Translate this page into:
Blood and Bleeding Management in Developing Economies: Perceptions, Preparedness, and the Evolving Practices
*Corresponding author: Dr. Ajay Gandhi, Associate Clinical Director, India and South Asia, Werfen. drgandhiajay@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Mishra AK, Agarwal AK, Gandhi A. Blood and Bleeding Management in Developing Economies: Perceptions, Preparedness, and the Evolving Practices. J Card Crit Care TSS. 2024;8:33-8. doi: 10.25259/JCCC_24S1_AG1
Abstract
Objectives:
The growing concerns around the judicious use of blood components have paved the way for the dissemination of awareness around the best practices related to the use of this precious resource. With the World Health Organization issuing a policy brief on the urgent implementation of Patient Blood Management (PBM), there has been an accelerated impetus within the healthcare ecosystem to imbibe and implement the principles and practices of PBM. This research work aims to understand the current level of understanding, adequacy, and appropriateness of practices and readiness toward the universal and standardized implementation of PBM.
Approach:
This article summarizes the findings of an online survey. The survey consisted of a Google Form questionnaire with responses in multiple-choice, open and closed ends, as well as short notes. The survey responses were analyzed and summed up graphically. The survey established that there is still a huge gap in the “multispecialty approach” to setting up of the safe tolerance limits to anemia, optimal cutoffs, and thresholds for transfusion and shifting focus from “blood product” safety to “patient” safety.
Conclusion:
A lot of guidance- and evidence-based recommendations on transfusion practices are available in developed economies; the developing world still continues to weigh the advantages against the availability of and access to resources needed for implementation. Within these economies, and among different strata of healthcare infrastructure, there is still a significant difference in the perceptions and practices around blood transfusion and bleeding management.
Keywords
Patient Blood Management
Awareness
Perception
Implementation
Challenges
INTRODUCTION
Blood transfusion is one of the most common procedures that are performed during hospitalization, and it is equally common among most age groups.[1] Blood may be transfused as either whole blood or its components. However, since the patient generally does not require all the components of blood, usually, the blood components are required and transfused in the patient for different and specific conditions or diseases.
Several governing bodies such as the World Health Organization (WHO), International Society of Blood Transfusion, National Aids Control Organization (NACO), and Ministry of Health and Family Welfare (MoHFW) manages and regulates the policies and procedures adopted by blood banks to ensure blood product safety.
Blood product safety has been an ever-engaging area of focus for most of the healthcare communities,[2] including policymakers and implementing healthcare professionals over the past few decades. There are various modes and means adopted to reduce the risk of blood transfusions and improve blood product safety. There are multiple effective interventions in every step of the process, ranging from the pre blood donation stage to the post-procedure follow-up of blood product recipients. This also includes improvements in the collection, storage, management, distribution, utilization, and monitoring of transfusions. Patient safety with blood product administration using wireless and bar-coded technology is one of the innovative attributes of ensuring blood product safety. Most of the guidance and recommendations,[3] including authentic handbooks, recommend modus operandi and best practices around safe blood. These guidance documents have also focused on safe transfusion, which is the right blood, right patient, right time, and right place, but not to the extent as much as that for safe blood. However, the evolving knowledge and practices have laid the foundation for adopting, implementing, and establishing novel and evidence-based standards of care like patient blood management (PBM).
There are several organizations and associations that have included PBM either within the scope of their objectives and campaigns or are completely dedicated to the subject matter. Society for Advancement of Blood Management, Network for Advancement of PBM, Hemostasis, and Thrombosis, and International Forum for PBM are the bodies that deal exclusively with issues related to PBM.
PBM is a multimodal, multidisciplinary approach adopted to limit the use and the need for allogeneic blood transfusion in all at-risk patients with the aim of improving their clinical outcomes. Although PBM usually refers to surgical patients, its clinical use has gradually evolved over the past few years. PBM is a compelling need for the healthcare ecosystem, particularly in developing countries, where anemia is common and blood continues to remain a scarce resource. Although there is a growing level of advocacy toward PBM in terms of evidence, as a concept, in terms of policy and practice, it continues to find avenues to establish itself.
