Translate this page into:
Inhaled Milrinone via HFNC as a Postextubation Cardiopulmonary Elixir: Case Series and Review of Literature
ItiShri, MD Department of Cardiac Anaesthesia, Atal Bihari Vajpayee Institute of Medical Sciences (ABVIMS) and Dr. Ram Manohar Lohia Hospital Baba Kharak Singh Marg, New Delhi 110001 India iti.anesthesia@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pulmonary hypertension (PH) often complicates perioperative course following pediatric cardiac surgery, often presenting unique challenges to the attending cardiac anesthesiologist. Apart from difficult weaning from cardiopulmonary bypass, PH can often compound weaning from mechanical ventilation in this postoperative subset. From pathophysiological standpoint, the former can be attributed to concurrent detrimental cardiopulmonary consequences of PH as a multisystemic syndrome. Therefore, with an objective to address the affected systems, that is, cardiac and pulmonary simultaneously, we report combined use of inhaled milrinone (a pulmonary vasodilator) through high-frequency nasal cannula (oxygen reservoir and continuous positive airway pressure delivery device), purported to complement each other's mechanism of action in the management of PH, thereby hastening postoperative recovery. The article additionally presents a nuanced perspective on the advantages of combining the aforementioned therapies and hence proposing the same as a possible “postoperative cardiopulmonary elixir.”
Keywords
cardiopulmonary elixir
inhaled milrinone via HFNC
postextubation
Background
Pulmonary hypertension (PH) due to congenital heart disease (CHD) manifests either secondary to pulmonary vasculature remodeling consequent to increased pulmonary blood flow or postcapillary elevation of pulmonary venous pressure in left-sided obstructive lesions. Ventricular septal defect (VSD) is the most common underlying CHD (42%) predisposing to PH with risks of PH persisting even after surgical management of the defect.1 Notably so, PH after surgically repaired CHD is associated with worse outcomes compared with other etiologies of PH.2
Moreover, the present day perioperative cardiac surgical challenges have only been intensified considering increasing number of patients presenting for surgical intervention post-coronavirus disease 2019 (COVID-19) infection because of its long-term ill effects and multiorgan involvement. In this context, COVID-19 infection may exacerbate and escalate PH secondary to CHD.3
Perioperative PH can peculiarly lead to a protracted intensive care unit (ICU) stay with enhanced morbidity and mortality owing to its perilous cardiopulmonary effects.2 Therefore, the current strategies to treat PH focus on pharmacological agents that may unload right ventricle while maintaining systemic pressures as well as applying cardiopulmonary protective ventilatory approach.4
In this background, we report a series of six pediatric PH predisposed cardiac surgical cohort who were administered inhaled milrinone (iMil), a pulmonary vasodilator via high-frequency nasal cannula (HFNC) postextubation, with an aim to avert residual PH-associated cardiopulmonary repercussion, thereby expediting ICU recovery and discharge. Furthermore, the article reviews role of iMil, HFNC, and combination thereof in alleviating deleterious cardiopulmonary interactions in PH.
Case Series
Cases 1 to 3 (Postoperative PH Predisposed CHD)
A 3-year-old child with a nonrestrictive VSD sized 1.4 cm with pulmonary vascular resistance index (PVRI) of 7 Woods Units/m2 and positive vasoreactivity was posted for surgical closure. After a successful weaning from cardiopulmonary bypass (CPB), the patient desaturated. Despite recruitment, suctioning, and application of positive end-expiratory pressure (PEEP), he continued to desaturate. On needle transduction, pulmonary artery pressure (PAP) was more than systemic pressures. Therefore, iMil was started, followed by inhaled nitric oxide (iNO) at 10 to 15 parts per million (ppm) due to nonresponse to intravenous therapy. The patient was stabilized and continued on iNO that was gradually tapered, and once the patient met extubation criteria, he was extubated. Considering a possibility of residual PH owing to CHD-induced pulmonary vascular remodeling as well as phenomenon of rebound PH following iNO discontinuation, milrinone was nebulized via HFNC and continued for 8 hours not only to ensure smooth weaning from ventilator but also to cover for the lag in time till oral vasodilator therapy could have become effective. Throughout the 2 L/kg/min of HFNC therapy, the child maintained acceptable partial pressure of arterial oxygen (PaO2) and stable hemodynamics. Subsequently, the patient could be shifted to a step-down facility from the ICU.
