus. 2009;27:E4.
- [CrossRef] [PubMed] [Google Scholar]
- Founder's Lecture in Plastic Surgery. Ann Plast Surg. 2006;56:471-4.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary Arterial Bypass Grafts. Ann Thorac Surg. 1968;5:443-50.
- [CrossRef] [PubMed] [Google Scholar]
- A Practical Guide to Surgical Loupes. J Hand Surg Am. 1997;22:967-74.
- [CrossRef] [PubMed] [Google Scholar]
- Landmarks in the Development of Coronary Artery Bypass Surgery. Circulation. 1998;98:466-78.
- [CrossRef] [PubMed] [Google Scholar]
- Dental Magnification Loupes: An Update of the Evidence. J Contemp Dent Pract. 2021;22:310-5.
- [CrossRef] [PubMed] [Google Scholar]
- Key Factors for Ordering Custom Loupes: Part 1. SurgiTel. 2014. General Scientific Corporation. Available from: https://www.surgitel.com/key-factors-for-ordering-custom-loupes-part-1-declination-angle-as-the-key-ergonomic-factor [Last accessed on 2024 Jan 06]
- [Google Scholar]
- USA Medical and Surgical Supplies. Available from: https://www.usamedicalsurgical.com/blog/10-features-consider-buying-surgical-loupes-operating-theater [Last accessed on 2024 Jan 06]
- [Google Scholar]