APPROACH
This article primarily sums up the responses obtained from the online survey in the form of a Google Form questionnaire sent to healthcare professionals practicing in relevant clinical settings (transfusion medicine, surgery, obstetrics, transplants, anesthesiology, critical care, etc.). The responses were analyzed vis-à-vis available evidence around the current level of understanding, adequacy, and appropriateness of practices and readiness toward the universal and standardized implementation of PBM. The responses were then depicted in pie charts and other pictorial art forms to give a visual representation of the stratification.
Blood transfusion
Blood transfusion, dating from the early 1900s, evolved into large-scale blood transfusions during the Second World War.[4] Eventually, after the war “blood save lives” became a common phenomenon and was accepted by all. Blood transfusions were hence considered safe and introduced in all forms of surgeries. With not much data or evidence to prove otherwise, blood transfusions were considered an inherent part of medicine and surgery across the globe. The practice of blood transfusion became increasingly sophisticated, standardized, and supervised in due course of time. Transfusion medicine developed as a branch of medicine to encompass the science, principles, and practices related to the transfusion of blood and blood components, including hemovigilance.
Blood and blood safety
The uprising of acquired immunodeficiency syndrome gathered the attention of all policymakers and subsequently shifted the focus on the “safety” of blood products.[5] The issues of immunocompatibility and transfusion-related adverse reactions further enforced the actions to ensure blood product safety. It would not be an exaggeration to say that transfusion medicine, as a subject, has evolved significantly but continues to focus on the “utilization” and “safety” of the product but nothing much with respect to the implications of blood transfusions for patients in terms of blood transfusion safety. Most (57%) respondents felt that blood banking, as an entity, focuses primarily on the blood product per se [Figure 1].
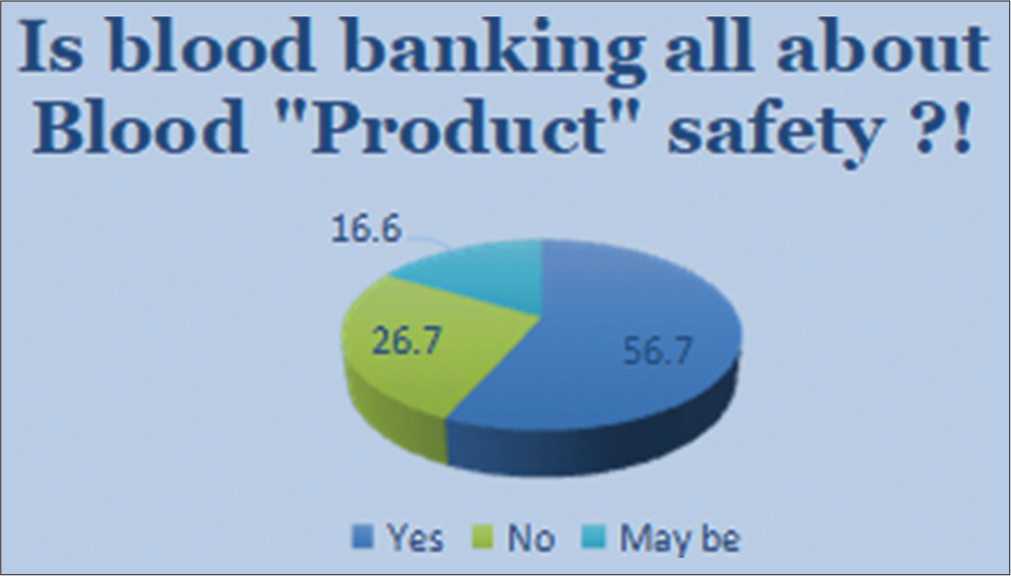
- Survey response – Is blood product safety all about the focus of blood banking?