Likewise, in another child with large unrestrictive VSD, after successful weaning from CPB, the patient was unable to maintain saturation. He was managed on iMil initially. However, a fall in his platelet count prompted resort to nebulized milrinone therapy via HFNC, postextubation and a smooth weaning from ventilator was corroborated.
Similarly, a 4-month-old child of supracardiac total anomalous pulmonary venous connection with evidence of preoperative PH presented for surgical correction. He was administered sildenafil through Ryles tube pre-CPB. Weaning from CPB, however, was tumultuous and resulted in rapid desaturation along with increase in carbon dioxide levels on serial blood gas analysis. A multipronged strategy including anti-inflammatory measures, intravenous inodilators on CPB while modified ultrafiltration (MUF), iNO delivery at 10 to 15 ppm, and lung protective ventilation post-CPB was applied. To expedite postoperative recovery while avoiding detrimental cardiopulmonary effects of persistent PH, iMil was administered via HFNC. The postoperative period remained uneventful.
Cases 4 and 5 (Post-COVID-19 Sequelae)
Two-year-old and 1.7-year-old children with a previous history of COVID-19 were posted for VSD closure. Both had nonrestrictive VSD (size 1.3 and 1.6 cm, respectively), high PVRI, and positive vasoreactivity test on preoperative catheterization study. They both displayed a difficult weaning from CPB with pulmonary artery (PA) pressures reaching suprasystemic levels on needle transduction. To facilitate weaning, anti-inflammatory measures and intravenous inodilators were employed alongside MUF and iNO post-CPB. In the postoperative period, lung protective ventilation, sedation, inodilators, and iNO were continued to prevent PH crisis. Furthermore, to retrench additive adverse effects of underlying CHD pathophysiology and COVID-19-induced alveolar damage and perivascular inflammation, iMil via HFNC was initiated with the objective to counter an exacerbated predisposition to PH in view of lung damage by COVID-19 in a PH liable CHD cohort.
Case 6
A 2-year-old female child with large perimembranous VSD (1.6 cm) and a neurogenic tumor extending into the thoracic cavity compressing the posterior segment of the right upper lobe of lung, presented for surgery. Since the beginning patient had decreased air entry on right side with sustained high peak airway pressures. Following CPB, however, the child kept on desaturating, with sustained rise in peak airway pressures. Anticipating increased PAP, iNO was administered along with iMil and lung protective ventilation strategy was applied. This was continued in ICU till extubation. The postextubation period again was covered with iMil via HFNC in anticipation to tide over remanent compressive effects of tumor as well as residual PH due to shunt. Further course in ICU was unremarkable.
Discussion
PH is a progressive disorder adversely affecting both cardiac and pulmonary systems, toiling weaning both from CPB as well as ventilator. Consequent to pulmonary vascular remodeling, proliferation, and occlusion, transpiring into right heart and eventual left heart dysfunction culminating into low cardiac output syndrome. It may persist postoperatively even after successful CHD repair.2, 5, 6 Pulmonary vasculature remodeling along with enhanced pulmonary vasoreactivity, and endothelial injury due to CPB are likely contributors to persistent PH postoperatively.5 In addition, rebound PH due to negative feedback inhibition by iNO may also activate endogenous vasoconstrictors resulting in brief vasoconstriction. This may prolong mechanical ventilation, lengthen ICU stay, and enhance morbidity and mortality. In this background, typical therapy to treat PH should address the hemodynamic and ventilatory effects of the precarious cardiopulmonary liaison, with the aim to ensure smooth weaning from ventilator and eventual recovery. With this aim, we administered milrinone (a pulmonary vasodilator and inotrope that inhibits enzyme phosphodiesterase-3) via HFNC (continuously delivers continuous positive airway pressure [CPAP] with humidified oxygen at high flow rates), in the aforementioned cases immediately postextubation as to mitigate deleterious effects of residual PH as well as addressing the problem of rebound PH following iNO discontinuation.