Blood as a resource: Access and availability
One of the major limitations of blood and its products, which remain almost true to date, is that it cannot be artificially manufactured in factories. It must be obtained from a healthy and, preferably, non-related voluntary donor. To meet this requirement, several global and regional drives have been conducted in the past and continue to dominate the circles of awareness and academia around blood transfusion. There are more than 3000 blood banks in India, out of which almost half are supported by NACO, MoHFW, and Government of India. The requirement of blood for the country is estimated to be 8.5–10 million units/year, whereas the available supply is only 7.4 million units/year. This is a clear indication that there is an immanent demand-supply mismatch. This also denotes that the available blood must be subjected to standardized and judicious practices so as to eliminate even the slightest possibility of irrational or inappropriate use.
While almost all blood banks have a practice of encouraging voluntary blood donation, most could only meet the requirements from combined voluntary and replacement blood donation [Figure 2]. The impetus of all the governing bodies has been to promote complete reliance on voluntary blood donation, but it appears that the majority of blood banks depend on replacement blood donors to fulfill the demands and that too not cent percent. This is a very critical situation considering not only the extent of efforts that the blood banks and the regulatory bodies make in ensuring uninterrupted blood supply vis-à-vis blood demand but also the significant amount of inconvenience that the family members or attendants of the patients have to face when arranging for blood requirements. To confound the situation further is the fact that not every blood bank is capable of producing or providing blood components as required by the ordering physician or surgeon. This is probably the most conspicuous reason for a significant gap in the demand and supply of blood.
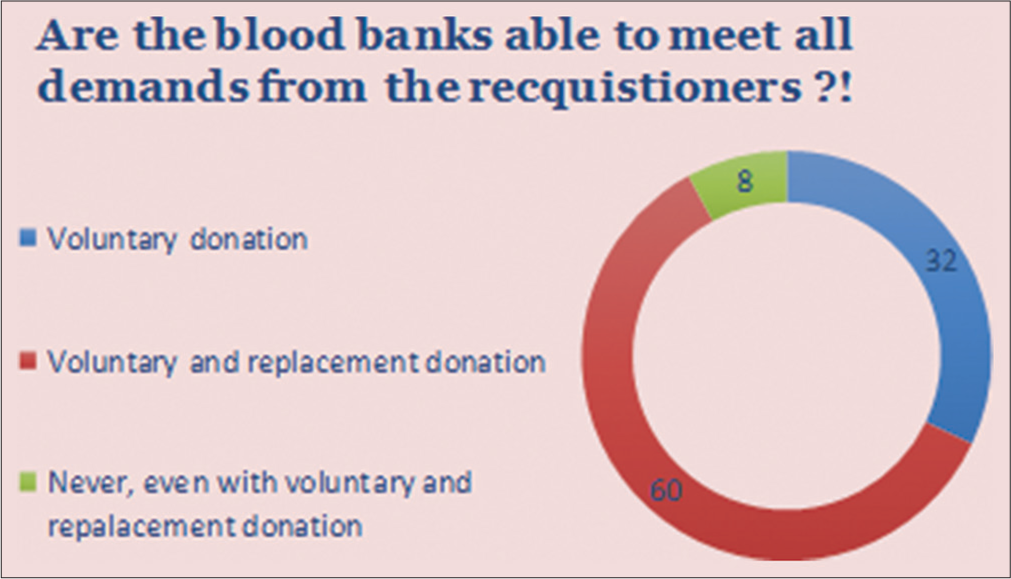
- Survey response – Meeting the blood requirement.
Rational use of blood
With the availability of blood and blood components and the formulation of habits and behavior around their usage, there has been an anticipated development of protocols and guidelines. The WHO recommends safe and rational use of blood to reduce unnecessary and unsafe transfusions. Every time a decision to transfuse is made, everyone involved in the blood bank and in the transfusion process is responsible and accountable for the rational transfusion of safe blood products. However, the challenge of finding both infrastructure and orientation to be present in the same place continues to remain a key problem in ensuring the best practices with respect to blood transfusion.