With respect to aforesaid, Maggiore et al and Hernández et al in their respective studies highlight the role of preemptive postextubation high-flow oxygen therapy via HFNC in favorably modulating the postoperative oxygenation status and minimizing the reintubation rate, when compared with conventional oxygenation therapy.7, 8 HFNC by the virtue of providing heated and humidified gas at flow commensurate to peak flow rate generated by the patient reduces the work of breathing and fatigue, creates an oxygen reservoir in the upper airways thereby improving oxygenation and avoiding accumulation of carbon dioxide, preventing inspissation of secretions. It also splints open the airway and prevents collapse during exhalation as well thereby preventing atelectasis and acting like CPAP support. Apart from above physiological advantages, there is an increased comfort and compliance to the machine as compared with other noninvasive modes of oxygenation, and early introduction of oral feeds and medications.9
Of relevance to PH predisposed cohort, HFNC by avoiding positive pressure ventilation not only avoids pulmonary vessel compression but also circumvents hypoxic pulmonary vasoconstriction that decrescents right ventricular (RV) preload as well.10 Even from a strict cardiac perioperative perspective, Kumar et al very recently proposed role of HFNC in postoperative acyanotic CHD patients, where the authors reported improvement in postextubation partial pressure of oxygen/fraction of inspired oxygen concentration (PaO2/FiO2).11 While our patients were postoperative adult CHD patient akin to the Kumar et al study,11 the additional attributes such as a previous history of COVID-19 infection, collapsed lung lobe, intraoperative PH crisis, and recent tapering of iNO, implied an accentuated risk in our setting.3
With reference to the role of pulmonary vasodilators, the literature bespeaks the advantages of inhaled therapy over intravenous with the former being pulmonary selective, ameliorates RV function better, improves oxygenation, and reduces inflammation while avoiding associated systemic side effects.12 Literature is accruing describing additional benefits of iMil therapy in PH like attenuating CPB-induced inflammation and facilitating weaning from CPB, and improving pulmonary endothelial function. Laflamme et al found a reduction in rate of difficult separation from CPB to 51% in group receiving combined inhaled prostaglandin and iMil as compared with 70% (p = 0.1638) in the inhaled group. There was also a reduction in postoperative vasoactive requirement both at 12 hours (35.9 vs. 73.7%, p < 0.01) and 24 hours (25.6 vs. 57.9%, p < 0.05) postoperatively.13 Similarly, Haraldsson et al in their study on patients with postoperative PH found a reduction in pulmonary vascular resistance (PVR) by 20% (p < 0.001) in patients administered iMil as compared with inhaled prostacyclin, while the former accentuated the effect of latter in reducing the PVR and increasing stroke volume.14 Singh et al in their series of 35 children with acyanotic CHD,15 Patel et al in their study on 100 patients with mitral valve stenosis,16 Nguyen et al in their series of patients,17 and Sablotzki et al in 18 consecutive male heart transplant patients18 have posited the safety and efficacy of iMil in the management of PH and subsequent RV dysfunction. Lamarche et al in their porcine model have further demonstrated a decrease in heart rate and hence myocardial oxygen demand when iMil was administered to study CPB effects on pulmonary endothelium.19
As mentioned, PH is a syndrome whose treatment involves not only optimizing ventilation and oxygenation but also demands decongesting right ventricle for achieving adequate left ventricular function. Propounding the advantages of combination therapy of pulmonary vasodilator and HFNC, Tominaga et al successfully employed the delivery of iNO via HFNC for postoperative management in patients undergoing Fontan procedure.20 The authors propose, iNO via HFNC may be indicated in other conditions with postoperative PH predisposition, for example, tetralogy of Fallot with pulmonary stenosis with major aortopulmonary collaterals. Li et al administered epoprostenol through HFNC in 11 subjects with PH and/or RV dysfunction and found improved PaO2/FiO2 ratio (07.5 ± 26.3 to 125.5 ± 31.6, p = 0.026).21
Hence with the motive to address both cardiac as well as pulmonary components, we aerosolized milrinone at a rate of 0.1 μg/kg/min based on a previous study22 through HFNC (using vibrating mesh nebulizer, Aerogen Solo, Aerogen Ltd., Ireland, which is considered not to interfere with the airflow and pressures in the circuit as well as deliver very fine particles beyond larger airways),23 where in heated-humidified oxygen at slight PEEP, improves alveolar recruitment, oxygenation status, and lung compliance and avoids reintubation (Fig. 1).20

- (A) Assembly for administering inhaled milrinone (iMil) via high-frequency nasal cannula (HFNC). (B) Aerosolization of milrinone solution. (C) Calculation of dosage and volume of milrinone solution administered.
Second, liberation from positive-pressure ventilation has resultant circulatory benefits from a specific context of an elevated afterload-induced RV dysfunction, pertinent to a setting of PH.20, 24 Third, the positive cardiopulmonary liaison only strengthens in the backdrop of a selective inhalational delivery of vasodilator therapy, curtailing the systemic hypotensive effects of intravenous vasodilator (Fig. 2).20
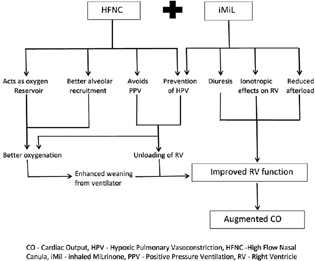
- The complementary action of inhaled milrinone (iMil) via high-frequency nasal cannula (HFNC) in alleviating after effects of postoperative pulmonary hypertension.
To the best of authors' knowledge, this article presents a unique research endeavor combining iMil and HFNC therapy harnessing the benefits of both the therapies in management of the PH syndrome and its aftereffects. The article reprises the continued oxygenation, reduced work of breathing, RV unloading, and a simultaneous improved left ventricular function leading to smooth weaning from ventilator and recovery, as a result of administration of aerosolized milrinone through HFNC, a combination complementing each other's mechanism of action to treat PH. The article also adequately reiterates that COVID-19 superadded infection in patients already predisposed or suffering from PH, notoriously perpetuates PH by worsening lung parenchymal inflammation and injury,25, 26 and PA obstruction, as evident by cases 3 and 4 who were acyanotic CHD post-COVD-19 infection status and exhibited turbulent CPB as well as ventilator weaning requiring meticulous pulmonary vasodilator therapy as well as ventilation-sedation strategy. Here in the role of iMil as well as HFNC has adequately been elucidated in curbing COVID-19 detrimental effects on oxygenation and RV function.27 Lastly, transnasal aerosol delivery is particularly preferable for small children in view of comfort and better tolerance.28
Conclusion
The projection of prophylactic iMil administration via HFNC in PH predisposed cohort, as to ensure smooth recovery postextubation, in the above case series is remarkable enough to motivate the fraternity to explore the promises of a combination therapy of iMil and HFNC, as a postextubation cardiopulmonary elixir in peculiarly predisposed perioperative settings, in future large-scale research endeavors.
Conflict of Interest
None declared.
References
- Pulmonary hypertension in congenital heart disease. Future Cardiol. 2018;14(4):343-353.
- [Google Scholar]
- Residual pulmonary hypertension more than 20 years after repair of shunt lesions. Medicina (Kaunas). 2020;56(6):297.
- [Google Scholar]
- Postoperative pulmonary hypertension: etiology and treatment of a dangerous complication. Respir Care. 2009;54(7):958-968.
- [Google Scholar]
- Residual pulmonary hypertension after pulmonary endarterectomy: a meta-analysis. J Thorac Cardiovasc Surg. 2018;156(3):1275-1287.