It was a little surprising to note that a very limited number of respondents believed that the blood transfusion practices around them were rational or judicious, based on guidelines and protocols [Figure 3]. The most common attribute of these transfusion practices was “empirical” transfusion, that is, not driven or guided by scientific evidence. Another revelation was that many centers still cater to blood transfusion requirements, which are ordered for correction of laboratory values, namely, hemoglobin, prothrombin time/international normalized ratio, and platelet count.
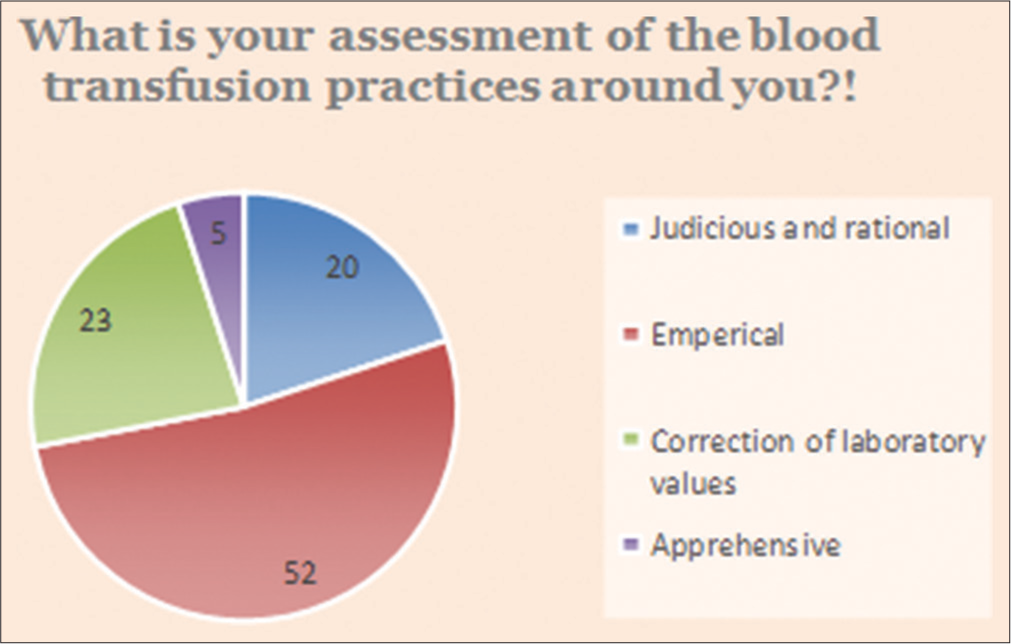
- Survey response – Assessment of current transfusion practices.
Blood safety to patient safety: The shifting focus
Advancements in technology for blood testing over the years and much emphasis on donor screening have reduced transfusion-related adverse events, especially the transmission of infectious agents; however, noninfectious complications continue to be a serious risk. The noninfectious transfusion-related adverse events[6] may happen due to various reasons specific to a blood component, amount of blood transfused, and error on the part of decision making toward transfusion. The increasing number of issues and evidence on complications of transfusions, per se, has functioned as the activator of shifting the focus toward the “patient” rather than the “product.”
PBM: The paradigm change
PBM[7] is a patient-centered, systematic, and evidence-based approach to improve patient outcomes by managing and preserving a patient’s blood while promoting patient safety and empowerment. PBM involves the timely, multidisciplinary application of evidence-based medical and surgical concepts aimed at (1) screening for, diagnosing, and appropriately treating anemia; (2) minimizing surgical, procedural, and iatrogenic blood losses and managing coagulopathic bleeding throughout the care; and (3) supporting the patient while appropriate treatment is initiated.
Although not a positive observation, it was not surprising to see that most respondents still believed that PBM is all about the optimal use of blood [Figure 4]. Another fair subset of participants believed that it revolves around innovation and technology, including point-of-care testing.
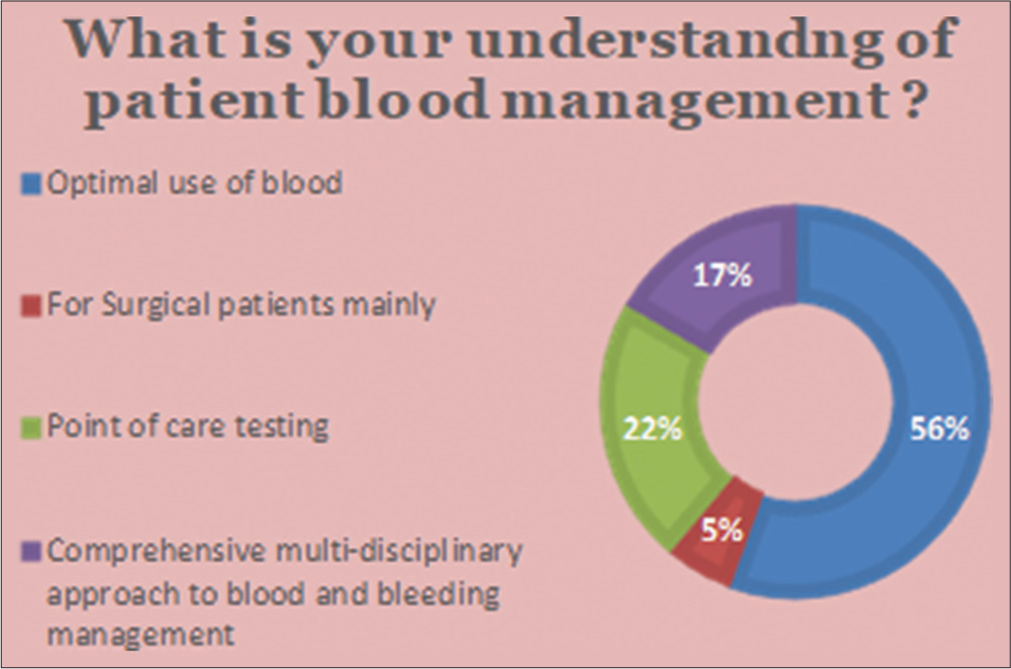
- Survey response – Perception of the concept of patient blood management.
There are several reasons[8] to shift from product-centered transfusion practice to patient-centered PBM – the aging population that has a worked-out demand for blood products as against the reducing donor base; the increasing “consumer” awareness that transfusion is a complicated service involving several different cost centers within a healthcare institution and amounting to a multiple of the blood product cost; the ongoing efforts to protect blood banking systems from existing, evolving, or altered pathogens; the emerging global evidence that blood transfusion is an independent risk factor for adverse outcomes; and a paucity of concrete evidence toward benefits of transfusion for a vast majority of transfusion recipients.
PBM improves patient outcomes by improving the patient’s medical and surgical management in ways that boost and conserve the patient’s blood.
Challenges to attain and sustain PBM
Anemia is one of the most widely prevalent conditions in most developing countries like India, and this is equally prevalent among the donors as well as recipients.[9] When a patient requires blood transfusion, the quality and quantity of blood components, especially the clotting factors, hematocrit, and platelets, are determined by a lot of factors that are not just inherent to the donor but also distributed amongst the donor-patient population. Although the stringent criteria on voluntary blood donation ensures at least a fair presence of these vital constituents, not every time a matched blood unit is available or, especially in emergency situations, a voluntarily donated blood unit is available. Despite several global and locally available protocols, anemia is inappropriately managed ahead of a decision to make a blood transfusion. This confounds the possibility of providing an effective blood transfusion and, hence, is a significant deterrent to the objective of the first pillar of PBM, which is optimizing the red cell mass. Shockingly, almost all centers still resort to preoperative correction of anemia using blood (packed red cells), and the use of parenteral iron to correct anemia before any surgical procedure is seen mostly in the tertiary or referral centers [Figure 5].