- [Google Scholar]
- Pulmonary hypertension associated with postoperative tetralogy of Fallot.Molecular Mechanism of Congenital Heart Disease and Pulmonary Hypertension. Singapore: Springer; 2020. In: eds.
- [Google Scholar]
- Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med. 2014;190(3):282-288.
- [Google Scholar]
- Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315(13):1354-1361.
- [Google Scholar]
- High Flow Nasal Cannula. [Updated 2022 May 10]StatPearls [Internet] Treasure Island, FL: StatPearls Publishing; 2022. In:
- [Google Scholar]
- Advanced airway management and respiratory care in decompensated pulmonary hypertension. Heart Fail Rev. 2021;2:1-11.
- [Google Scholar]
- Comparative evaluation of high-flow nasal cannula oxygenation vs nasal intermittent ventilation in postoperative paediatric patients operated for acyanotic congenital cardiac defects. Med J Armed Forces India. 2022;78(4):454-462. [ahead of print, September 23]
- [Google Scholar]
- Preliminary experience with combined inhaled milrinone and prostacyclin in cardiac surgical patients with pulmonary hypertension. J Cardiothorac Vasc Anesth. 2015;29(1):38-45.
- [Google Scholar]
- The additive pulmonary vasodilatory effects of inhaled prostacyclin and inhaled milrinone in postcardiac surgical patients with pulmonary hypertension. Anesth Analg. 2001;93(6):1439-1445.
- [Google Scholar]
- Inhaled nitroglycerin versus inhaled milrinone in children with congenital heart disease suffering from pulmonary artery hypertension. J Cardiothorac Vasc Anesth. 2010;24(5):797-801.
- [Google Scholar]
- Inhaled versus intravenous milrinone in mitral stenosis with pulmonary hypertension. Asian Cardiovasc Thorac Ann. 2021;29(3):170-178.
- [Google Scholar]
- Inhaled milrinone in cardiac surgical patients: a pilot randomized controlled trial of jet vs. mesh nebulization. Sci Rep. 2020;10(1):2069.
- [Google Scholar]
- Selective pulmonary vasodilation with inhaled aerosolized milrinone in heart transplant candidates. Can J Anaesth. 2005;52(10):1076-1082.
- [Google Scholar]
- Inhaled but not intravenous milrinone prevents pulmonary endothelial dysfunction after cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2005;130(1):83-92.
- [Google Scholar]
- Post-extubation inhaled nitric oxide therapy via high-flow nasal cannula after Fontan procedure. Pediatr Cardiol. 2019;40(5):1064-1071.
- [Google Scholar]
- Epoprostenol delivered via high flow nasal cannula for ICU subjects with severe hypoxemia comorbid with pulmonary hypertension or right heart dysfunction. Pharmaceutics. 2019;11(6):281.
- [Google Scholar]
- Preliminary experience with inhaled milrinone in cardiac surgery. Eur J Cardiothorac Surg. 2007;31(6):1081-1087.
- [Google Scholar]
- Vibrating mesh nebulisers – can greater drug delivery to the airways and lungs improve respiratory outcomes? Eur Respir Pulmonary Dis. 2018;4(1):33-43.
- [Google Scholar]
- Cardiovascular effects of mechanical ventilation. Crit Care Resusc. 1999;1(4):388-399.
- [Google Scholar]
- Evidence of pulmonary hypertension after SARS-CoV-2 infection in subjects without previous significant cardiovascular pathology. J Clin Med. 2021;10(2):199.
- [Google Scholar]
- Pulmonary hypertension and COVID-19. Hamostaseologie. 2021;••• Epub ahead of print
- [CrossRef] [Google Scholar]
- Improved oxygenation with inhaled milrinone in mechanically ventilated patients with severe COVID-19. Br J Anaesth. 2021;127(3):e111-e113.
- [Google Scholar]
- Narrative review of practical aspects of aerosol delivery via high-flow nasal cannula. Ann Transl Med. 2021;9(7):590.
- [Google Scholar]