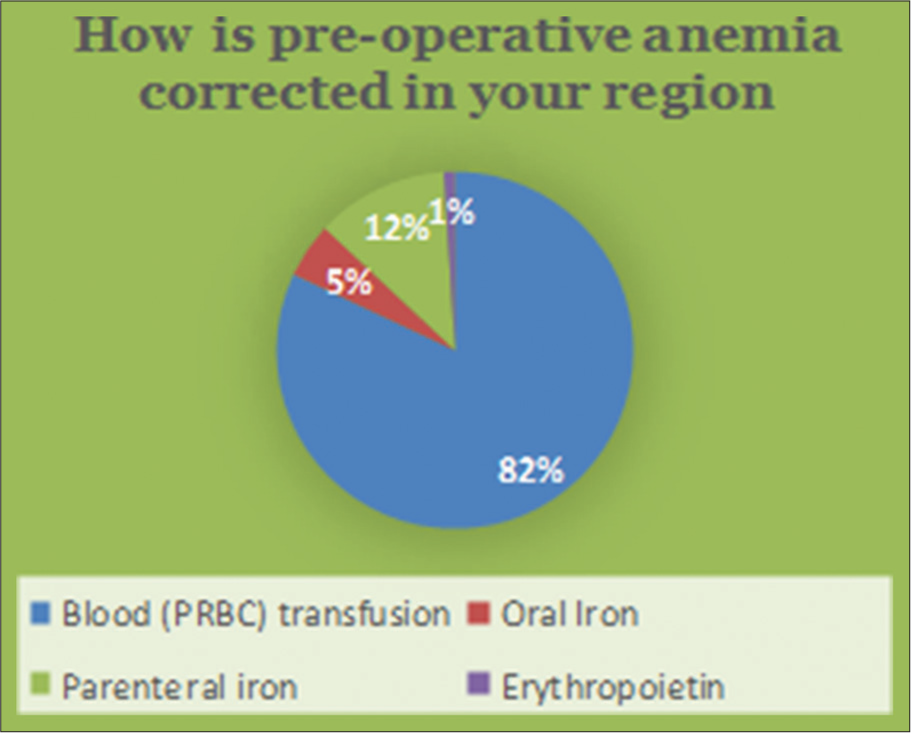
- Survey response – Practice of preoperative anemia management.
In a developing country like India, again, with limited resources and poor availability of and access to healthcare facilities, dealing with any massive hemorrhage is a major challenge. This challenge gets compounded by pre-existing anemia, hemostatic disorders, and logistic issues of timely transfer of such patients from peripheral hospitals to centers with adequate resources and management expertise.[10] Particularly in acute settings such as perioperative bleeding or complex bleeding situations like trauma and obstetric hemorrhage (mostly post-partum), there is a major challenge in terms of identifying the exact cause of bleeding, assessing the exact requirement of type and volume of blood components, and/or pharmacologic agent, and the intensity of time constraints. Most of the respondents ascribed the lack of resources, relevance on conventional tools and modalities, and absence of pertinent (regional) guidance [Figure 6].
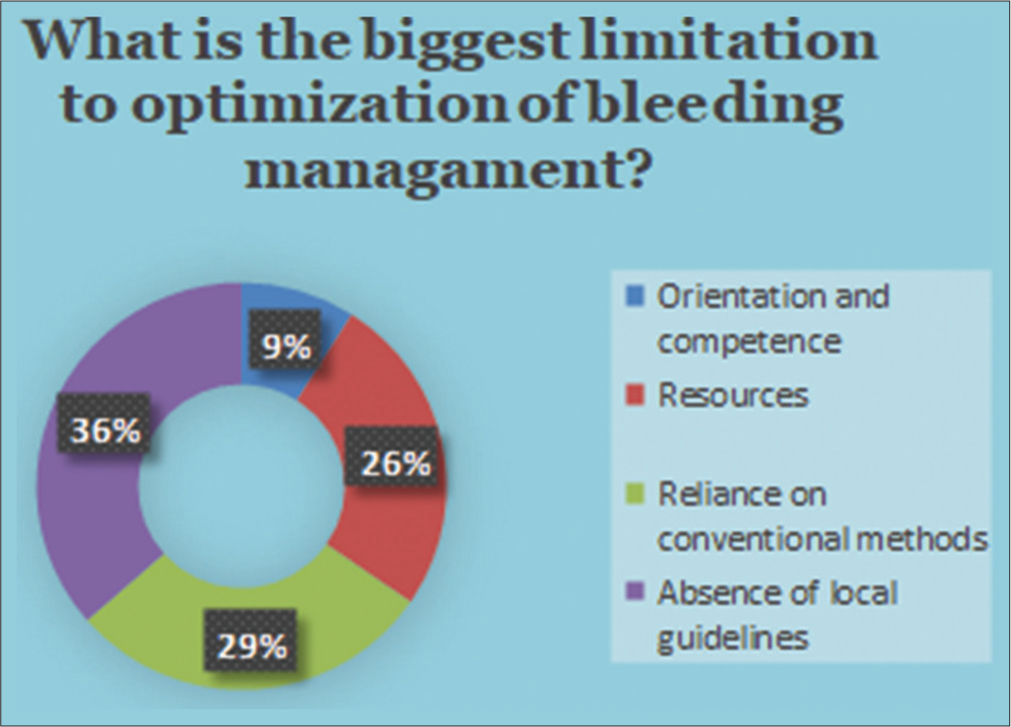
- Survey response – Limitations to optimal bleeding management.
A decision to transfuse often lacks a thorough discussion between the physician, blood transfusion specialist, and other clinical services to ensure effective and patient-safe transfusion practices. Often, the thresholds or triggers toward transfusion are based on subjective or perceived interpretation of the patient’s laboratory values alone rather than their implications with respect to the patient’s hemodynamic status and other vital parameters. This poses a significant challenge to address the third pillar of PBM.
All these factors were equally highlighted as background reasons for irrational transfusions by the respondents [Figure 7].
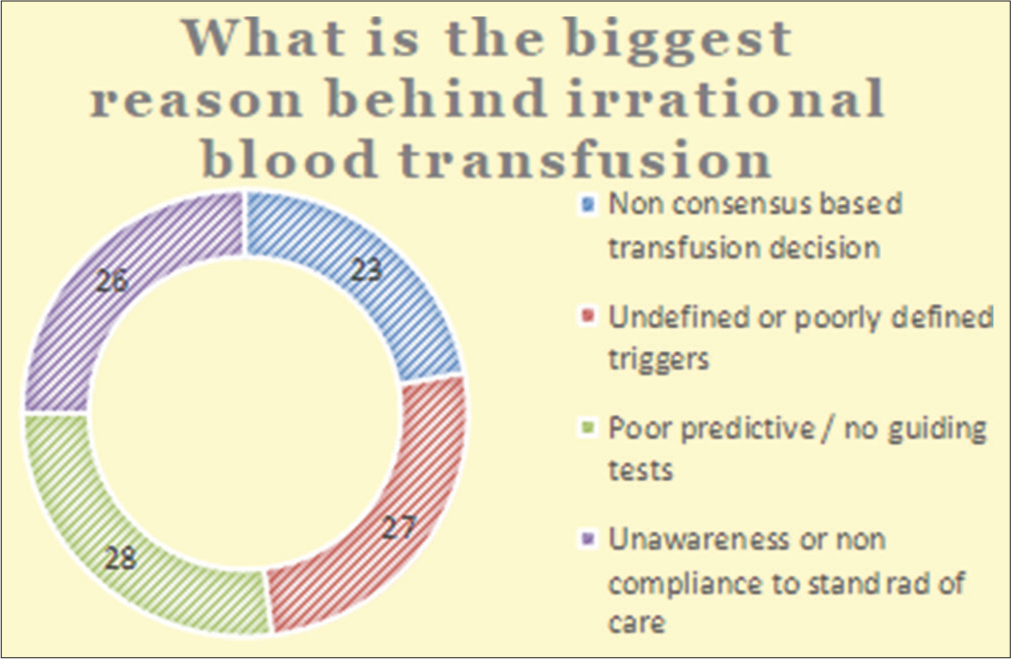
- Survey response – Analysis of factors contributing to irrational transfusion.
Health economics: Selective ignorance
In developing economies, especially where the cost of healthcare is usually borne not by the government or the insurer but by the patients themselves, there is a widely skewed consideration toward the cost of blood transfusion which is often calculated only in terms of blood product acquisition and cost of transfusion consumables. There is, still, not much consideration offered toward complications inflicted as a result of irrational transfusion, thereby undermining the role of potentially preventable complications of injudicious blood transfusion.
CONCLUSION
There is a wide demand-supply gap for blood in developing countries like India. The gap emphasizes the need for sustained and concerted efforts from all stakeholders. The gap not only denotes increased efforts toward making complete universal voluntary blood donation as the only source to meet all the blood requirements but also a pressing need to adopt means and modes of ensuring optimal utilization of blood, optimizing the availability of blood components through efficient blood component separation units, promoting modern principles of PBM, and strengthening capacities of human resources in the blood transfusion system in India.
Blood is not just a very scarce resource but also could do much more harm than benefits. The complications of blood transfusion per se need to be considered and followed up so as to ensure a proper audit of every blood transfusion recipient. The focus should also be on safe transfusion, positively influencing maximum lives apart from ensuring safe blood practices are being followed all across so far.
Transfusion committees, often a very important functional unit to ensure safe and judicious blood transfusion, should be replaced by PBM committees, to additionally incorporate all relevant stakeholders as well as address the decision to transfuse as a conscious, calculated, communicative, and consensual activity.
PBM is an evidence-based practice that should be implemented and regulated as the standard of care. Policymakers and administrators should ensure universal and standardized implementation starting right from the grassroots level of healthcare facilities. This should include the inclusion of PBM as a subject matter within the health education curriculum, setting up of anemia clinics, bleeding management competence build-up, enhancement of infrastructure needed toward coagulopathy evaluation, and management and national guidelines and recommendations on effective and patient-centric use of precious resource blood.
In an era when the patient is also believed to be a consumer, every decision to transfuse must be treated beyond informed consent through proactive and inclusive communication, collaboration, and consensus of all stakeholders, including the patient and/or his attendants.
The growing awareness and campaigns on best practices around blood transfusion should clearly establish PBM as the standard of care above and beyond just the optimal use of blood.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
Authors AM and AG were employed by the company Werfen. The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Demographic and Epidemiologic Characterization of Transfusion Recipients from four US Regions: Evidence from the REDS-III Recipient Database. Transfusion. 2017;57:2903-13.
- [CrossRef] [PubMed] [Google Scholar]
- Blood Product Safety In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023.
- [Google Scholar]
- The Administration of Blood Components: A British Society for Haematology Guideline. Transfus Med. 2018;28:3-21.
- [CrossRef] [PubMed] [Google Scholar]
- The History of Blood Transfusion Prior to the 20th Century--Part 1. Transfus Med. 2012;22:308-14.
- [CrossRef] [Google Scholar]
- History of the Controversy In: HIV and the Blood Supply: An Analysis of Crisis Decisionmaking. Washington, DC: National Academies Press (US); 1995. p. :3. Available from: https://www.ncbi.nlm.nih.gov/books/NBK232419 [Last accessed on 2023 Dec 13]
- [Google Scholar]
- Noninfectious Transfusion-Associated Adverse Events and Their Mitigation Strategies. Blood. 2019;133:1831-9.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management: A Revolutionary Approach to Transfusion Medicine. Blood Transfus. 2019;17:191-5.
- [Google Scholar]
- Five Drivers Shifting the Paradigm from Product-Focused Transfusion Practice to Patient Blood Management. Oncologist. 2011;16(Suppl 3):3-11.
- [CrossRef] [PubMed] [Google Scholar]
- Donor Deferral due to Anemia: A Tertiary Care Center-Based Study. Asian J Transfus Sci. 2011;5:53-5.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Blood Management in India-Review of Current Practices and Feasibility of Applying Appropriate Standard of Care Guidelines. A Position Paper by An Interdisciplinary Expert Group. J Anaesthesiol Clin Pharmacol. 2021;37:3-13.
- [CrossRef] [PubMed] [Google Scholar]







